Cancer and Diabetes
This blog explores the relationship between cancer and diabetes. We differentiate the risk of cancer for people with type 1 and type 2 diabetes. Lastly, we explore the importance of diabetes educators in promoting lifestyle change and being involved early detection and cancer prevention.
Together, we can help those living with diabetes take early action and get appropriate screenings!
Type 1 and Type 2 Diabetes
What’s the Link?

Diabetes is the 7th leading cause of death.
What is the intersection between diabetes and cancer?
In 2010, Diabetes and Cancer, a Consensus Statement was the first official report that brought this connection to light. Since that initial publication, our understanding of this co-relationship continues to evolve. This article highlights these newer findings.
There are risk factors that are common to both diseases:
- Aging
- Obesity
- Diet
- Physical Inactivity
- Alcohol
- Smoking
- Ethnicity
In addition, there are some possible mechanisms for a direct link. People with diabetes and cancer share:
- Inflammation
- Hyperglycemia
- Hyperinsulinemia
In both conditions, cellular inflammation exists and some researchers have suggested that the abundance of glucose feeds hungry tumor cells.
Cancer and Diabetes Rates
Type 1 Diabetes and Cancer – Risk Compared to general population.

- Stomach
- Liver
- Kidney
- Pancreas
- Endometrium
Decreased Cancer Risk of:
- Breast
- Prostate
Type 2 Diabetes and Cancer – Risk Compared to general population.

- Liver
- Pancreas
- Endometrium
- Breast
- Bladder
- Colon
Decreased Cancer Risk of:
- Prostate
Prevention and Screenings are Critical
Since the link between diabetes and cancer seems to be due in part to shared risk factors such as obesity, diet and inactivity, we can continue to promote the usual lifestyle adjustments:
- Promote healthy diet, high in fiber, fruits and vegetables and decrease meat intake
- Increased activity and weight loss improves outcomes of type 2 diabetes and some forms of cancer.
- Strongly encourage people with diabetes to undergo appropriate cancer screenings. This is especially true for people with type 2, who tend to receive less cancer screenings than those with type 1 diabetes.
Diabetes Medications and Cancer
Some diabetes medications should not be used in patients at risk of certain cancers.
- Pioglitazone (Actos) may increase bladder cancer risk.
- Dapagliflozin (Farxiga) should not be used in patients with bladder cancers.
- GLP-1 Receptor Agonists should not be used in patients at risk for medullary thyroid tumor.
Download Medication PocketCard for reference »

Metformin is a plant based derivative. It originates from French Lilac, Galega Officinalis.
Results of a growing number of observational human studies suggest that treatment with metformin (relative to other glucose-lowering therapies) is associated with reduced risk of cancer or cancer mortality.
There are trials underway to see if metformin is associated with slowing cellular aging and increasing telomere length.
As diabetes educators, we can help increase awareness of the association between cancer and diabetes. We can inform and advocate to make sure patients get appropriate screenings with a focus on early detection.
Want to learn more?
Join us to explore the relationship between cancer and diabetes and to use a case study approach to determine best strategies to manage hyperglycemia during chemotherapy on steroids.
Diabetes and Cancer Course – Earn 1.5 CEs >>
This On Demand Presentation now available
Earn 1.5 CEs and learn more about this important topic.
Improving Dental Hygiene May Lower Risks for New-Onset Diabetes | Mindful Monday

