January 2021 eNews – 5 Reasons to Celebrate & Most Frequently Asked Exam Question
January 2021 eNews – 5 Reasons to Celebrate 2021
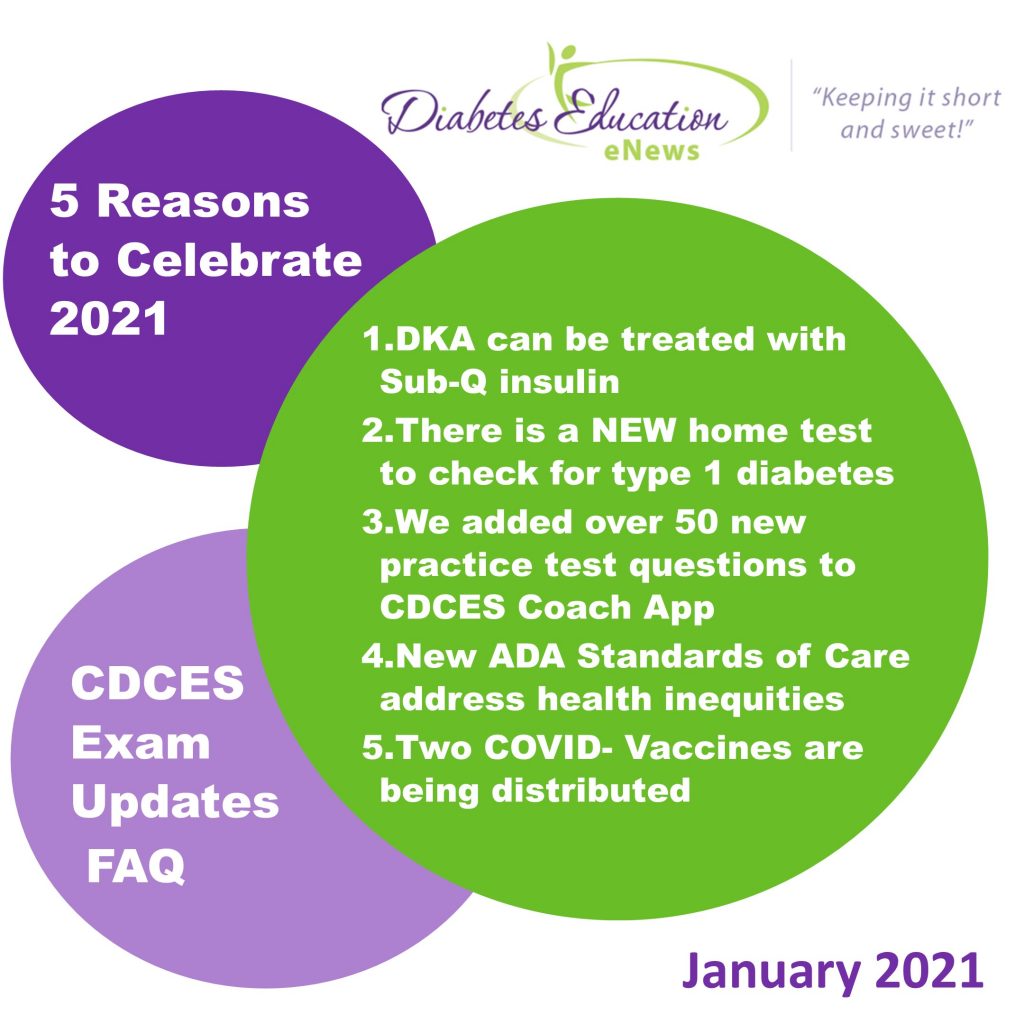
5 Reasons to Celebrate 2021
- DKA can be treated with Sub-Q insulin
- There is a NEW home test to check for type 1 diabetes
- We added over 50 new practice test questions to CDCES Coach App
- New ADA Standards of Care address health inequities
- Two COVID- Vaccines are being distributed
In this newsletter, we are excited to celebrate notable breakthroughs.
As a diabetes nurse for over 20 years, I assumed that the ONLY way to treat DKA was with an insulin drip. It turns out that a Sub-Q approach is as effective and safe. Investigate more about the steps involved in this approach in our featured article.
In the past, testing for type 1 diabetes required a provider order. Now, concerned family members can choose to get tested from home. Read more about this super easy screening test for type 1 diabetes.
