Staging For Cardiovascular-Kidney-Metabolic (CKM) Syndrome
New Blood Pressure Target and Intervention
If you are taking the CDCES or BC-ADM exam in 2023, these new blood pressure target recommendations and treatment interventions are important to know.
For all of us who serve people with diabetes, research suggests that these more intensive blood pressure targets will save lives and decrease CV and microvascular disease. By sharing this information with our colleagues and teams, we can be a part of improving outcomes and quality of life.
The following content summarizes the 2023 updated ADA guidelines as outlined in Standard 10 – Cardiovascular Disease and Risk Management.
New Hypertension Definition and Target of 130/80

- A person with diabetes who has a confirmed blood pressure reading of 130/80 or greater (with either a systolic reading greater than 130 or diastolic reading greater than 80) qualifies for antihypertensive drug therapy.
- The on-treatment target blood pressure goal is less than 130/80 if it can be safely attained.
- It is important to individualize blood pressure targets through shared decision-making process. Consider cardiovascular risk, potential adverse effects of antihypertensive medications, and individual preferences.
- All people with diabetes and hypertension need to have a home blood pressure monitor for ongoing evaluation of treatment response.
Lowering Blood Pressure Saves Lives and Reduces CV Risk.
Randomized clinical trials have unequivocally demonstrated that getting blood pressure to target saves lives and reduces risk of cardiovascular and microvascular complications.
The recommendation to support a blood pressure goal of <130/80 in people with diabetes is consistent with guidelines from the American College of Cardiology and American Heart Association (20), the International Society of Hypertension (21), and the European Society of Cardiology (22).
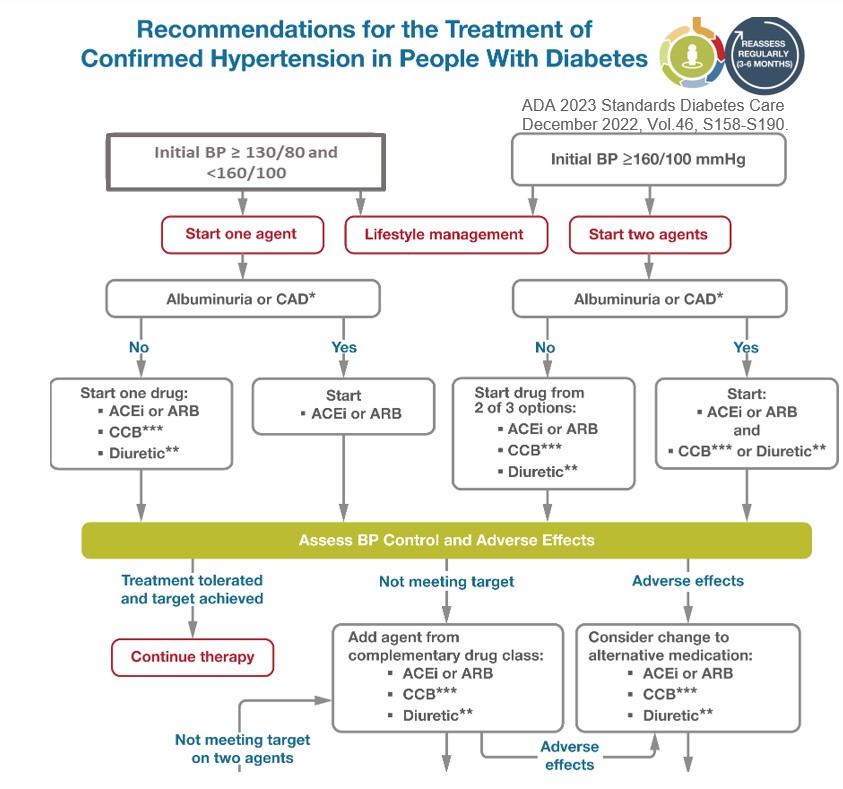
Action Steps to Treat Hypertension
- Lifestyle interventions for people with blood pressure >120/80 include weight loss when indicated, a Dietary Approaches to Stop Hypertension (DASH)-style eating pattern including reducing sodium and increasing potassium intake, moderation of alcohol intake, and increased physical activity.
