How to Identify Diabetes Distress or Burnout – Interview with Coach Beverly
What is Diabetes Distress?

At some point, almost everyone with diabetes will experience a degree of diabetes distress. It’s expected and completely understandable, especially for those on intensive medication and insulin regimens. Having diabetes is not just about checking blood sugars, counting carbs, taking medications, and giving insulin. People also have an emotional relationship with their diabetes. These feelings around their diabetes can fluctuate throughout their lifetime.
Sometimes a person might have a great day, when their blood sugars on mostly on target, they don’t miss any of their medications and insulin, plus they made it to the gym. But the next day or week or month may feel like a complete mess, with blood sugars all over the place. These blood sugar swings are due to a variety of different reasons, many of which may be out of the person’s control.
Regardless of where a person is with their diabetes self-care, the emotions that bubble up, need to be acknowledged and recognized both by the person with diabetes and the health care provider.
When diabetes self-care all starts feeling like it’s too much or like it’s out of control, that’s when we might say a person is experiencing diabetes distress.
You can determine if a person is experiencing diabetes distress by observing self-care behaviors and asking questions. Or you can use a standardized assessment tool to determine how much distress a person is experiencing in four different areas of diabetes self-care. Please see this link to download the Diabetes Distress Scale and other psychosocial screening tools.
The four areas of Diabetes Distress include:
Emotional Distress – Feeling like they are not doing enough; like they are failing and out of control.
Physician-related distress – Provider doesn’t understand diabetes.
Interpersonal Distress – Friends and family don’t really get it, or are critical, or don’t want to hear about diabetes. Can often be co-associated with depression.
Regimen-related distress – all the daily stuff a person has to do to self-manage their diabetes. Regimen-related distress is the most common kind of diabetes distress, especially for those living with type 1 diabetes.
Health Care Professionals can take an active role in identifying Diabetes Distress
We can start by asking this question, “What is most driving you crazy about your diabetes right now?” or “How are you doing with your diabetes?” while listening carefully to their response and evaluating their degree of distress.
We can also look at self-care behaviors to identify distress:
- A person may not be giving bolus insulin before meals when they used to in the past
- They disconnect from their CGM for extended periods of time.
- A surprise elevation in their blood sugars
- Expressing feelings of anger, discouragement, or frustration.
- They may think that they are the only ones going through this, that everyone else with diabetes has it figured out, so what is wrong with them?
Sometimes diabetes distress can lead to burnout or be co-associated with burnout. Sometimes, it may be hard to tell the difference. Don’t worry about figuring out if it’s burnout or distress. What’s most important is to recognize that this person is having trouble coping and to provide active listening and help with problem-solving.
What is diabetes burnout?
Diabetes burnout is an emotional reaction that is usually more intense than diabetes distress. A person in the state of burnout is someone with diabetes who has grown tired of managing their condition, then simply ignores it for a period of time.
Sometimes I refer to burnout as taking a diabetes vacation.
This vacation might be a weekend trip, a week trip, or a long-term sabbatical. Diabetes burnout looks different for everyone. Diabetes burnout is a normal reaction to living with diabetes. I am not saying it is a good thing, or we want people to feel burned out. We want to recognize that managing diabetes is a lot of work and sometimes people just take breaks from diabetes self-management.
As health care providers, we can support people experiencing diabetes distress or burnout. According to Mark Heyman, PhD, CDCES, here is an approach he has found helpful.
- Ask how they are doing and listen for emotions or actions that indicated diabetes distress.
- Help them recognize there are 2 parts to it
- Emotional reaction – Feelings of being distressed or burned out. A person might be thinking, “If I ignore my diabetes for a while, it might go away or the distress might go away.”
- Behavioral reaction – when a person feels distressed or burned out, they might ignore the diabetes as a way to manage that stress.
- Recognize how they are feeling and reassure them that their reaction makes sense.
- Then explore if they could consider separating the emotion from the behavior.
- Yes, you feel burned out but can you still check blood sugars and give yourself insulin?”
- We can help people recognize the feeling of being burned out and encourage them to make adjustments to their self-care response, ie “I am going to manage my diabetes anyway, even though I am completely frustrated and burnt out.”