Our rationale of the week brings Section 1 of the new ADA Standards on Population Health to light. This standard boldly addresses social determinants of health, with an intense focus on food insecurity and other barriers to self-care.
Lastly, this Monday, I was lucky enough to get my first dose of the Pfizer COVID-19 vaccine. I sported a sore arm for less than 24 hours and that was it. Now, I am anxiously cheering for all my family, friends, colleagues, and community to get this life-saving vaccination.
Stay safe everyone and don’t forget to get enough sleep!
Click here to read our full January 2021 newsletter.
Most Frequently Asked Exam Question – Which Standards to Study?
One of the most frequently asked questions about the CDCES Exam is the following:
Should I study this year’s ADA Standards of Care or last year’s ADA Standards of Care?

In this years exam handbook, the CBDCE provided clarification on this high anxiety topic.
CBDCE Exam Content Update Policy
Immediately – New diagnostic criteria or specific guidelines impacting diabetes care and education and/or treatment of diabetes which are released nationally and identified as effective immediately may be including in the examination at any time.
One Year – New medical advances, guidelines, or pharmaceuticals will be included in CDCES Exam no sooner than one year after the information is released.
What does this mean for us?
I have already read and reviewed the 2020 ADA Standards of Care.
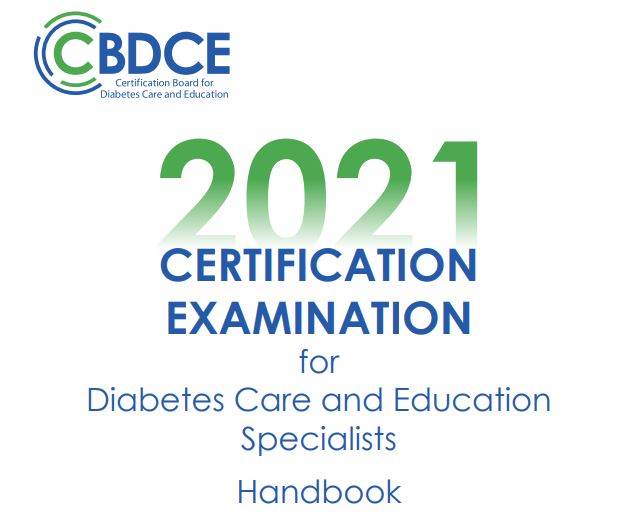
If you have already studied the ADA 2020 Standards of Care, you will be set for the 2021 CDCES Exam. Since there are no new diagnostic criteria or specific guidelines that are dramatically different from the 2020 Standards of Care.
The one exception is that there are updated diabetes management guidelines for the older population as outlined in our Older People Level 2 Course and you can review in the ADA Standards of Care, section 12.
Please see ADA Standards Summary of Revisions for more detailed information on updates for 2021.
I haven’t started reviewing the ADA Standards of Care.
Great. Please plan on studying the 2021 ADA Standards of Care, which includes all of the same content as the 2020 Standards with some additions and updates.
We are all rooting for your success! For More info:
- Download CDCES Coach App FREE for iOS or androids
- Join our Prep for CDCES Webinar FREE
January News Topics
- Treating DKA with Sub-Q Insulin
- At-Home Test for Type 1
- Which Year’s ADA Standards to Study for Exam
- Rationale of the Week – What is Causing Hypoglycemia?
Featured Items
- Level 1 Updates
- Level 3 Updates
- Virtual DiabetesEd Specialist Conference
- Free Resources Catalog
Sign up for Diabetes Blog Bytes – we post one daily Blog Byte from Monday to Friday. And of course, Tuesday is our Question of the Week. It’s Informative and FREE! Sign up below!
[yikes-mailchimp form=”1″]Accreditation: Diabetes Education Services is an approved provider by the California Board of Registered Nursing, Provider 12640, and Commission on Dietetic Registration (CDR), Provider DI002. Since these programs are approved by the CDR it satisfies the CE requirements for the CDCES regardless of your profession.*
The use of DES products does not guarantee the successful passage of the CDCES exam. CBDCE does not endorse any preparatory or review materials for the CDCES exam, except for those published by CBDCE.
