
Our September 28th Question of the week quizzed test takers on the best strategy to prevent hypo in the hospital. 64% of respondents, chose the best answer. We are excited to share info so you can pass on helpful info to people living with diabetes and your hospital colleagues.
Before we start though, if you don’t want any spoilers and haven’t tried the question yet, you can answer below: Answer Question
Question: As a diabetes specialist at a local hospital, one of your quality improvement goals is to prevent nocturnal hypoglycemia.
Which of the of following policy changes would most likely lower rates of overnight and morning hypoglycemia?
Answer Choices:
- Make sure the medication carts are stocked with glucagon rescue kits.
- Eliminate insulin sliding scale and encourage basal insulin therapy.
- Collaborate with dietary to make sure all people with diabetes get protein plus carb snack.
- Implement a plan to decrease basal insulin dose if morning glucose is less than 100 mg/dl.
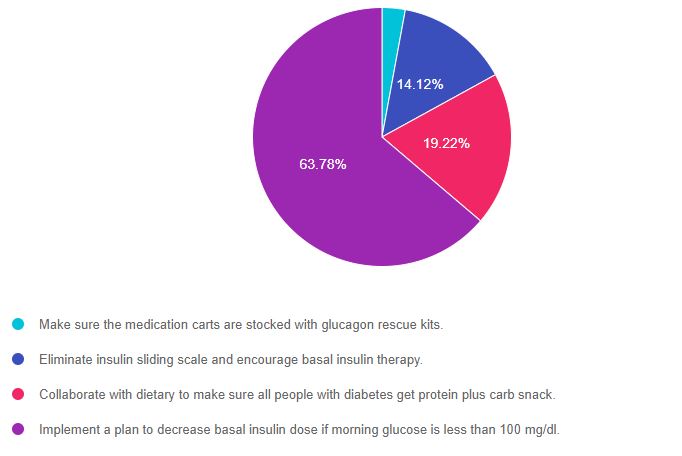
As shown above, the most common choice was option 4, the second most common answer was option 3, then option 2, and finally option 1.
Getting to the Best Answer
If you are thinking about taking the certification exam, it is helpful to know the goals of care and considerations for people with diabetes in the acute care setting. This practice test question will set you up for success. Test writers anticipate possible answers based on the details in the question. They will wave those “juicy answers” that seem so familiar to you, right under your nose. Your job is to weed through the to choose the BEST answer.
Answer 1 is incorrect. 2.88% chose this answer, “Make sure the medication carts are stocked with glucagon rescue kits.” Since the question is asking “what policy changes would most likely lower rates of overnight and morning hypoglycemia“, this is answer does not address the problem in the question; what policy change would PREVENT hypoglycemia. Having glucagon rescue meds would treat hypoglycemia, but not prevent it.
Answer 2 is incorrect. 14.12% of you chose this answer, “Eliminate insulin sliding scale and encourage basal insulin therapy.” It is true that the ADA does not recommend insulin sliding scale for inpatient management of diabetes since it is not an effective way to manage hyperglycemia. In addition, since sliding scale is usually administered with meals, it is not the most likely culprit causing morning hypoglycemia. Generally speaking, too much basal insulin is usually the cause of morning hypoglycemia. So stopping the sliding scale and encouraging basal insulin, is not the BEST answer to address the question and reduce morning hypoglycemia.
Answer 3 is incorrect. 19.22% of respondents chose this answer, “Collaborate with dietary to make sure all people with diabetes get protein plus carb snack.” Studies have shown that providing a carb snack at bedtime can decrease risk of nocturnal and morning hypoglycemia. But, if the basal insulin dose is too much, the person could still experience hypoglycemia, even with a carb snack. P.S, adding protein has not been shown to sustain the action of the carb and enhance hypoglycemia prevention. We never want to “feed” the insulin. We always want to give the least amount of insulin to get glucose to target and keep people safe.
Finally, Answer 4 is correct. 63.78% chose this answer, “Implement a plan to decrease basal insulin dose if morning glucose is less than 100 mg/dl.” YES, this is the BEST Answer. GREAT JOB. To keep inpatients safe, creating a policy that notifies the medical team when the morning glucose level is less than 100 mg/dL coupled with a reduction of basal insulin dose, would be an effective strategy to prevent morning hypoglycemia.