As health care professionals, we need to check in with people about their distress on a regular basis and provide support.
We need to reassure them that management of diabetes isn’t easy, but they are not alone. There are lots of other people with diabetes experiencing the same feelings.
We might say something like, “Managing diabetes is hard work, but we believe in your ability to make small changes to get to a safer place. You don’t have to move mountains; you just need to take a baby step.“
Let’s remind them, that having diabetes is like getting a job you didn’t ask for. You have to do the work of a body organ, a pancreas. that requires 24 hours a day of attention, without any pay or vacations. Sincerely focus on their successes, no matter how small, and reinforce our belief in their ability to move forward. We got this.
Special thanks for the Team from Quin for hosting this interview. To learn more about Quin, click here.
Want to learn more about this topic?
Enroll in our Level 2 | Assessing and Promoting Well-Being: From Population Health to a Person-Centered Approach Standards | 1.5 CEs
Annual Update Airs Live on December 21st at 11:30 am PST

This presentation will include the latest information on Social Determinants of health, assessment strategies, and approaches. We will explore the psychosocial issues that can discourage individuals from adopting healthier behaviors and provides strategies to identify and overcome these barriers. Life studies are used to apply theory to real-life situations. A great course for anyone in the field of diabetes education or for those looking for a new perspective on assessment and coping strategies.
Objectives:
- State strategies to assess and address social determinants of health
- Discuss health care delivery systems using a person-centered approach
- List screening tools that can help detect depression, trauma, and cognitive decline
- Describe psycho-social and emotional barriers to diabetes self-management
- Provide strategies for healthcare professionals to identify and overcome barriers to self-care
Intended Audience: A great course for healthcare professionals in the field of diabetes education looking for a straightforward explanation of identification and treatment of hyperglycemic crises.
Instructor: Beverly Thomassian RN, MPH, CDCES, BC-ADM is a working educator and a nationally recognized diabetes expert.
Enroll in our entire Level 2 – Standards of Care to join us for the below 2022 Live Webinar Updates. All courses air at 11:30 a.m. (PST)
- December 15, 2021 – Hyperglycemic Crises, DKA & HHS Standards | 1.0 CE
- December 21, 2021 – Assessing and Promoting Well-Being: From Population Health to a Person-Centered Approach Standards | 1.5 CEs
- February 3, 2022 – ADA Standards of Care | 2.0 CEs
- March 24, 2022 – Meds Management for Type 2 – 1.5 CEs
- March 29, 2022 – Lower Extremity Assessment 1.5 CEs
- April 26, 2022 – Microvascular Complications, Eye, Kidney Nerve Disease 1.5 CEs
- April 28, 2022 – Critical Assessment of Diabetes Patient 2.0 CEs
- May 10, 2022 – Cardiovascular Disease and Diabetes Standards 1.5 CEs
- May 12, 2022 – Older Adults and DIabetes 1.5 CEs
- May 17, 2022 – Tots to Teens – Diabetes Standards 1.5 CEs
- May 19, 2022 – Pregnancy and Diabetes 1.5 CEs
- May 26, 2022 – Hospital and Hyperglycemia 1.5 CEs
- July 21, 2022 – Setting up a Successful Diabetes Program 1.5 CEs
All hours earned count toward your CDCES Accreditation Information
Sign up for Diabetes Blog Bytes – we post one daily Blog Byte from Monday to Friday. And of course, Tuesday is our Question of the Week. It’s Informative and FREE! Sign up below!
[yikes-mailchimp form=”1″]The use of DES products does not guarantee the successful passage of the CDCES exam. CBDCE does not endorse any preparatory or review materials for the CDCES exam, except for those published by CBDCE.
New Treatment for Type 1 Diabetes | VX-880
Vertex Pharmaceuticals just announced preliminary results from a trial that explores a new intervention to treat type 1 diabetes. The early results are very promising.
The first person with type 1 diabetes to receive this new stem-cell derived experimental therapy, had an 91% drop in their insulin needs. The person has lived with type 1 for over 40 years. After the intervention, they not only experienced a reduction in their insulin needs, their fasting C-peptide levels went from undetectable to 280. This dramatic C-peptide increase is a clinical indicator of stem-cell therapy success and endogenous insulin secretion.