December Newsletter | New Diabetes App, Winter Recipes, and a Sprinkling of Gratitude
Click here to read our full December newsletter.

Boy, am I looking forward to 2021.
The New Year brings hope – vaccines to curb the pandemic are around the corner and we keep improving our care for people with COVID infections.
But right now, my heart is heavy. I don’t feel like putting up holiday decorations and my cookie making motivation is at an all-time low.
The hospitals are bursting with people and I am worried about our medical colleagues and their mental and physical health.
I am concerned about the people we serve who live with diabetes, knowing that they are hit especially hard by Corona Virus infections.
Now, more than ever, I am leaning into my strong belief that our compassion, intelligence and humanity, will lift us out of this dark time into the light.
I feel grateful that my business has survived this harsh year. Me, Bryanna and our entire team, worked tirelessly to move all of our programs to a virtual format so that we could deliver critical content to our community.
We created new content on COVID and Diabetes, to help navigate these new uncharted waters. Knowing that many have been impacted financially by the pandemic, we are providing this course and many of our Level 2, Standards of Care Courses for free to ensure important information is accessible.
We believe that armed with information and tools, our community keeps making a significant difference in improving not only outcomes but the quality of life for those living with diabetes.
We are thankful for each one of you and the light you shine on our diabetes community.
In health and gratitude,
Coach Beverly, Bryanna and Jackson
Click here to read our full December newsletter.
Dec News Highlights
- New Diabetes App T1D1
- BG Level Predicts Outcomes
- Finding Gratitude During a Pandemic
- Rationale of Week
- Winter Recipes
Featured Items
FREE Resource Catalog

- Diabetes Cheat Sheets
- Diabetes Blog Bytes
- Medication PocketCards
- Start Your Certification Journey
- CDCES Coach App
- Free Webinars hosted by Coach Beverly
- Question of the Week
See Full Free Resource Catalog
Sign up for Diabetes Blog Bytes – we post one daily Blog Byte from Monday to Friday. And of course, Tuesday is our Question of the Week. It’s Informative and FREE! Sign up below!
[yikes-mailchimp form=”1″]Accreditation: Diabetes Education Services is an approved provider by the California Board of Registered Nursing, Provider 12640, and Commission on Dietetic Registration (CDR), Provider DI002. Since these programs are approved by the CDR it satisfies the CE requirements for the CDCES regardless of your profession.*
The use of DES products does not guarantee the successful passage of the CDCES exam. CBDCE does not endorse any preparatory or review materials for the CDCES exam, except for those published by CBDCE.
October Newsletter | Meds Update, Free Quizzes, and Rationale
Click here to read our full October newsletter.

Greetings to our awesome diabetes community.
For this newsletter, we are excited to share three diabetes medication announcements. Our updated PocketCards are ready for downloading and viewing with these changes.
We know how much you love testing your knowledge, so we have created 3 new quizzes in our CDCES Coach App. For now, you can access these quizzes for free, so flex your test-taking muscle today.
The pandemic has taken a toll on people with diabetes and exposed the impact of health inequities. We take a moment to pause and reflect on the impact of this pandemic, with a special focus on food insecurity and actions we can take to address gaps in health care.
Lainey Koski was the first full-time employee at my company. She was not only an exceptional colleague, she was a wonderful human and friend. We pay tribute to Lainey, who left us way too soon.
Finally, since November 3rd is around the corner, we have included information on finding a polling place near you.
Be safe, take care of yourself, and take time to enjoy the small wonders.
Coach Beverly, Bryanna, and Jackson
Click here to read our full October newsletter.
Sign up for our newsletter
The New Art and Science of Diabetes Care and Education Desk Reference – 5th Edition| $249
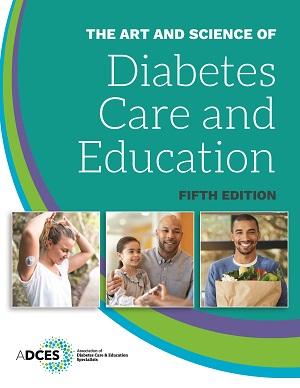
We are so excited that the 5th edition The Art and Science of Diabetes Care and Education is finally here!
This specialist’s one-volume, go-to resource for the core knowledge and skills for providing person-centered care and education to persons with diabetes and related chronic conditions. This is a core resource for those who are studying for the Certified Diabetes Care and Education Specialist® (CDCES) exam.