We hope you appreciate this week’s rationale! Thank you so much for taking the time to answer our Question of the Week and participate in this fun learning activity!
Enroll in our Virtual DiabetesEd Specialist Program!
Did you miss the live conference? No worries!
You can register now to watch on-demand
Click here to learn more and get started!
Whether you are new to diabetes or a seasoned expert, you’ll benefit from this virtual conference with the latest research plus critical content that you can immediately apply to your clinical practice.
If you are seeking a state-of-the-art review of current diabetes care, this course is for you. Our team has been fine-tuning this course for over fifteen years, and we know what you need. This program can also be a great addition to your CDCES or BC-ADM exam study plan.
Team of expert faculty includes:
- Diana Isaacs, PharmD, BCPS, BC-ADM, BCACP, CDCES – Educator of the Year, 2020
- Coach Beverly Thomassian, RN, MPH, CDCES, BC-ADM
- Ashley LaBrier, MS, RD, CDCES, Diabetes Program Coordinator
In addition to informative lectures, we also use group activities and case studies to highlight the essential knowledge, skills, and strategies needed to succeed in diabetes education today!
CEs: Includes over 30 CEs
Program Info: 2021 Diabetes Educator Course Flyer & Schedule (subject to change)
Speakers: View Conference Faculty.
Dates: Your registration fee includes access to FREE podcast and all recorded webinars for one year.
Virtual DiabetesEd Specialist Conference Deluxe | Recorded & Ready for Viewing! | 30+ CEs
Deluxe Virtual Program for $459 includes:
- Presentations by our team of experts
- Q & A Session with the instructor after each webinar
- State-of-the-art review of current diabetes care and technology.
- Resources for each session
- Access to FREE podcast and recorded webinars within a week of each live session for one full year.
+Plus Syllabus, Standards and Swag:
- Diabetes Educator Course 2021 Syllabus Hard Copy – over 100 pages -This spiral-bound workbook contains the printed version of all of the instructor’s slides.
- DiabetesEd Services highlighters, Medication PocketCard and Pen
2021 Diabetes Educator Course Flyer & Schedule (subject to change)
Team of Experts: Our team of expert faculty has been fine-tuning this course for over fifteen years and we know what you need to succeed! In addition to informative lectures, we also use group activities and case studies to highlight the essential knowledge, skills, and strategies needed to succeed in diabetes education today!
Bonus Courses worth 12+ CEs, FREE
When you register for our Virtual Course, you have immediate access to these Bonus DiabetesEd University Online Courses – for FREE!
- Test Taking Toolkit – Over 200 sample test questions!
- Level 2 – Assessing and Promoting Well-Being: From Population Health to a Person-Centered Approach 1.5 CEs
- Level 2 – Hospital and Hyperglycemia 1.5 CEs
- Level 2 – Hyperglycemic Crisis, DKA and HHS Standards 1.0 CEs
- Level 2 – Meds Management Update for Type 2 – 1.5 CEs
- Level 2 – Setting up a Successful Diabetes Program 1.5 CEs
- Level 2 – Pregnancy and Diabetes 1.5 CEs
- Level 2 – From Tots to Teens – Diabetes Standards 1.5 CEs
- Level 2 – Older Adults and Diabetes 1.5 CEs
- Mindfulness and Compassion in the Diabetes Encounter – 1.0 CE
2021 Diabetes Educator Course Flyer & Schedule (subject to change)
Sign up for Diabetes Blog Bytes – we post one daily Blog Byte from Monday to Friday. And of course, Tuesday is our Question of the Week. It’s Informative and FREE! Sign up below!
[yikes-mailchimp form=”1″]Accreditation: Diabetes Education Services is an approved provider by the California Board of Registered Nursing, Provider 12640, and Commission on Dietetic Registration (CDR), Provider DI002. Since these programs are approved by the CDR it satisfies the CE requirements for the CDCES regardless of your profession.*
The use of DES products does not guarantee the successful passage of the CDCES exam. CBDCE does not endorse any preparatory or review materials for the CDCES exam, except for those published by CBDCE.