A study published earlier this month by Diabetologia tested a possible link between oral hygiene and new-onset diabetes.
In an attempt to determine if there is a relationship between periodontal (gum) disease and the rate of new-onset diabetes, Yoonkyung Chang, Ph.D., and researches at the Ewha Woman’s University College of Medicine in Seoul, South Korea, analyzed a series of data collected by the National Health Insurance System-Health Screening Cohort (NHIS-HEALS). This data which was collected from 2003 to 2006, across more than 188,000 subjects, found a positive link between oral care and new-onset diabetes.
Of the included subjects, 17.5% had periodontal disease. After a median follow-up of 10.0 years, diabetes developed in 31,545 (event rate: 16.1%, 95% CI 15.9%, 16.3%) subjects.
The correlation between periodontal disease and new-onset diabetes remained positively associated even after adjusting the data for demographics and lifestyle choices such as regular exercise, alcohol consumption, and vascular risk factors, among others.
The good news is that the study did find that regular tooth brushing (3x a day) had a negative association with new-onset diabetes.
To read more about this study, click here.
Sign up for Diabetes Blog Bytes – we post one daily Blog Byte from Monday to Friday. And of course, Tuesday is our Question of the Week. It’s Informative and FREE! Sign up below!
[yikes-mailchimp form=”1″]
Question of Week Rationale – Common Barrier for LGBTQ Population
For the Question of the week, QoW, test takers usually choose the correct answer 70-80% of the time. However, for one question of the week, about 40% of respondents chose the correct answer.
So, we thought this would be a perfect opportunity for another answer rationale. We’ll explore this question and the best answer in more detail and throw in some test-taking tips along the way. Before we start though, if you don’t want any spoilers and haven’t tried the question yet, you can answer below:
Question of the week:
What is a common educator or provider barrier to care for the LGBTQ population?
Answer Choices:
- Being aware of personal biases.
- Understanding those in a same-sex relationship may be concerned how an illness or its treatment will have on fertility.
- Knowing that all people seeking care may wish to discuss relationship issues.
- Assuming person is straight or belongs to the LGBTQ population.
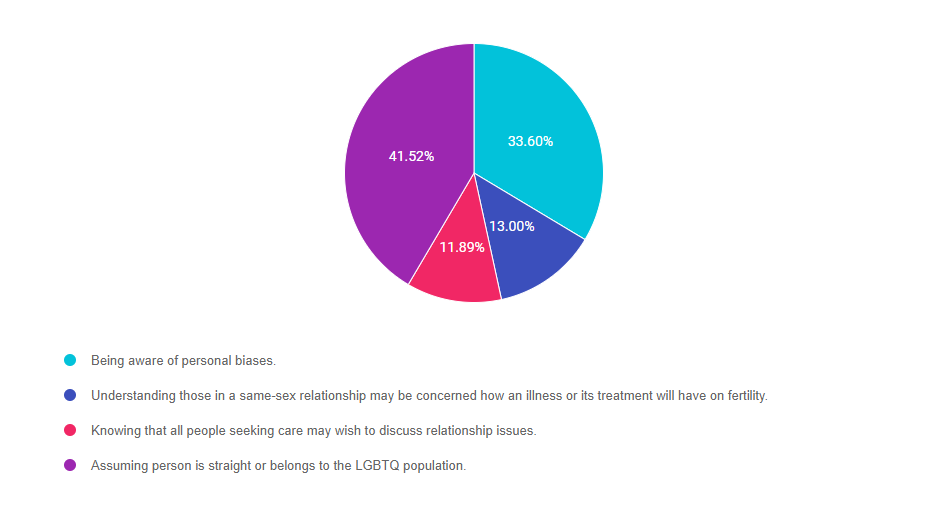
As shown above, the most common choice was option 4, the second most common answer was option 1, then option 2, and finally option 3.
Option 1 is incorrect. Being aware of our personal bias is not a barrier. It helps us to explore and be cognizant of our personal beliefs.
Option 2 is incorrect. This answer considers that the same sex couple may be interested in pursuing having children. In addition, this response shows the educator or provider is aware this is a barrier.
Option 3 is incorrect. People in the LBGTQ community may want the opportunity to discuss relationship issues as it allows them to feel respected as a person, get your support and understanding as to how their social structure relates to their diabetes care.
Option 4 is the correct answer. Assuming a person is straight or belongs to the LGBTQ population is a common barrier to providing person-centered care. Learn more about effective communication in our January Newsletter with our guest contributor, Ms. Theresa Garnero.
We hope you appreciate this week’s rationale and keep studying hard! Thank you so much for taking the time to answer our Question of the Week and participate in this fun learning activity!
Footer 1
Garnero, T. L. (2010) Providing Culturally Sensitive Care for LGBT with Diabetes. Diabetes Spectrum, 23(3): 178-182. https://doi.org/10.2337/diaspect.23.3.178
Sign up for Diabetes Blog Bytes – we post one daily Blog Byte from Monday to Friday. And of course, Tuesday is our Question of the Week. It’s Informative and FREE! Sign up below!
[yikes-mailchimp form=”1″]Ask an Expert: Stress and Diabetes
Our body responds to stress by releasing hormones that increase glucose levels to provide muscles with the fuel they need to engage in battle. This system works well if you don’t have diabetes. However, for people living with insulin deficiency and /or resistance, chronic stress can make glycemic control even more challenging. In addition, stress can cause a detour in the best laid plans to eat healthier and exercise more. Hence, the “Double Whammy” of diabetes and stress.
We asked our special guest contributor to share her expertise on stress and provide us with some coping strategies we can pass along to our patients. Thanks Cathy!
How does daily stress impact people?