Updates:
- Two new chapters addressing multiple daily injections (MDI), continuous subcutaneous insulin infusion (CSII), pump therapy, continuous glucose monitoring (CGM) and intensifying therapy, pattern management, and data analysis.
- Revised AADE7 Self-Care Behaviors®, with its recognition of the impact the emotional burden of diabetes on metabolic and quality of life outcomes.
- Highlights obesity management, including the 3-step algorithm for care of overweight and obese people with diabetes.
- Expanded coverage of motivational interviewing (MI).
- Major rewrites of the kidney disease and diabetic neuropathies chapters.
Sign up for Diabetes Blog Bytes – we post one daily Blog Byte from Monday to Friday. And of course, Tuesday is our Question of the Week. It’s Informative and FREE! Sign up below!
[yikes-mailchimp form=”1″]Accreditation: Diabetes Education Services is an approved provider by the California Board of Registered Nursing, Provider 12640, and Commission on Dietetic Registration (CDR), Provider DI002. Since these programs are approved by the CDR it satisfies the CE requirements for the CDCES regardless of your profession.*
The use of DES products does not guarantee the successful passage of the CDCES exam. CBDCE does not endorse any preparatory or review materials for the CDCES exam, except for those published by CBDCE.
September Newsletter | New Online Scholarship, Liver Disease, CGM Update
Click to view the September Newsletter

What a year!
Thank you everyone for your support as I shared my adventure of moving my oldest son into his Texas college dorm two weeks ago. He is thriving and excited to live away from home, hang out with other students (while wearing a mask) and attend a combination of virtual and live classroom instruction. My 15-year-old son, Jackson, has stepped into Robert’s role at our company and is doing a great job fulfilling orders and working on special projects.
A special shout out of recognition to all of you who are juggling homeschooling, new working situations, and your lives. This is a tough time for all of us and I miss seeing all of you!
Speaking of virtual instruction, we have great news to share. Our DiabetesEd Boot Camp starts on Sept 16th. We can’t wait to join together with you in the community again as we hunker down to prepare for certification exams.
We are excited to announce that we are offering two Online University Scholarships for diabetes advocates that are “Making a Difference” in their community. Please share it with your colleagues and friends.
In addition, this newsletter explores the importance of promptly recognizing the liver disease and the cost-saving benefits of CGM technology.
Lastly, we love providing our customers with easy-to-find resources, so we put all our most popular Cheat Sheets on one Resource Page for fast access.
During this time of uncertainty and financial hardships, we will be offering frequent discounts. It’s our way of saying thank you with a virtual hug of appreciation.
Warmest regards,
Coach Beverly, Bryanna, and Jackson
Sign up for Diabetes Blog Bytes – we post one daily Blog Byte from Monday to Friday. And of course, Tuesday is our Question of the Week. It’s Informative and FREE! Sign up below!
[yikes-mailchimp form=”1″]
Accreditation: Diabetes Education Services is an approved provider by the California Board of Registered Nursing, Provider 12640, and Commission on Dietetic Registration (CDR), Provider DI002. Since these programs are approved by the CDR it satisfies the CE requirements for the CDCES regardless of your profession.*
The use of DES products does not guarantee the successful passage of the CDCES exam. CBDCE does not endorse any preparatory or review materials for the CDCES exam, except for those published by CBDCE.
DiabetesEd Top 3 Blog Posts | July 1, 2020
Click here to view our Top 3 Blogs Newsletter

Happy Wednesday Diabetes Community!
We are excited to announce our new feature; Top 3 blog posts of the Month.
Coach Beverly and team are committed to keeping you apprised of the latest findings in diabetes.
We promise to keep this end-of-the-month wrap-up announcement short and sweet while providing links to references so you can dig deeper.
As part of our commitment to sharing information, we are offering FREE webinar viewing of our Level 2 Standards Intensive Series. See upcoming topics and dates below.
Our top 3 blogs this month include the recall of some long-acting metformin brands, Medicare’s $35 monthly cap on insulin starting in 2021, and the rationale for this month’s most popular question of the week.
Happy early July 4th weekend. Please stay safe and take good care.
Coach Beverly
Click here to view our Top 3 Blogs Newsletter
Check out our new bundle!
