
For last week’s practice question, we quizzed test takers on the new ADA/EASD Standards. 56% of respondents chose the best answer. We want to clarify and share this important information, so you can pass it on to people living with diabetes and your colleagues, plus prepare for exam success!
Before we start though, if you don’t want any spoilers and haven’t tried the question yet, you can answer it below: Answer Question
Question:
The new ADA /EASD Management of Hyperglycemia in Type 2 Consensus Statement 2022 was just released.
Which of the following is an accurate recommendation according to these updated guidelines?
Answer Choices:
- Initiate treatment with metformin for most individuals, including those with cardiovascular disease.
- If A1C not at target with 2 or more oral agents, add on basal insulin therapy.
- Avoid the use of SGLT-2 Inhibitors in those with an eGFR of less than 25.
- Prioritize the use of organ protective medications in those with cardiorenal disease.
Getting to the Best Answer
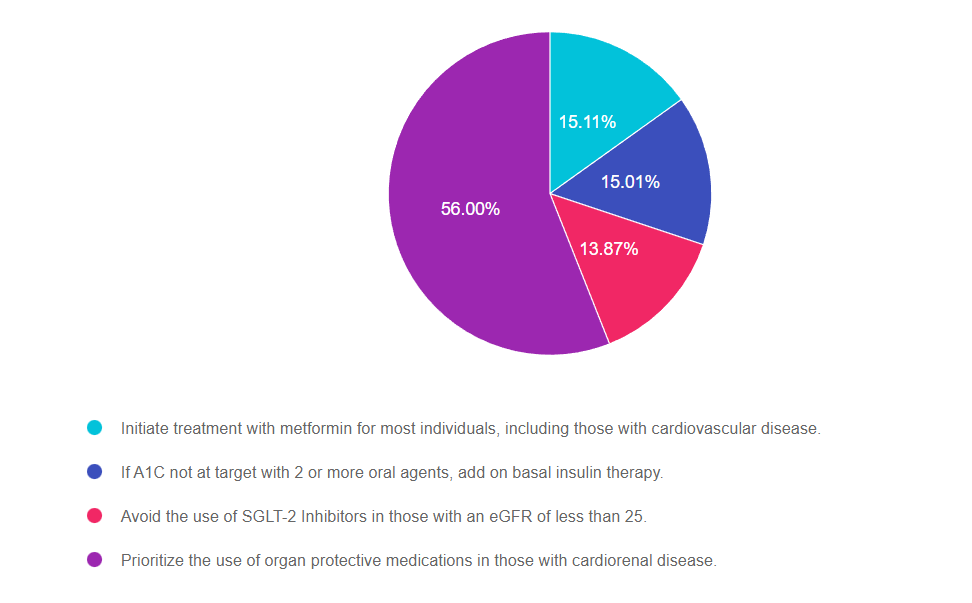
Answer 1 is incorrect. 15.11% chose this answer, Initiate treatment with metformin for most individuals, including those with cardiovascular disease.” In the past, this would have been the best answer, but based on latest guidelines, metformin is no longer the only first treatment. Based on the individual and our risk assessment (ie heart or renal failure or elevated CV risk) we could choose a SGLT-2 or GLP-1 as first line therapy.
Answer 2 is incorrect. 15.01% of you chose this answer, If A1C not at target with 2 or more oral agents, add on basal insulin therapy.” With the guidelines, they strongly suggest starting a GLP-1 RA before starting basal insulin as the first choice if possible. GLP-1 is preferred since insulin therapy is associated with hypoglycemia and weight gain, while the GLP-1’s is associated with weight loss, CV risk reduction and no hypoglycemia.
Answer 3 is incorrect. 13.87% of respondents chose this answer, “Avoid the use of SGLT-2 Inhibitors in those with an eGFR of less than 25.” This is a juicy answer, but the new guidelines encourage the use of SGLT-2 Inhibitors in people with diabetes with a GFR of 20 or greater, stopping SGLT-2 therapy when dialysis is started. Even with stage 3 & 4 kidney failure, SGLT-2’s can effectively slow the progression of kidney disease and improve CV outcomes in people with diabetes.
Finally, Answer 4 is correct. 56.00% chose this answer, Prioritize the use of organ protective medications in those with cardiorenal disease.” YES, GREAT JOB. This is the best answer. We are encouraged to target therapy based on the individual and to protect organs. For people with renal and heart failure, SGLT-2’s are the preferred class and for people with CV disease, starting either a GLP-1 or SGLT-2 decreases risk of major adverse cardiovascular events (MACE). We hope you can join our webinar on December 1st to learn more.
Want to learn more about this question? Join us for our
Meds for Type 2 Update; New ADA/EASD Consensus Statement
Level 2 | 1.25 CEs
Airs live on Wednesday, December 1st at 11:30 am PST

Plan on joining this exciting webinar that walks participants through the newly released, “Management of Hyperglycemia in Type 2 Consensus Report by the ADA and EASD”. These updated guidelines will be incorporated into the 2023 ADA Standards of Care, but you can get a early sneak peak by joining Coach Beverly on December 1st, 2022. She will highlight the revised guidelines with a focus on new elements and exciting changes on how we approach medication management for type 2 diabetes. Together, we will explore clinical factors to consider when determining the best strategy to improve glucose management in people with type 2 diabetes and other co-conditions. There will be a special focus on cardiovascular risk reduction and renal protection and addressing clinical inertia.
Objectives:
- Describe the role of Diabetes Care and Education Specialists in advocating for optimal therapeutic approaches.
- Discuss the application of the new ADA/EASD Guidelines to improve glucose and reduce CV and renal risk.
- List strategies to initiate and adjust oral and injectable therapy using a person-centered approach
Intended Audience: A great course for health care professionals seeking evidence-based information that improves the quality of life and outcomes.
Don’t worry if you can’t make it live. Your registration guarantees access to the recorded version in the Online University.
All hours earned count toward your CDCES Accreditation Information
Sign up for Diabetes Blog Bytes – we post one daily Blog Byte from Monday to Friday. And of course, Tuesday is our Question of the Week. It’s Informative and FREE! Sign up below!
The use of DES products does not guarantee the successful passage of the CDCES exam. CBDCE does not endorse any preparatory or review materials for the CDCES exam, except for those published by CBDCE.