Most adults experience some level of stress on a daily basis. Everything from the minor annoyance of a traffic jam to the life-altering commitment of caring for a chronically ill family member can lead to the familiar feelings of uneasiness, muscle tension, difficulty concentrating, changes in sleep and appetite, irritability, headaches, gastrointestinal problems, increased heart rate, trembling, and even feeling faint. Stress affects the physical functioning of the body as well as common behaviors, making it particularly challenging for people with diabetes.
How does stress increase blood glucose levels?
When faced with a stress or danger, the body initiates an immediate and well-coordinated fight or flight response that allows
a person to fight the danger or flee it. Stress hormones, like adrenaline and cortisol, are released causing an elevation in glucose levels. In people without diabetes, this glucose surge is beneficial; it provides energy for muscles to fight off the danger or to outrun it. The system is based on the assumption that the extra glucose will be spent while conquering the dangerous situation, allowing the body to return to a normal (baseline) state. For centuries this system has allowed humans to always be ready to handle threats to their survival.
How have the effects on stress impacted human’s overtime?
It’s rare for modern stressors to require physical fighting or fleeing. Stressors are more often encountered while sitting still — paying bills, sitting in traffic, working at a desk, or having a difficult conversation. Unfortunately the fight or flight response is so ingrained and automatic that it does not allow for differentiation between stress that requires action and stress that requires other types of responses. If the stressor does not necessitate the use of muscles, glucose levels can climb in the bloodstream stimulating the pancreas to increase insulin release.
What is the impact of stress on people with diabetes?
Stress has a dual effect on diabetes. Life stressors can affect behavior by influencing decision-making abilities (such as snacking on unintended foods or skipping exercise). Plus, stress activates the body’s fight or flight response increasing glucose levels circulating in the blood. Recognition of the double impact of stress on individuals with diabetes highlights the need for effective stress management as an integral part of diabetes management programs.
What are some tools that Diabetes Educators can share?
Several techniques can be employed to help alleviate stress. Perhaps the most important skill is to learn to identify stressors. Often individuals report feeling weighed down and stressed out. It can be surprisingly difficult to pinpoint the causes of those feelings. However, taking some time to discuss them with another person can be helpful in naming the stress-causing demands on their lives. Once identified, one can work to lessen or eliminate the stress or to increase their ability to manage the stress.
There are numerous effective ways to reduce feelings of stress, making it possible to find a technique that fits into the lifestyle and values of the individual who will be using it. An active, energetic person might find that exercise is a great stress-reducer. Alternatively, a person who values calm and quiet may prefer taking several slow, deep breaths to encourage relaxation.
Several relaxation techniques, such as progressive muscle relaxation (PMR), meditation, journaling and guided imagery, have actually been shown to reduce glucose levels in people with diabetes in addition to reducing feelings of stress. There are many books and internet resources available that can provide more detail or instruction on these techniques. In some cases, individuals find it helpful to enlist the help of a therapist who is trained in ways to help reduce stress and change thought patterns.
While no one likes the feeling of stress, it’s clear that it is especially detrimental to those with diabetes. Featuring stress management in diabetes management programs can bring about positive changes psychologically as well as physically.
Special thanks to our guest contributor, Cathy A. Bykowski, from Tampa, Florida. Her research and clinical interests revolve around the relationship between mental and physical health, and in particular, how psychological factors affect diabetes outcomes. She is actively recruiting participants for her FREE Stress and Mood Management Program to complete her PhD. Please share this valuable resource with your patients.
Ask An Expert
In our Ask an Expert series, Beverly Thomassian answers commonly asked patient questions.
Help! I’m an over-corrector
Anytime I have a blood sugar low, I take it as license to eat. Muffins, chocolate, pizza—you name it. As a result, I gained 8 pounds last year! How can I tame this habit?