- Pharmacologic therapy is initiated for individuals with confirmed office-based blood pressure of 130/80 or greater to achieve the recommended blood pressure target of <130/80.
- Treat hypertension with drug classes demonstrated to reduce cardiovascular events in people with diabetes. ACE inhibitors or angiotensin receptor blockers (ARBs) are recommended first-line therapy for hypertension in people with diabetes and coronary artery disease and/or for those with a urinary-albumin-creatinine ratio of 30 mg/g or greater. (Do not combine ACE Inhibitors and ARBS)
- Monitor potassium levels and GFR for individuals treated with an ACE inhibitor, angiotensin receptor blocker, or diuretic.
Hypertension Medication Cheat Sheets
Keeping track of medications for hypertension and cholesterol can seem daunting. We have put together a Hypertension and Lipid Medication Cheat Sheet along with summary information for each class that is important to know for certification exams and is very useful in clinical practice.
Hypertension and Lipid Medication Cheat Sheet
Blood Pressure Matters
Together, we can improve the quality of life and outcomes for people living with diabetes. Getting blood pressure to target is one of the most important interventions we can take to maintain health. Thank you for reading this article and advocating for the best evidence-based care.
Want to learn more about this question? Join us for our
Level 2 | ADA Standards of Care CE Course | 2.0 CEs
Updates air live between Feb. 2, 2023, at 11:30 am PST
This course, updated annually, is an essential review for anyone in the field of diabetes. Join Coach Beverly as she summarizes the 2023 updates to the American Diabetes Association’s Standards of Medical Care in Diabetes and provides critical teaching points and content for healthcare professionals involved in diabetes care and education.
Objectives:
- List significant changes and updates to the 2023 ADA Standards of Medical Care.
- State 3 updates on new blood pressure and lipid goals.
- Identify 5 key elements of the position statement.
- Discuss how to apply the Standards in the clinical setting and in preparation for exam success.
Intended Audience: This course is a knowledge-based activity designed for individuals or groups of diabetes professionals, including RNs, RDs, Pharmacists, Nurse Practitioners, Clinical Nurse Specialists, Physician Assistants, and other health care providers interested in staying up to date on current practices of care for people with prediabetes, diabetes and other related conditions.
Don’t worry if you can’t make it live. Your registration guarantees access to the recorded version in the Online University.
All hours earned count toward your CDCES Accreditation Information
Studying for the CDCES Exam? Enroll in our
CDCES Deluxe Prep Bundle | 30+ Online Courses + Bonus Items | 47 CEs
This bundle includes our CDCES Online Prep Bundle (featured above) plus the ADCES Review Guide – 5th Edition-Revised. The online bundle includes Level 1, Level 2, and Level 3 (Boot Camp), plus two bonus courses. The ADCES Review Guide offers over 480+ practice questions and is a fantastic independent study tool and comprehensive resource for the Diabetes Care and Education Specialist Exam.
Included in this bundle
- Level 1 focuses on the fundamentals and introduces each topic area for the exam.
- Level 2 deep dives into the ADA Standards of Care,
- Level 3 AKA Boot Camp is a more accelerated level that focuses on test simulation for finding the best answer to get you to the finish line of your study path.
- Technology Toolkit which gives information on pumps, sensors, and calculations,
- Test Taking Toolkit includes over 220 practice questions for test simulation plus a webinar where Coach Beverly provides test-taking tips based on her experience taking the certification exam six times.
- ADCES Review Guide for the Diabetes Care and Education Specialist Exam – 5th Edition – Revised – The ADCES Review Guide is a fantastic independent study tool and comprehensive resource for the Diabetes Care and Education Specialist Exam. This book includes 480 + multiple-choice questions and strategies for preparing for and taking the exam with an answer key with rationales for all questions!
- Medication PocketCard – Our four-sided medication accordion Pocketcards were designed by Coach Beverly Thomassian to assist in clinical practice and exam preparation.
- Tote Bag
Sign up for Diabetes Blog Bytes – we post one daily Blog Byte from Monday to Friday. And of course, Tuesday is our Question of the Week. It’s Informative and FREE! Sign up below!