Level 3 | Boot Camp + Expert Team Bundle
Join us live starting September 16th!
When you join our DiabetesEd Certification Boot Camp, it’s like having your own online coaching staff.
?In each webinar, either Coach Beverly, Dr. Isaacs, or Ms. Armstrong, highlight the critical content of each topic area, so you can focus your study time most efficiently. They also launch multiple poll questions to help participants focus on key concepts and assess their knowledge while learning the best test-taking strategies.
Mastery of this content is critical to ensure certification exam success and to improve clinical outcomes.
Click here to download Level 3 + Expert Bundle flyer
Sign up for Diabetes Blog Bytes – we post one daily Blog Byte from Monday to Friday. And of course, Tuesday is our Question of the Week. It’s Informative and FREE! Sign up below!
[yikes-mailchimp form=”1″]Accreditation: Diabetes Education Services is an approved provider by the California Board of Registered Nursing, Provider 12640, and Commission on Dietetic Registration (CDR), Provider DI002. Since these programs are approved by the CDR it satisfies the CE requirements for the CDCES regardless of your profession.*
The use of DES products does not guarantee the successful passage of the CDCES exam. CBDCE does not endorse any preparatory or review materials for the CDCES exam, except for those published by CBDCE.
May Newsletter | Insulin Savings, Telehealth Updates, and Salivary Glucose Testing
Click here to read our entire May Newsletter

As a Diabetes Nurse Specialist in a local clinic, I am providing telehealth once a week. During these visits, I am checking in with people about their food and medications.
Do you have enough food and insulin to last? Most of them answer, “yes, for now”.
Many of them may run out of insulin and supplies in the near future, some as a result of the costs that make essential medications in-affordable. If this is the case, what can we offer them?
We are excited to thank our guest contributor and Diabetes Educator of the Year, Dr. Diana Isaacs, who has provided us with helpful information and a multitude of resources for people in need of low-cost insulin.
In light of the COVID-19 emergency, the Centers for Medicare & Medicaid Services (CMS), has expanded opportunities to provide remote care to people with diabetes. We have highlighted some recent updates and provided links to helpful resources for your billing team.
Lastly, we are looking towards the future with salivary glucose testing and insights into a past Question of the Week.
I am grateful to be a part of this amazing community of diabetes specialists. Thank you for your care, concern and advocacy.
Be well! Coach Beverly
Click here to read our entire May Newsletter
Virtual Course Insulin Therapy, Pumps, & CGM + CV Risk Reduction Strategies
Earn 4.0 CEs | $69
Join Diana Isaacs, PharmD, BCPS, BC-ADM, BCACP, CDCES, and ADCES 2020 Diabetes Educator of the year as she reviews these important topics. As Diabetes Specialists, we are tasked with taking a leadership role in technology and cardiovascular risk reduction. Dr. Isaacs will address these topics with clinical insight and expert knowledge during these two virtual courses.
Session 1 | CV Risk Management with Pharmacology and Intensive Insulin Therapy | Recorded & Ready for Viewing!
Session 2 | Continuous Glucose Monitoring and Insulin Pump Therapy | Recorded & Ready for Viewing!
Objectives:
- Describe critical teaching content before starting insulin pump therapy.
- Describe appropriate candidates for insulin pump therapy.
- Discuss strategies to determine and fine-tune insulin pump basal rates.
- Discuss how to determine and fine-tune bolus rates including coverage for carbs and hyperglycemia.
- State important safety measures to prevent hyperglycemic crises.
- List inpatient considerations for insulin pump therapy and CGMs.
- Discuss features of available professional and personal CGMs and insulin pumps.
- Describe CV risk factors associated with diabetes and future event prediction.
- List different pharmacologic approaches to mitigate CV events.
$69 | Earn 4 CEs
These sessions are also included in our Virtual Conference.
Sign up for Diabetes Blog Bytes – we post one daily Blog Byte from Monday to Friday. And of course, Tuesday is our Question of the Week. It’s Informative and FREE! Sign up below!
[yikes-mailchimp form=”1″]Accreditation: Diabetes Education Services is an approved provider by the California Board of Registered Nursing, Provider 12640, and Commission on Dietetic Registration (CDR), Provider DI002. Since these programs are approved by the CDR it satisfies the CE requirements for the CDCES regardless of your profession.*
The use of DES products does not guarantee the successful passage of the CDCES exam. CBDCE does not endorse any preparatory or review materials for the CDCES exam, except for those published by CBDCE.
