For last week’s practice question, we quizzed participants on assessing risk factors for hypoglycemia. 69% of respondents chose the best answer. We want to clarify and share this important information, so you can pass it on to people living with diabetes and your colleagues, plus prepare for exam success!
Before we start though, if you don’t want any spoilers and haven’t tried the question yet, you can answer it below: Answer Question

Question: LM has had type 2 diabetes for over 30 years and takes 1000 mg metformin BID, 30 units of glargine at bedtime, 25 mg empagliflozin, as well as daily lisinopril and lovastatin. A1c was 7.2%, LDL: 56, and eGFR was 38 mL/min/1.73m2 last visit. CGM ambulatory glucose profile report indicates a time in range of 71%, time below range of 4%, and time above range of 25%. LM reports living on a fixed income, relying on social security, and an increase in recent financial stress. They are concerned they may not have enough money to purchase foods by the end of the month.
Select the best answer considering LM’s potential risk factors for hypoglycemia?
Answer Choices:
- LM has chronic kidney disease, and we note he is taking an ACE and SGLT-2
- Basal insulin therapy alone.
- Income status.
- All the above.
Getting to the Best Answer
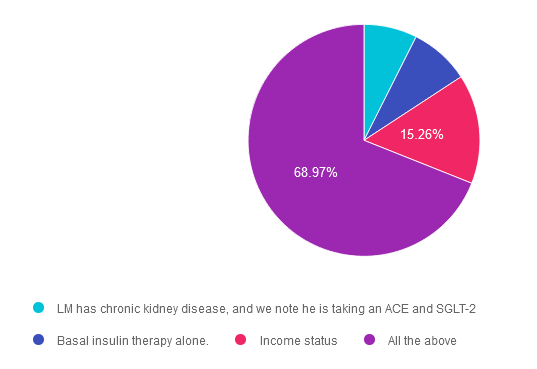
Answer 1 is incorrect. 7.42% chose this answer. “LM has chronic kidney disease, and we note he is taking an ACE and SGLT-2.” Answer 1 is somewhat true but is not the best answer. We may consider this question incorrect due to the statement that LM is taking ACE and SGLT-2 medications, and we know these have a low risk of hypoglycemia. However, a diagnosis of CKD, especially along with basal insulin therapy, can be a factor that increases hypoglycemia risk. If LM’s GFR was below 15 with a diagnosis of end-stage renal disease, then we would consider this a major risk factor. Let’s keep reading for the best answer.
Answer 2 is incorrect. 8.36% of you chose this answer. “Basal insulin therapy alone.” Answer 2 is also true but is not the best answer. Hypoglycemia risk is highest in individuals treated with intensive insulin therapy followed by basal insulin and then sulfonylureas.1 Basal insulin therapy is a risk factor for hypoglycemia, and we may be tempted to select this answer alone. However, other considerations also impact LM’s risk for hypoglycemic events while on basal insulin therapy.
Answer 3 is incorrect. About 15.26% of respondents chose this. “Income status.” Answer 3 is also true but is not the best answer. Income status and food insecurity are considered risk factors for hypoglycemia and are associated with increased hospital admissions and ER visits. However, we must also consider this along with medication treatment. Food insecurity along with LM’s basal insulin therapy is a major risk factor for hypoglycemia.
Finally, Answer 4 is correct. 68.97% chose this answer. “All the above.” Answer D is the correct Answer. The 2024 Standards of Care recommends hypoglycemia assessment at every clinical visit. We can use validated tools to determine risk for hospital admission or an ER visit, but these do not consider every risk factor. It is important to consider not only clinical factors but also social, economic, and cultural factors. Risk stratification is for all individuals treated with insulin, sulfonylureas, or meglitinides. ° American Diabetes Association Professional Practice Committee; 6. Glycemic Goals and Hypoglycemia: Standards of Care in Diabetes—2024. Diabetes Care 1 January 2024; 47 (Supplement_1): S111–S125. https://doi.org/10.2337/dc24-S006
We hope you appreciate this week’s rationale! Thank you so much for taking the time to answer our Question of the Week and participate in this fun learning activity!
Want to Learn more about recognizing and addressing Diabetes Distress?
Join us live on June 17th & June 24th, 2024 for our
ReViVE 5 Diabetes Training Program:
Unlocking Hidden Barriers to Diabetes Management
“ReVive 5” breathes new life into our relationship with diabetes, bringing a fresh perspective to both the person with diabetes and the provider.
The ReVive 5 program is built on sound research from the Embark Trial and will revolutionize your approach to diabetes self-management education.
We have reassembled the Embark training team and created a resource binder of fantastic tools that we are excited to share with you in our ReVive 5 Diabetes Training Program. You are invited to join us to learn a step-wise, proven approach to addressing hidden barriers to diabetes self-management and glucose management.
You don’t need to be mental health expert or diabetes technology wiz to join this training or to integrate these new strategies into your daily practice.
ReVive 5 uses an integrated, evidence-based approach that provides health care professionals with a realistic 5-step approach to addressing the whole person, starting with emotional distress and incorporating a unique, but integrated approach to problem-solving glucose management difficulties.
Intended Audience: This library of critical information is designed for individuals or groups of diabetes specialists, including RNs, RDs, Pharmacists, Nurse Practitioners, Clinical Nurse Specialists, Physician Assistants, and other health care providers interested in staying up to date on current practices of care for people with diabetes and preparing for the CDCES or BC-ADM Certification Exams.
Can’t join live? That’s okay. Your registration guarantees you access to the recorded version of the series, along with podcasts and resources for one full year.
Accredited Training Program:
- 15+ CEs – Includes the 7-hour ReVive 5 Training Program, Certificate, and 5 FREE bonus courses to supplement content.
- A comprehensive set of assessment tools, educational materials, log sheets, and resources.
Join us to gain the confidence and learn the skills needed to support people with diabetes to move forward in their self-management and discover the expert within.
Team of Experts:
ReVive 5 is taught by a team of 3 Interdisciplinary Experts:
- Lawrence Fisher, Ph.D., ABPP, Professor Emeritus, UCSF
- Susan Guzman, PhD
- Beverly Thomassian, RN, MPH, CDCES, BC-ADM
Speakers Interviews – Learn more about the ReVive 5 Team
Sign up for Diabetes Blog Bytes – we post weekly Blog Bytes that are informative and FREE! Every week we post one exam practice Question of the Week and Rationale of the Week. Sign up below!
Accreditation: Diabetes Education Services is an approved provider by the California Board of Registered Nursing, Provider 12640, and our CPEU courses have received Prior Approval* from the Commission of Dietetic Registration (CDR), Provider DI002. Since our CPEU courses received Prior approval* from the CDR, these CPEU courses satisfy the CE requirements for the CDCES /BC-ADM regardless of your profession!
The use of DES products does not guarantee the successful passage of the certification exam. CBDCE and ADCES do not endorse any preparatory or review materials for the CDCES or BC-ADM exams, except for those published by CBDCE & ADCES.