These results are exciting and offer hope for a potential new treatment approach for type 1 diabetes.
VX-880 is a stem cell derived therapy that replaces damaged beta cells with healthy transplanted insulin producing cells in clinical trials. However, these new cells are at risk for attack by the body’s immune system, so immunosuppression therapy is currently required for stem-cell transplant success.
The future goal is to create a version of this treatment that doesn’t require immunosuppressive therapy. And Vertex, the makers of VX-880 are working on creating an encapsulated islet cell program that doesn’t initiate an autoimmune attack.
For more information and clinical trials, click this link.
Resources for People Living with Type 1 Diabetes

Below is a list of helpful online resources for Type 1 Diabetes. They include sites for national organizations like the American Diabetes Association (ADA), sites for diabetes interest groups, and other participant organizations that provide helpful diabetes tips and opportunities to join online groups. Click here for a Type 1 Resource Handout to share with colleagues and people living with type 1 diabetes.
Click the links below to visit the website:
- Let’s fight Type 1 Together | American Diabetes Association (ADA)
- Mental Health Resources Directory | ADA
- Type 1 Diabetes Resources and Support | Juvenile Diabetes Research Foundation: Explore our informational guides or make a personal connection with someone experienced with type 1 diabetes (T1D). The JDRF community has you covered.
- Empowering Youth with Type 1 Diabetes |The Chris Dudley Foundation
- The National Institutes of Health Diabetes Resources | CDC
- The College Diabetes Network: Focuses Specifically on Young Adults with Diabetes | College Diabetes Network
- The Diabulimia Helpline: for Individuals Having Eating Problems
- Beyond Type 1 Diabetes
- Connected in Motion: Peer-Based Sports & Outdoor Adventures for those with Type 1 (in U.S. and Canada) | Connected In Motion
- Diatribe: Library of Online Resources, Blog & Community Forums
- Diabetes Education: At times it might seem overwhelming, but you can thrive with diabetes, and a Diabetes Care and Education Specialist can help. Includes a link to find a diabetes program near you.
Sign up for Diabetes Blog Bytes – we post one daily Blog Byte from Monday to Friday. And of course, Tuesday is our Question of the Week. It’s Informative and FREE! Sign up below!
[yikes-mailchimp form=”1″]November eNews | Diabetes Month Celebration & FREE Webinars
How is “Diabetes Remission” Really Defined?
“I just want to get rid of my diabetes”, is something I frequently hear when people are newly diagnosed with diabetes.
Can people with type 2 get rid of their diabetes? Well, not exactly, but a small percentage of people with type 2 can achieve normoglycemia, especially after metabolic surgery or significant weight loss. However, over time, blood sugars often rise again. That is why diabetes isn’t “cured” or fixed. Keep reading to learn the new standardized term and ongoing screening guidelines.
What is the right term to use when blood sugars normalize, even with type 2 diabetes?

A new consensus statement designed to answer this question was issued by the American Diabetes Association, the Endocrine Society, the European Association for the Study of Diabetes, and Diabetes UK last month.
The 12-member panel recognized that we have no standard term to describe the phenomenon of prolonged normoglycemia in people previously diagnosed with type 2 diabetes, who are not using glucose-lowering medications.
Terms like “reversal”, “resolution”, or “cure”, are frequently used to describe this phenomenon and are sometimes are associated with unsubstantiated claims.
The new standardized term is “remission”.
Diabetes remission defined – A1c< 6.5% for at least 3 months after stopping glucose-lowering pharmacotherapy. This definition holds true whether attained by lifestyle changes, metabolic surgery, or other means,
When A1c is not a reliable marker of glycemic control (due to anemia, hemoglobinopathies, or others), fasting plasma glucose <126 mg/dL or estimated A1C <6.5% calculated from CGM values can be used.
With this standardized definition, researchers will be able to conduct studies and analyze medical records using standard terminology so they can accurately compare factors that help people with type 2 achieve remission and factors that influence remission duration.
A1c Testing still needed if in Remission?
Even if people are experiencing remission, they require continued glucose evaluation because hyperglycemia frequently recurs. People in remission who experience weight gain, are started on steroids or other medications like atypical antipsychotics or meds to treat HIV, may exhibit elevated blood glucose levels. In addition, stress from other forms of illness and the natural decline of beta-cell function over time can all lead to the recurrence of Type 2 diabetes. Testing of A1c or another measure of glycemic levels needs to be performed at least yearly.