The use of DES products does not guarantee the successful passage of the CDCES exam. CBDCE does not endorse any preparatory or review materials for the CDCES exam, except for those published by CBDCE.
Oral Hygiene & Heart Health Link | Mindful Monday

A study done by the department of neurology at Mokdong Hospital at Ewha Womans University College of Medicine in Seoul, South Korea analyzed data from over 160,000 people who had no history of heart failure or atrial fibrillation. Information collected during the study included weight, height, lifestyle questionnaires, lab tests, oral health disease, dental visits in the past year, and oral hygiene behaviors.
All study participants were examined for periodontal disease. Of all participants present, 3% developed atrial fibrillation and 4.9% developed heart failure after a follow up 10.5 years later.
The study found that people who frequently brushed their teeth (3 or more times per day) had a lower risk of heart failure and atrial fibrillation. Getting teeth professionally cleaned also lessened risked of these problems.
More research is needed to see if there is a causal relationship. However, recommending active oral hygiene is always a great idea!
Read more here.
Sign up for Diabetes Blog Bytes – we post one daily Blog Byte from Monday to Friday. And of course, Tuesday is our Question of the Week. It’s Informative and FREE! Sign up below!
[yikes-mailchimp form=”1″]Lower B/P Target and Earlier Treatment for Diabetes?

People with diabetes who delay getting blood pressure to target may be more likely to have heart attacks and strokes than their counterparts who manage it promptly, a recent study suggests.
A study conducted by Dr. Sridharan Raghavan of University of Colorado Anschutz Medical Campus, examined data on over 43,000 participants. Participants were all people with diabetes who started treatment for high blood pressure between 2002 and 2007.
Those who waited until their blood pressure was more elevated before beginning treatment were 10% more likely to have events like fatal heart attacks and strokes.
Raghavan stressed that lowering blood pressure in people with diabetes with hypertension “can mitigate some of the risk of atherosclerotic cardiovascular disease.” The study indicates that people with diabetes may have improved outcomes with a lower systolic blood pressure target than the ADA target of 140 mmHg. The American Heart Associations and the American College of Cardiology’s guidelines are to start treatment when systolic blood pressure is above 130 mmHg.
Using the lower standard of 130 systolic instead of starting treatment at the higher 140 systolic standard may result in fewer deaths from heart attacks and strokes.
Read the full study here.
Sign up for Diabetes Blog Bytes – we post one daily Blog Byte from Monday to Friday. And of course, Tuesday is our Question of the Week. It’s Informative and FREE! Sign up below!
[yikes-mailchimp form=”1″]Happy National Heart Month | Mindful Monday
February is National Heart Month!

This month we want to help our communities lower their risk of heart disease. People with diabetes are at an increased risk of developing heart disease and twice as likely to die from heart attack or stroke. However, a recent survey suggest only about half of those living with diabetes are aware of the elevated risk.
“That’s why the ADA and the AHA, along with industry leaders, have teamed up to form the “Know Diabetes By Heart” initiative. These powerhouse organizations want to raise awareness and understanding of the link between people with type 2 diabetes and cardiovascular disease and empower people to reduce their risk for heart disease.”
And we want to help by sharing the incredible resources they have put together for health care professionals. Please enjoy the resources below:
- Know Diabetes by Heart poster
- ASCVD Risk Calculator
- Educational Podcasts
- Brochures
- Fact sheets and infographics
All can be found at KnowDiabetesByHeart
Please refer people with Type 2 diabetes to https://knowdiabetesbyheart.org/ for resources including a quiz to test their knowledge of the link between diabetes and heart disease.
Thank you for helping get the word out!
Sign up for Diabetes Blog Bytes – we post one daily Blog Byte from Monday to Friday. And of course, Tuesday is our Question of the Week. It’s Informative and FREE! Sign up below!
[yikes-mailchimp form=”1″]
Mindful Monday | “Social Jet Lag” and Risk of Heart Disease
 An abundance of research supports getting adequate sleep for adequate growth and overall health. Health risks increase when an individual is sleep deprived. Sleep deprivation increases risk for type 2 diabetes, high blood pressure, heart disease, and insulin resistance.