First, if you are getting low blood sugars a few times a month, it could be a sign you are taking more diabetes medication than you need. Talk to your provider about decreasing your diabetes medication dose. If that’s not the case, then try and follow the 15 -15 rule: If your blood sugar is less than 70, try to limit yourself to only eating 15 grams of carbohydrate and then recheck blood sugar in 15 minutes and if still below 70, eat 15 more grams. Have preplanned 15 gram carb snacks easily available such as; small box of raisins, an apple, a 6oz juice box.
Guilty and down in the dumps
Type 2 diabetes runs in my family. For the last two years, my doctor has told me to lose 25 pounds because my blood sugars put me in the pre-diabetes range. Well, now I have full-blown type 2. I feel guilty and depressed. How can I find the motivation to do what I need to do?
Start by giving yourself permission to let go of the past. Be encouraged that even though you have diabetes, you can still have a healthy life. Starting today, write a list of what brings you joy in your life. This “joy list” can be used to light your spark of motivation and encourage small changes in your activity level and eating habits. Commit to making one change that you can realistically accomplish. For example, “I will drink water instead of soda” or “I will get up and move every hour”. Also meeting with a diabetes educator or attending a support group can be very helpful.
Confused about “good” and “bad” foods
I’m newly diagnosed with type 2 and confused: I thought I would have to cut out sugar. But my diabetes educator tells me no foods are off limits. Isn’t the sugar in foods making by blood sugar levels high?
Yes, you can eat foods with sugar, you just have watch portion sizes and not eat too much at one time – a strategy called “carb counting”. Many starchy foods are healthy and are full of nutrients and fiber, even though they are broken down to sugar in your blood. These include fruits, whole grains, milk, beans and starchy vegetables (potatoes, corn etc.). Other carb sources such as desert and snack foods, offer less nutritional value, so they would be considered a special treat to enjoy on occasion. And if possible, avoid sugary drinks and sodas to help with weight and blood sugar control.
How to spot a stroke
F.A.S.T. is an easy way to remember the sudden signs of stroke. When you can spot the signs, you’ll know that you need to call 9-1-1 for help right away. F.A.S.T. is:
Download Infographic on Stroke and App here >>
F | Face Drooping – Does one side of the face droop or is it numb? Ask the person to smile. Is the person’s smile uneven? |
A | Arm Weakness – Is one arm weak or numb? Ask the person to raise both arms. Does one arm drift downward? |
S | Speech Difficulty – Is speech slurred? Is the person unable to speak or hard to understand? Ask the person to repeat a simple sentence, like “The sky is blue.” Is the sentence repeated correctly? |
T | Time to call 9-1-1 – If someone shows any of these symptoms, even if the symptoms go away, call 9-1-1 and get the person to the hospital immediately. Check the time so you’ll know when the first symptoms appeared. |
Beyond F.A.S.T. – Other Symptoms
- Sudden NUMBNESS or weakness of face, arm, or leg, especially on one side of the body
- Sudden CONFUSION, trouble speaking or understanding speech
- Sudden TROUBLE SEEING in one or both eyes
- Sudden TROUBLE WALKING, dizziness, loss of balance or coordination
- Sudden SEVERE HEADACHE with no known cause
My Stroke of Luck
 April 27, 2016 started out as a usual morning. Rushing to get the kids ready for school, preparing breakfast and writing my to-do list for the day.
April 27, 2016 started out as a usual morning. Rushing to get the kids ready for school, preparing breakfast and writing my to-do list for the day.
That’s when I noticed something was wrong. I kept trying to write my list, but the words on the paper did not match the words in my head. I gave up on that project and moved on to talking to the kids, making sure they were ready for school. But, I couldn’t assign the right words to my instructions. I called bread, butter. I couldn’t remember the word for egg. I stuttered. Then I started crying and said, “I think I am having a stroke”.
My 14-year-old son Robert, jumped up, got the phone and called my husband, a pharmacist who works at a nearby hospital and stroke center. My husband, Chris, frantically told Robert to, ‘call 911 and get your mom to the hospital NOW”.
I grabbed the phone from Robert and reassured my husband that I was fine and I did not need an ambulance. I hung up and hurried my 3 kids into the car, worried they would be late for school. As I drove them to their 3 different destinations, I tried retelling them news events that had happened earlier that day, to prove to them I was fine.
After all, I was only 52 and super healthy.
During that 20-minute kid drop of route, my husband called me at least 6 times. He kept commanding that I come to the hospital NOW. The entire stroke team was waiting for me.

