
For last week’s practice question, we quizzed participants on Diabetes and NASH. 41% of respondents chose the best answer. We want to clarify and share this important information, so you can pass it on to people living with diabetes and your colleagues, plus prepare for exam success!
Before we start though, if you don’t want any spoilers and haven’t tried the question yet, you can answer it below: Answer Question
Question:
The provider referred RT, a 72-year-old with type 2 diabetes and non-alcoholic fatty steatohepatitis (NASH), for an appointment with the diabetes care and education specialist. RT is frightened because their brother died of liver cancer.
Which of the following is the most accurate statement regarding NASH and diabetes?
Answer Choices:
- NASH is when intrahepatic fat is equal to or greater than 5% of liver weight.
- About 30% of people with diabetes and extra weight also have NASH.
- There are standardized medication algorithms to guide the treatment of NASH.
- Risk of NASH is greater in people who consume excess alcohol and processed foods.
Getting to the Best Answer
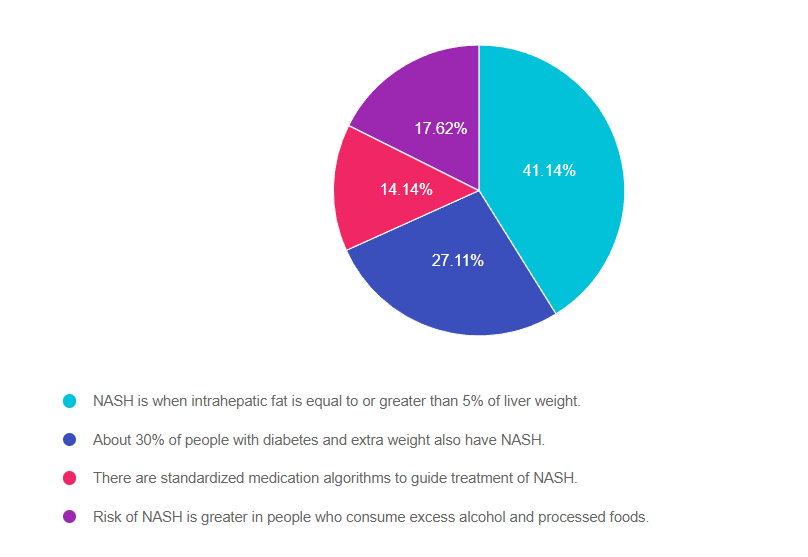
Answer 1 is correct. 41.14% chose this answer, “NASH is when intrahepatic fat is equal to or greater than 5% of liver weight.” GREAT JOB! According to ADA Standard 4, “NASH is defined histologically as having more than 5% hepatic steatosis and associated with inflammation and hepatocyte injury (hepatocyte ballooning), with or without evidence of liver fibrosis”.
Answer 2 is incorrect. 27.11% of you chose this answer, “About 30% of people with diabetes and extra weight also have NASH.” This is a juicy answer, but it is an underestimate of the current problem. Recent studies in adults in the U.S. estimate that more than 70% of people with type 2 diabetes have non alcoholic fatty liver disease (NAFLD). The more serious, steatohepatitis, is estimated to affect more than 50% of people with type 2 diabetes with NAFLD and it appears to be a driver for the development of fibrosis.
Answer 3 is incorrect. 14.14% of respondents chose this answer, “There are standardized medication algorithms to guide the treatment of NASH.” According to ADA Standard 4, at present, there are no FDA-approved drugs for the treatment of NASH. Therefore, treatment for people with type 2 diabetes and NASH is centered on the dual purpose of treating hyperglycemia and weight loss. Pioglitazone and some glucagon-like peptide 1 receptor agonists (GLP-1 RAs) have been shown to be effective to treat steatohepatitis, may slow fibrosis progression, and decrease cardiovascular disease.
Finally, Answer 4 is incorrect. 17.62% chose this answer, “Risk of NASH is greater in people who consume excess alcohol and processed foods.” Nonalcoholic steatohepatitis [NASH] indicates liver inflammation in the absence of ongoing or recent consumption of significant amounts of alcohol (defined as ingestion of >21 standard drinks per week in men and >14 standard drinks per week in women over a 2-year period preceding evaluation) or the presence of other secondary causes of fatty liver disease. NASH is not a result of excess alcohol intake and is usually associated with genetics, body weight and insulin resistance.
Thank you so much for reading this “Rationale of the Week”.
We also invite you to join our Online Courses for more information (see info below)
Hope you can join our Diabetes Boot Camp in February and our other Level 2 Courses.
Preparing for Diabetes Certification Exam? Enroll in our Level 3 – Boot Camp 2023 Updates
Level 3 | DiabetesEd Specialist Boot Camp | 12+ CEs

Can’t join all the sessions live? No problem. Your registration guarantees you access to the recorded lectures for a full year.
This bundle is specifically designed for healthcare professionals who are studying for the Board Certified in Advanced Diabetes Management (BC-ADM) or the Certified Diabetes Care and Education Specialist (CDCES) certification exam.
Intended Audience: This library of critical information is designed for individuals or groups of diabetes specialists, including RNs, RDs, Pharmacists, Nurse Practitioners, Clinical Nurse Specialists, Physician Assistants, and other health care providers interested in staying up to date on current practices of care for people with diabetes and preparing for the BC-ADM or the CDCES certification Exam.
2023 Webinar Updates
- February 7, 2023 – Class 1 – Diabetes – Not Just Hyperglycemia 1.75 CEs
- February 9, 2023 – Class 2 – Standards of Care & Cardiovascular Goals 1.8 CEs
- February 14, 2023 – Class 3 – Meds for Type 2 – What you need to know 1.5
- February 16, 2023 – Class 4 – Insulin Therapy – From Basal/Bolus to Pattern Management 1.5 CEs
- February 21, 2023 – Class 5 – Insulin Intensive – Monitoring, Sick Days, Lower
- February 23, 2023 – Class 6 – Exercise and Medical Nutrition Therapy 1.5 CEs
- February 28, 2023 – Class 7 – Screening, Prevention, and Treatment of Microvascular Complications
- March 2, 2023 – Class 8 – Coping and Behavior Change 1.5 CEs
- March 9, 2023 – Class 9 – Test-Taking Coach Session (48 Questions) No CE
All hours earned count toward your CDCES Accreditation Information
Sign up for Diabetes Blog Bytes – we post one daily Blog Byte from Monday to Friday. And of course, Tuesday is our Question of the Week. It’s Informative and FREE! Sign up below!
The use of DES products does not guarantee the successful passage of the CDCES exam. CBDCE does not endorse any preparatory or review materials for the CDCES exam, except for those published by CBDCE.