An abundance of research supports getting adequate sleep for adequate growth and overall health. Health risks increase when an individual is sleep deprived. Sleep deprivation increases risk for type 2 diabetes, high blood pressure, heart disease, and insulin resistance.
In addition, new research by the academic journal “Sleep,” has shown that,”Social Jet Lag” waking up at different times on the weekends vs. weekdays, may increase the risk of heart disease.
Current research by Duke University Medical Center demonstrated that individuals with what is referred to as “social jet lag” may also have an increased risk of depression and stress than subjects who woke up at the same time consistently. The connection thus far is not clear as some researchers believe that, “poor sleep interferes with the body’s metabolism which can lead to weight gain” which creates a vicious cycle of poor sleep and weight gain. Previous studies have also shown that a varied sleep schedule can lead to the development of obesity and type 2 diabetes.
The authors conclude that further research is needed to determine why individuals who get less sleep are gaining weight and increasing their risk for cardiometabolic conditions.
For more information on “social jet lag” and its effects on cardiometabolic health, visit A regular bedtime may benefit your heart and metabolism”
Sign up for Diabetes Blog Bytes – we post one daily Blog Byte from Monday to Friday. And of course, Tuesday is our Question of the Week. It’s Informative and FREE! Sign up below!
[yikes-mailchimp form=”1″]
“Full-fat dairy may actually benefit heart health”
 Full-fat dairy is typically thought of as being detrimental to health due to the high content of saturated fats. However, a new study begins to question this commonly known ideology.
Full-fat dairy is typically thought of as being detrimental to health due to the high content of saturated fats. However, a new study begins to question this commonly known ideology.
A recent study conducted by Dr. Dariush Mozaffarian from the Friedman School of Nutrition Science and Policy at Tufts University, challenges this popular opinion. The study reveals that whole-fat dairy does not seem to raise cardiovascular risk. Interestingly enough, some of the fats present may actually reduce your risk of heart attack and stroke.
Until recently, governmental organizations such as the United States Department of Agriculture (USDA) and the U.S. Department of Health & Human Services have advised people to avoid full-fat dairy in order to steer clear of “bad” cholesterol.
However, after studying the fatty acids contained in full-fat products, “none of the three fatty acids examined correlated with the risk of total mortality. In fact, high circulating levels of heptadecanoic fatty acid were associated with a lower risk of death from heart disease.” In fact, adults with higher levels of fatty acids overall, were 42% less likely to die of stroke.
As consumers we are often fed conflicting opinions about diet, which can make staying knowledgeable about all the options seem overwhelming. However, as diabetes educators, we want to stay aware of the many changes and developments made in the nutrition world and how this new information can benefit our diabetes community. The question now is, should the dietary guidelines be revised?
This research was funded by NIH, read the full article here. “Serial measures of circulating biomarkers of dairy fat and total and cause-specific mortality in older adults: the Cardiovascular Health Study”
To learn more, enjoy the summary article “Full-fat dairy may actually benefit heart health” by Medical News Today







 Coach Beverly Thomassian RN, MPH, CDCES, BC-ADM – CEO of DiabetesEd Services
Coach Beverly Thomassian RN, MPH, CDCES, BC-ADM – CEO of DiabetesEd Services Diana Isaacs, PharmD, BCPS, BCACP, CDCES, BC-ADM, FADCES, FCCPCES
Diana Isaacs, PharmD, BCPS, BCACP, CDCES, BC-ADM, FADCES, FCCPCES  In support of improving patient care, this activity has been planned and implemented by Partners for Advancing Clinical Education (Partners) and Diabetes Education Services. Partners is jointly accredited by the Accreditation Council for Continuing Medical Education (ACCME), the Accreditation Council for Pharmacy Education (ACPE), and the American Nurses Credentialing Center (ANCC), to provide continuing education for the healthcare team.
In support of improving patient care, this activity has been planned and implemented by Partners for Advancing Clinical Education (Partners) and Diabetes Education Services. Partners is jointly accredited by the Accreditation Council for Continuing Medical Education (ACCME), the Accreditation Council for Pharmacy Education (ACPE), and the American Nurses Credentialing Center (ANCC), to provide continuing education for the healthcare team.