Metabolic Memory – people in diabetes remission still experience complications.
Even after a remission, the classic complications of diabetes including retinopathy, nephropathy, neuropathy, and enhanced risk of cardiovascular disease can still occur due to metabolic memory.
Diabetes Care Consensus Report 2021
The metabolic memory or legacy effect is relevant in this setting. If a person with diabetes has a history of hyperglycemia, this metabolic memory can cause persisting harmful effects in various tissues. Even after remission, the classic complications of diabetes including retinopathy, nephropathy, neuropathy, and enhanced risk of cardiovascular disease can still occur. This is why it is important for people in diabetes remission to have regular retinal screening, tests of renal function, foot evaluation, and measurement of blood pressure and weight in addition to ongoing monitoring of A1c.
To read the complete article from Diabetes Care, Aug 2021, Consensus Report: Definition and Interpretation of Remission in Type 2 Diabetes.
Are you preparing for the CDCES Exam?
Join us live on November 4th, for our FREE Webinar
Starting your journey to becoming a CDCES? We recommend watching our FREE Preparing for CDCES Exam Webinar!
This course will transform your test anxiety into calm self-confidence and test-taking readiness.
Webinar Topics
- Exam requirement updates for 2021.
- Exam eligibility and test format
- Strategies to succeed along with a review of study tips and test-taking tactics.
- We will review sample test questions and the reasoning behind choosing the right answers.
- Learn how to focus your time and prepare to take the CDCES Exam. We provide plenty of sample test questions and test-taking tips!
Can’t join us live?
Don’t worry, we will send you a link to the recorded version.
What is a Certified Diabetes Care and Education Specialist?
Read More: What is a CDCES? First awarded in 1986, as Certified Diabetes Educator (CDE) credential and in 2020 with a new name: Certified Diabetes Care and Education Specialist (CDCES) to more accurately reflect the specialty. CDCES has become a standard of excellence for the delivery of quality diabetes education. Those who hold this certification are known to possess comprehensive knowledge of and experience in diabetes prevention, management, and prediabetes. “Becoming a Certified Diabetes Care and Education Specialist (CDCES) is one of the best professional and personal decisions I have ever made.” – Coach Beverly Thomassian, RN, MPH, CDCES, BC-ADM
Why become a CDCES?
Three Reasons from Coach Beverly
Read More: 3 Reasons to Become a CDCES “The best part of becoming a CDCES is working with my colleagues and people living with diabetes. As diabetes educators, we hear compelling and beautiful life stories. I am astounded by the barriers they face and inspired by their adaptability, problem-solving skills, and resilience.” Reason 1: CDCES is a widely recognized certification by employers and health care professionals throughout the U.S. This credential demonstrates a specialized and in-depth knowledge in the prevention and treatment of individuals living with pre-diabetes and diabetes. Reason 2: Currently, 10% of people in the U.S. have diabetes and another 35% have pre-diabetes which means 45% of Americans are running around with elevated blood glucose levels. Given this epidemic, there will be plenty of future job opportunities. Reason 3: Having my CDCES along with my nursing degree, has opened many doors of opportunity; from working as an inpatient Diabetes Nurse Specialist in a hospital to working as a Manager of Diabetes Education in the outpatient setting to starting my own consulting company.
Sign up for Diabetes Blog Bytes – we post one daily Blog Byte from Monday to Friday. And of course, Tuesday is our Question of the Week. It’s Informative and FREE! Sign up below!
[yikes-mailchimp form=”1″]Accreditation: Diabetes Education Services is an approved provider by the California Board of Registered Nursing, Provider 12640, and Commission on Dietetic Registration (CDR), Provider DI002. Since these programs are approved by the CDR it satisfies the CE requirements for the CDCES regardless of your profession.*
The use of DES products does not guarantee the successful passage of the CDCES exam. CBDCE does not endorse any preparatory or review materials for the CDCES exam, except for those published by CBDCE.