So Tissue Plasminogen Activator (TPA) was not indicated. TPA a clot buster that is administered to non-hemorrhagic stroke patients within 3 hours of stroke symptoms. I was not the right candidate for this intervention since most of my stroke symptoms had resolved.
Three hours after the event, I was ready to go home. Convinced this was all a mistake since my CT scan, labs and heart rhythm looked good. Why should I waste precious hospital resources with an overnight stay?
The team insisted I stay and wait for the results of the MRI of my brain that was scheduled for the next morning.
I spent the night in the hospital, getting neuro checks every 4 hours, playing with the controls on my bed, keeping a brave face when I told shocked family members and friends of the series of events.

Me and my dad, pictured here, months before his death at 56 from a massive heart attack.
His shortened life was a central motivating force for my healthy lifestyle.
To maintain my best health, I was clocking 55 miles a week of walking, dancing two hours a week, and eating a diet filled with vegetables, fruit, fiber and an occasional glass of red wine. My lifestyle habits put me at low risk for stroke, but my genetics worked against me. Because of my dad’s stroke history, my risk of stroke was triple that of the general population.

At 11 a.m. I was rolled into the noisy, rhythmic banging tunnel of the MRI machine. I imagined the magnetic energy exploring the nooks, crannies and undulations of my white matter, searching for injured brain tissue. An exploration that I was sure, would turn up empty handed.
At 12:40 p.m., the neurologist walked into the room saying he had read the results of my MRI and that I had suffered a stroke in the Wernicke center of my brain. What he said after that, I don’t remember.
He left the room and the tears started pouring from my eyes. The nurse walked in and just sat with me as I shared the news. My husband, who was working in the hospital, flew into the room, breathless from running up three flights of stairs after I texted him to “please come”. He saw my distress and wrapped me in his arms. He whispered a sweet prayer in Armenian, blessing me and asking for Gods healing powers.
Since that day, I feel like I am a slightly different version of myself. If you met me on the street or at a conference, you probably would have no clue of my stroke history. And, according to my family, I am pretty much still the same.

The neurologist explained that I had suffered an ischemic stroke and would need to be on medications (aspirin, Plavix and Lipitor) to prevent another stroke. As I learned during my hospital stay:
There are 3 main types of stroke:
- Ischemic stroke – this occurs due to an obstruction in a brain blood vessel
- Hemorrhagic stroke – when a weakened blood vessel ruptures
- Transient Ischemic attack – caused by a temporary clot
Most of the time, the cause of the stroke can be identified.
However, thirty percent of the time, the cause is not known. This is called a cryptogenic stroke. In cryptogenic stroke, possible culprits include atrial fibrillation, clotting issues, heart malformations, and other inflammatory states. This is the type of stroke I had. For this reason, they will do long term heart monitoring to see if I have silent a-fibrillation and if it is positive, they will need to start me on a Coumadin-like therapy.
In either case, a person who has had a stroke has a 14 to 25% of recurrence within 2 years. To prevent the second event, there is a BIG focus on risk reduction (see below).