April Newsletter | COVID-19 & Best Diabetes Care
Click here to read our entire April Newsletter

At a local hospital, a person in their mid-40s, with type 2 diabetes was admitted for treatment of COVID-19 and Diabetes Ketoacidosis (DKA). An insulin drip was started and their SGLT-2 Inhibitor was stopped. Why are people with type 2 and COVID-19 going into DKA and how is this impacting outcomes?
A person with type 1 diabetes calls into a rural health clinic and says they are running a temperature, having difficulty breathing and can’t get their blood sugars below 300. The diabetes specialist instructs them to go to the hospital. What supplies should they take in case they are admitted to the hospital?
How do we help prepare people with diabetes for the possibility of hospitalization and what are best practices to care for people with diabetes and COVID-19 in the hospital setting?
What instruction do we provide for people with diabetes if they get sick and are wondering if they need to go to the hospital?
In this newsletter, our goal is to answer these questions based on the opinions of experts in the field and the best information to date.
In addition, we are excited to share information on drone delivery of insulin, mask making and the opportunity to celebrate the AADE (ADCES) Educator of the Year, Dr. Diana Isaacs.
Lastly, please let CMS (Medicare) know that RNs and Pharmacists need to be considered as providers of DSME telehealth services. Now, more than ever, we need all hands on deck.
Thank you everyone. Take extra good care of yourselves.
Beverly
Click here to read our entire April Newsletter
Positioning our Practice for the Future | February Newsletter
February Newsletter Now Available!

Our February Newsletter celebrates the future of diabetes care and education. As we settle into the year with a new title, amazing advances in health tech, and a person-centered approach, we are excited about what’s ahead! Our newsletter and Blog Bites are focused on filling the knowledge gaps while honoring these changes, as we move into a new era of diabetes care and education.
Sign up for our Monthly Newsletter
Featured Blog Byte
Every weekday our Diabetes Detective Team scans the news to discover and report on the most relevant info that Diabetes Ed Specialists need for their daily practice.
New Triple Combo Pill for Type 2 Diabetes

The FDA made history last month by approving the first-ever triple combination pill for type 2 diabetes. This medication can help simplify the medication regimen for people living with type 2 diabetes.
As the director of the diabetes research unit at the University of Texas Health Science Center at San Antonio, Ralph A. DeFronzo, MD, said, “Type 2 diabetes is a complex disease that often requires the use of multiple antidiabetic medications to improve glycemic control. Having three different diabetes medications in a single tablet is an important advance in diabetes treatment.”
Known as Trijardy XR, this medication combines the SGLT2 inhibitor empagliflozin, the DPP-IV inhibitor linagliptin, and metformin extended-release. Both empagliflozin and linagliptin lower blood glucose and empagliflozin has the added benefit of reducing the risk of cardiovascular death and chronic heart failure for those living with cardiovascular disease or chronic heart failure.
Additionally, a trial that was presented at the American Diabetes Association (ADA) Scientific Sessions by Healio found that linagliptin will not increase the risk for a cardiovascular event, nor will it contribute to the progression of renal disease among people with type 2 diabetes. This trial, known as the CARMELINA trial, was conducted over six years, across a group of 6,000 people. The trial demonstrated that no “between-group differences for the incidence of nonfatal myocardial infarction, nonfatal stroke and CV death during a median of 6 years.”
- Trijardy XR will be available in four dosages:
- 5 mg empagliflozin/2.5 mg linagliptin/1,000 mg metformin ER
- 10 mg empagliflozin/5 mg linagliptin/1,000 mg metformin ER
- 12.5 mg empagliflozin/2.5 mg linagliptin/1,000 mg metformin ER
- 25 mg empagliflozin/5 mg linagliptin/1,000 mg metformin ER.
There is no information on pricing as of yet. Read more about Trijardy here.
Sign up for Diabetes Blog Bytes – we post one daily Blog Byte from Monday to Friday. And of course, Tuesday is our Question of the Week. It’s Informative and FREE! Sign up below!
[yikes-mailchimp form=”1″]