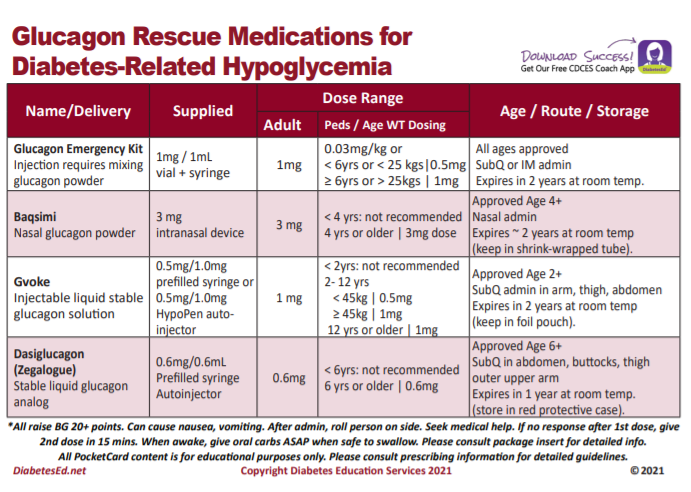
Glucagon Kit Recall Alert – Let’s get the Word Out
Eli Lilly and Company issues a voluntary nationwide recall of one lot of GLUCAGON® Emergency Kit due to Loss of Potency. Warning – A person with severe hypoglycemia who injects this faulty formulation will experience worsening hypoglycemia.
Eli Lilly and Company is voluntarily recalling lot D239382D, Expiration April 2022, of Glucagon Emergency Kit for Low Blood Sugar (Glucagon for Injection, 1 mg per vial; Diluent for Glucagon, 1 mL syringe).
Loss of Potency due to manufacturing process issue

The Eli Lilly injectable glucagon kit (pictured here), usually contains a syringe with diluent and a vial with powdered glucagon. The user needs to put the diluent into the vial with the powdered glucagon and reconstitute it before injecting it.
However, a product complaint from a user found that the vial of Glucagon was in liquid form instead of powder form. Associated with this useful product complaint, the patient who was given this glucagon vial content, experienced worsening hypoglycemia and also reported subsequent seizures.
The use of the liquid form of this product may fail to treat severe low blood sugar due to loss of potency.
It is well known that severe hypoglycemia in people with diabetes, if not promptly treated and reversed, can potentially cause adverse health consequences ranging from transient, minor complaints to neurological damage, seizures, and even death. Eli Lilly’s investigation indicates that the liquid in this Glucagon vial could be related to a problem with the manufacturing process.
Please help get the word out
The Eli Lilly Glucagon product is packaged in a kit containing 1mg of freeze-dried (lyophilized) product in a 3 mL vial and a pre-filled diluent syringe. The affected Glucagon Emergency Kit lot is D239382D and the expiration date is April 2022 (label expiry date: 04 2022). The lot number can be found on the label of the kit as well as the vial (refer to the complete FDA warning below). The lot was distributed nationwide to wholesalers and retailers.
Contact Info for Consumers
Consumers in possession of Glucagon Emergency Kit lot D239382D should contact The Lilly Answers Center at 1-800-LILLYRX (1-800-545-5979) for return and replacement instructions for the product (hours of operation are Monday- Friday, 9AM – 7PM EST) and should contact their health care provider for guidance. Consumers should contact their physician or healthcare provider if they have experienced any problems that may be related to taking or using this product.
Lilly is notifying its distributors and customers by written communication and is arranging for the return and replacement of all recalled products. Wholesalers and Distributors with an existing inventory of Glucagon Emergency Kit lot D239382D should cease distribution and quarantine the product immediately.
Read complete FDA Announcement Here
FREE Glucagon PocketCards
There are now 4 different glucagon formulations to choose from.
This free card details the different formulations available, from the injectables to the nasal powder formulation.
The backside includes teaching and hypoglycemia prevention strategies, along with the different official levels of hypoglycemia (for your certification study preparation).
Join us live on November 11th for the upcoming
Meritus Health’s Virtual Diabetes Conference
Diabetes in the 21st Century with Coach Beverly

Join us live on November 11th from 8:00 am to 4:00 pm for our Virtual Conference: Diabetes in the 21st Century | 6.5 CEs
This conference offers comprehensive presentations on care of a person with diabetes examining a variety of evidence-based topics to aid in the care of a person with diabetes.
