
Subscribe
eNewsletter

Ready to get certified?
Free CDCES Coach App
Download
Free Med Pocket Cards

eNewsletter

Free CDCES Coach App
Free Med Pocket Cards
Enjoy this poem by Coach Bev that summarizes steps to achieve diabetes certification success in 53 seconds!
Get Ready for Diabetes Certification Success
___________________
We know you’re excited to take your certification exam — and we want you to walk in feeling confident, calm, and completely prepared. 🖥️ To make sure you have the content you need, we have moved up the dates for our Level 3 and Level 4 live courses by a few months. We will complete Level 3 live course updates by April 30th and Level 4 updates will wrap up by June 20th. 📆Download Boot Camp flyers for complete date listings. |
We are always keeping you in mind! All of our accredited content is person-focused and evidence-based. Plus, we make sure you have fun and feel engaged during our programs. |
To prepare for your CDCES, we recommend enrolling in our CDCES Boot Camp, which includes:
✔ Level 1 – Fundamentals (2026) Recorded and ready for immediate viewing. Build your foundation and master the core concepts.
✔ Level 2 – ADA Standards Intensive 2026. Live throughout February and March. We break down the Standards of Care so they actually make sense — and stick.
✔ Level 3 – Final Exam Prep Mastery. Originally scheduled for June… but you told us that was too late. We heard you.
Level 3 now begins in March and runs through April 30th — giving you earlier access to focused exam mastery and test-taking strategy.
⬇️Download CDCES Boot Camp Flyer with New 2026 Dates!
This is your CDCES step-by-step path: Level 1 → Level 2 → Level 3. From fundamentals to final confidence 🏆.
To prepare for your BC-ADM, we recommend enrolling in our BC-ADM Boot Camp, which includes:
✔ Level 2 – ADA Standards Intensive 2026.
✔ Level 3 – Final Exam Prep Mastery. Begins in March and runs through April 30th.
✔ Level 4 – Final Exam Prep Mastery. Begins in April and runs through June 20th.
⬇️ Download BC-ADM Boot Camp Flyer with New 2026 Dates
This is your BC-ADM step-by-step path: Level 2 → Level 3 → Level 4. From Standards to advanced to final confidence 🏆.
You are the reason that diabetes care gets better.
We appreciate your hard work, advocacy, and the care you give every day!
💜Coach Beverly, Bryanna, Astraea, and Katarina
Get exam-ready with confidence.
Course credits through AMA PRA Category 1 Credits™, ACPE, ANCC, and CDR!
Full accreditation details are available on the registration page
Our CDCES Boot Camp Online Prep Bundle is a comprehensive, high-impact program built specifically for healthcare professionals preparing for the Certified Diabetes Care and Education Specialist (CDCES) exam who want to level up their clinical knowledge and skills.