Maybe this was my stroke of luck – An early warning sign that forced me to take action to prevent a more debilitating stroke. This event gives me the opportunity to make sure I am doing everything possible to keep healthy through lifestyle and the right medications. After all, my dad had his first stroke at 44 and I didn’t have mine until 52. So maybe all the years I have worked hard to keep healthy have paid off.
Maybe this stroke provided me with a window to share my story with you and my diabetes community to increase awareness and early intervention.

My 14-year-old son wrote me the most touching Birthday Card a few weeks after my stroke. In it he said,
“Mom, you taught me that it’s not what happens to you,
but how you bounce back”.
I love this quote by Anna Quindlen, “The thing that is really hard, and really amazing, is giving up on being perfect and beginning the work of becoming yourself.” I am excited to start on this new journey and thankful for this stroke of luck.
Here is some more info on Signs of Stroke to share with your community!
Ask an Expert – Commonly asked care questions
Diabetes Nurse Specialist Beverly Thomassian provides some answers to commonly asked care questions.
I love fruit, but I’m confused about if it’s okay for me to eat it. It has a lot of sugar and it is a carb. What’s the story?
Fruits contain a natural sugar called fructose, which can raise blood sugars like any other foods containing carbohydrates. But, this doesn’t mean fruits are off limits. We recommend that people with diabetes eat 3 to 4 fruit servings, spread throughout the day. Fruits provide natural energy, fiber, nutrients and support good gut health, plus they are fat free. Here are some examples of one serving of fruit: Small baseball size apple, orange or peach or other stone fruit, 1 ¼ cup strawberries or watermelon, 3 apricots, ½ cup canned fruit, ¾ cup of berries, ½ banana. So enjoy fruit; a completely natural food that nourishes your body.
Sometimes I feel wobbly on my feet, and it’s hard to walk. Could this have anything to do with my diabetes, and if so, what can I do about it?
Balance is a big issue for people living with diabetes, since it can lead to a fall, bone fracture or other problems. There are several potential causes for wobbliness that you can bring up with your provider for evaluation. First, there may be nerve damage to your feet, causing numbness which can make you feel unsteady. Another common cause associated with aging, is the loss of muscle mass and sense of balance. This is more likely to be true in people who sit for long periods of time and don’t move much. The good news is that by becoming more active and doing specific exercises designed for balance, many people feel less wobbly on their feet.
I have type 2 diabetes, I’m a woman, and I weigh 225 pounds. I know I have to lose at least 75 pounds, so why does my doctor say that losing just 5% will help a lot? That’s only about 12 pounds!
There are many studies looking at people living with type 2 diabetes that clearly demonstrate that losing 5-7% of your body weight (no matter how overweight you are) helps your cells respond better to your body’s own insulin and lower blood sugars. When people lose weight, about 30-50% of that weight loss is from the belly fat. This is important, because belly fat releases chemicals that stop insulin from working effectively. Just a 5-7% weight loss burns enough belly fat to make your body’s own insulin work better and help your muscle use sugar for energy. Which translates into lower blood sugars.
My diabetes medications are getting so expensive, but I’m embarrassed to talk with my doctor or diabetes educator about it. Do you have any suggestions?
Many people, like you, are struggling with expensive medication co-pays that are outside their budget. I encourage to ask your pharmacist to see if there are generic or less expensive versions of the medications you are taking. Contact your insurance company and ask if there are any medications in the same “class” that would be less expensive. After doing this research, you can bring the information to your team of providers and/or educators and ask for their help in problem solving. Be reassured, that they want to help you get the medications you need to stay heathy.