Click here to download the program flyer.
Location: Virtual
Fees: No charge for Meritus Health Employees. $50.00 for Non-Meritus Health Participants Meritus Health Employees: Please register via Healthstream, using keyword search “21st Century” or by clicking here.
Cancellation Policy: If you must cancel, please notify Ruth Leizear by phone at 301-790-8619 or toll free at 888-803-1518.
Check-in: Check-in starts at 8:00 a.m., please log in 15 minutes prior to the first presentation
Accreditation:
- Registered Nurses: Nursing Education Department of Meritus Health is accredited with distinction as a provider of nursing continuing professional development by the American Nurses Credentialing Center’s Commission on Accreditation.
6.5 ANCC Contact Hours will be awarded; No partial credit will be given. - Dieticians: Approved for 6.5 CPE II for Registered Dietitians by the Commission on Dietetic Registration.
Click here to download the program flyer.
Instructor: Beverly Thomassian RN, MPH, CDCES, BC-ADM is a working educator and a nationally recognized diabetes expert.
Sign up for Diabetes Blog Bytes – we post one daily Blog Byte from Monday to Friday. And of course, Tuesday is our Question of the Week. It’s Informative and FREE! Sign up below!
[yikes-mailchimp form=”1″]Accreditation: Diabetes Education Services is an approved provider by the California Board of Registered Nursing, Provider 12640, and Commission on Dietetic Registration (CDR), Provider DI002. Since these programs are approved by the CDR it satisfies the CE requirements for the CDCES regardless of your profession.*
The use of DES products does not guarantee the successful passage of the CDCES exam. CBDCE does not endorse any preparatory or review materials for the CDCES exam, except for those published by CBDCE.
We are Celebrating DiabetesEd Specialist Scholarship Recipients
We are so excited to announce our DiabetesEd Specialist Scholarship Recipients!
We received dozens of applications for our annual Making a Difference Scholarship and the Flower Scholarship gifted from an anonymous donor! It was a great personal joy for our team to read these scholarship applications. Each applicant is serving communities with a great need and going “above and beyond” to promote and provide accessible diabetes care and education. It is always a very difficult decision for all of the judges, and we read each application in careful detail considering the financial need, impact, volunteerism, and readiness to take the CDCES exam.
We greatly appreciate the good work of all the applicants and thank them for their service!
This year we are offered 3 Scholarship Options for our Virtual DiabetesEd Specialist Conference, October 6-8, 2021.
Congratulations Chantel Wade, his year’s Flower Scholarship Recipient!
Chantel Wade is the recipient of our “Flower Scholarship.” Chantel is an ambulatory RN and the lead in the Patient Education Department at her local health center. There she serves a diverse population of individuals from different socioeconomic backgrounds, seeing many people who are on Medicare, Medi-Cal or are uninsured. She uses a hands-on, interactive approach with those she works with; she is committed to meeting people where they are by creating custom care plans that meet their individual needs. Outside of work, she is active in her local Fellowship Church and other organizations where she volunteers her time and expertise to offer pre-diabetes and diabetes education.
Congratulations Keira McCrary, “Making a Difference Exemplar Scholarship” Recipient!
Keira McCrary is the recipient of our “Making a Difference Exemplar Scholarship” because of her dedication to her community. Keira works as a Registered Dietician who provides direct care services to Native American tribal communities in her area. In her work, she supports people living with diabetes through all stages of life with programs such as home meal delivery for elder tribal members and the Native Youth Preventing Diabetes Organization. Through Native Youth Preventing Diabetes Organization Keira assists in the education of tribal youth in the areas of diabetes prevention, nutritional education, physical activity, behavioral health, and more. She also creates user-friendly tools for those she works with such as informational “how-to” diabetes-friendly recipe videos and a weekly newsletter.
Congratulations Logan Mumphrey, “Making a Difference Scholarship” Recipient!
Logan Mumphrey is our second recipient of our “Making a Difference Scholarship” for many reasons! Logan is currently working towards his MSN/FNP and has worked as the primary nurse and clinical coordinator for transgender health services helping to build the program from the ground up. This program provides gender-affirming care that goes beyond hormone therapy including care navigation, surgery coordination, assistance with identity document changes, peer support, and much more. Logan is passionate about diabetes care and education and hopes that by becoming a CDCES, it will allow him to provide more support for those he works with so they can manage their diabetes with a gender-affirming lens.
This year we are offered 3 Scholarship Options which include:
- Flower Scholarship valued at $1000 for a diabetes nurse educator who comes from an under-served community and is providing care and education to communities that lack access to Diabetes Specialists and health care resources. The nurse applicant taking their CDCES exam within a year. The donor of this scholarship is generously providing funds to cover course registration plus enrollment in our Ultimate Online Bundle, Diabetes Educator Course 2021 Syllabus Hard Copy – over 100 pages, ADA 2021 Standards of Care Book DiabetesEd Services highlighters, PocketCard and Pen.
- Making a Difference Exemplar Scholarship valued at $1000 for a diabetes educator who exemplifies advocacy and compassionate care in their community and is pursuing their CDCES. This top-tier scholarship provides funds to cover course registration plus enrollment in our Ultimate Online Bundle, Diabetes Educator Course 2021 Syllabus Hard Copy – over 100 pages, ADA 2021 Standards of Care Book DiabetesEd Services highlighters, PocketCard and Pen.
- Making a Difference Scholarship valued at $900 for a diabetes educator who exemplifies advocacy and compassionate care in their community and is pursuing their CDCES. This scholarship provides funds to cover course registration plus enrollment in our Ultimate Online Bundle.
The goal of these scholarships are three-fold:
- To support U.S. health care professionals who are going above and beyond to improve diabetes care in their community; and
- To support applicants’ effort to become a Certified Diabetes Care and Education Specialist (CDCES) and
- To provide financial assistance with the DiabetesEd Course registration fee and or sleeping rooms
3 Important Reasons to Recognize and Address Trauma
As a child, LR lived with neglect and mistreatment by their parents. Escaping home as a teenager, LR couch surfed at friends but finally ending up living in their car. At the age of 23, LR showed up at our local community clinic with dysregulation, depression, and anxiety coupled with a new diagnosis of type 2 diabetes and elevated triglycerides. LR had limited access to healthy food and carried a BMI of over 35.
After a few months of getting comfortable with the clinic staff, our counselor asked LR to complete the Adverse Childhood Experiences (ACE) screening assessment. After LR finished checking off their adverse childhood experiences, they looked up with tears and said, “I scored a 9 out of 10”.

Adverse Childhood Experiences (ACEs) are common. At least two-thirds of people living in the U.S. have experienced one ACE and over 15% have experienced 4 or more.
Furthermore, a dose-response relationship exists: as the number of adverse experiences increases so does the risk of problems from childhood through adulthood.
These childhood traumas can lead to toxic stress which, over time, can change the biology of our bodiy.
People with elevated ACE scores are more likely to experience a variety of mental health issues, which is not surprising given their painful, confusing, and unsafe childhoods. Based on sound research by the CDC and Kaiser, they are also more likely to suffer from physical diseases, like heart attack and stroke, diabetes, and cancer. They are more likely to break bones and experience unintended pregnancies.
Join Coach Beverly at an Upcoming Webinar
The Impact of Adverse Childhood Experiences on Health: A Personal Story of Resilience and Hope with Coach Beverly
ADCES National Virtual Meeting – Ready for Viewing
California Coordinating ADCES Chapter – September 30, 2021 at 4:45pm PST
Diabetes Ed Services Webinars – airs October 27th at 11:30 am PST
Toxic Stress Affects us at the Cellular Level
Research shows that ACEs can lead to a cycle of toxic stress and cellular inflammation. This heightened adrenal-mediated “flight or fight” response over time, can lead to neuroendocrine dysregulation, altered immune response, affect DNA packaging and activate epigenetic tags that can alter genetic makeup.
The CDC Morbidity and Mortality Weekly 2019 report tell us that preventing ACEs could reduce:
- 21 million cases of depression
- 1.9 million cases of heart disease
- 2.5 million cases of excess weight
The first Surgeon General of California, Nadine Burke Harris, MD, MPH, has made it her mission to increase awareness, identify and address ACEs with parents, children, and adults so that we can break the cycle.
Health care professionals at risk for ACEs
People who enter healing professions may be experiencing toxic stress from childhood or current trauma. They may be dealing with burnout, fear, or feelings of deep pain with their past coupled with all the intensity of providing care during the COVID pandemic. This chronic and toxic stress can lead to dysregulation while impairing our ability to cope and care for others. You are not alone.
My own personal journey of experiencing childhood trauma and holding myself together until I ended up in the hospital, has compelled me to share my story with you. And offer a message of hope.
Coach Beverly
As I work on healing and integrating the different aspects of myself, I now feel more attuned to others who have weathered and survived childhood trauma. This awareness has significantly changed the way I hear what people with diabetes are saying and interpret what they are doing. For example, knowing that LR had a very high ACE score, I was able to adjust my expectations and focus on behavior changes that support self-care and self-regulation. When LR doesn’t take their diabetes medications for a few weeks, I provide gentle strength-based coaching to help LR get back on track. I make sure LR knows that they are safe sharing the truth of their story, no matter what.
In your hospital setting, do you have a person who keeps getting readmitted to the hospital in a diabetes crisis? In your outpatient setting, do you experience frequent no-shows or situations where people aren’t able to make changes in self-care? Maybe, they are struggling with the emotional impact of toxic stress.
Adults who have experienced trauma as children may exhibit the following behaviors:
- Missing appointments
- Not taking meds as prescribed
- Not adopting new lifestyle changes
As Diabetes Care and Education Specialists, if we recognize these behaviors as a response to dysregulation due to toxic stress, we can provide a therapeutic response to start the healing process.
Helpful provider responses when you suspect that participants are not engaging in care due to childhood trauma and toxic stress:
- Refrain from harsh language or judgement
- Be curious, ask open ended questions
- Provide the ACE screening tool to start the conversation
- Encourage collaboration using a person centered approach
- Identify mental health resources in you community
Diabetes Care and Education Specialists recognize that the mind and body are a deeply connected, dynamic, and powerful force when they are working together in harmony. When trauma and toxic stress are not recognized or treated, there can be devastating health consequences. We can make a difference in preventing, recognizing, and helping people heal from adverse childhood experiences.
Want to learn more about the ACEs and Healing?
Join Coach Beverly at an Upcoming Webinar
The Impact of Adverse Childhood Experiences on Health:
A Personal Story of Resilience and Hope with Coach Beverly
ADCES National Virtual Meeting – Ready for Viewing
California Coordinating ADCES Chapter – September 30, 2021 at 4:45pm PST
Diabetes Ed Services Webinars – airs October 27th at 11:30 am PST
Resources
ACE Screening Tool and Resilience Inventory
Becoming ACE-Aware Training Program
Nadine Burke Harris, MD TED Talk on How Childhood Trauma affects health
NPR Article – Take the ACE Score and Learn what it does and doesn’t mean
Trauma-Informed Care Fact Sheet
Why should I care about my number?
CDC Vital Signs – Impact of ACES
CDC Mortality and Morbidity Weekly Report on ACEs – 2019
What happened to you? Conversations on Trauma, Resilience, and Healing – authors Oprah Winfrey and Bruce D. Perry, M.D., Ph.D.
Sign up for Diabetes Blog Bytes – we post one daily Blog Byte from Monday to Friday. And of course, Tuesday is our Question of the Week. It’s Informative and FREE! Sign up below!
[yikes-mailchimp form=”1″]Accreditation: Diabetes Education Services is an approved provider by the California Board of Registered Nursing, Provider 12640, and Commission on Dietetic Registration (CDR), Provider DI002. Since these programs are approved by the CDR it satisfies the CE requirements for the CDCES regardless of your profession.*
The use of DES products does not guarantee the successful passage of the CDCES exam. CBDCE does not endorse any preparatory or review materials for the CDCES exam, except for those published by CBDCE.
August eNews | Trauma and Hidden Barriers to Type 1 Tech Use
Click here to read our full August 2021 newsletter.
Featured Blogs
- DiabetesEd Scholarship Recipients
- 3 Reasons to Recognize and Address Trauma
- Rationale of the Week
- Question of the Week
Upcoming Events & Resources