This evidence-based study bundle is a comprehensive BC-ADM Boot Camp designed for advanced-level healthcare professionals preparing for the Board Certified in Advanced Diabetes Management (BC-ADM) exam and will also provide you with state-of-the-art information to level up your clinical practice.
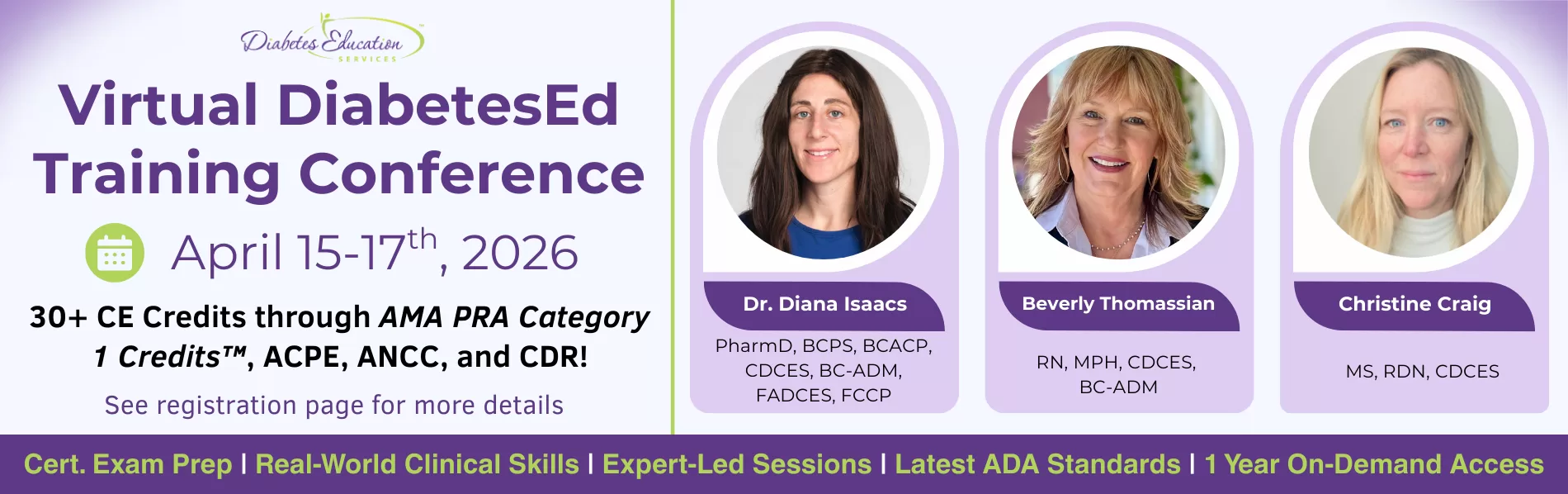
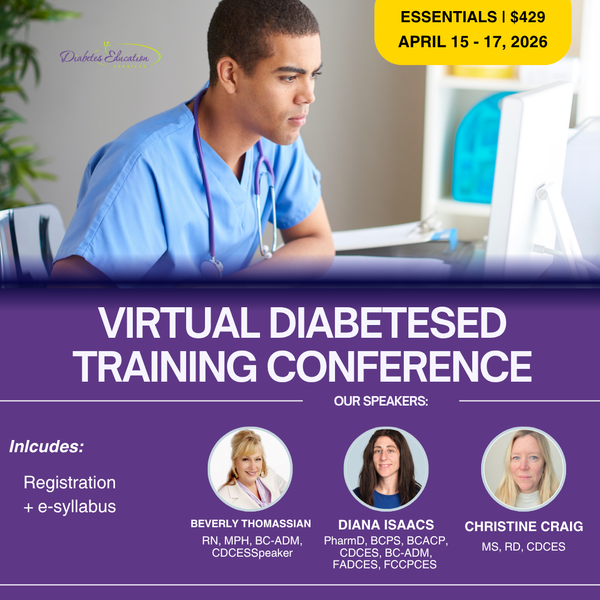
Join national experts including Dr. Diana Isaacs (Cleveland Clinic), Beverly Thomassian (30+ years of experience), and Christine Craig for high-impact, virtual learning—no travel required.
✔ Learn from National Experts — Anywhere
Get the same expert-level instruction you’d receive in person, delivered live to your home or office.
✔ Interactive & Flexible
Walk away with tools you can apply immediately in clinical practice or while preparing for CDCES or BC-ADM exams. From insulin dosing protocols to behavior change strategies that work in the real world—this content bridges theory & practice.

Announcements
___________________
Healing through Connection for Healthcare Professionals is available in:
Like me, I am sure you have experienced moments of intense frustration when you wanted to scream or give up!
Maybe you had to show up when you were emotionally spent and felt like you had nothing else to give.
I see you and I celebrate you—the hardworking healthcare professional who shows up day after day with heart and courage. In my book, Healing through Connection, I honor your journey and share strategies to help you care for your own well-being as you care for others.
Join a Virtual Conversation and Interview with Coach Bev on Feb 20th at 11:30am PST to delve into the healing power of creative endeavors.
If you can’t make the interview, enjoy this excerpt from Chapter 6, that dives into the Healing Power of Self-Expression and encourages you to dive into your creativity for healing, rejuvenation, and pure JOY.
Even if you can only commit to engaging creativity for a few minutes or half an hour a week, it makes a difference. Stop thinking about all the reasons you can’t do it, and instead, listen to that internal hum, get in the metaphorical car, turn on the ignition, and drive.
Within you lives a quiet, creative spark waiting for attention and care. When you tend to it, you renew your capacity to show up with presence, compassion, and strength, for yourself and for those in your care.
Healing through Connection is both a reminder and a roadmap; an invitation to care for yourself with the same compassion you offer others. It provides a rare perspective on mutual healing.
As we heal ourselves, we expand our capacity to help others with healing. Within the pages of this book, you’ll find a toolbox for exploring your truth, tapping into your emotions, and cultivating creativity. Together, we’ll explore the often-overlooked connection between your own lived experiences and those of the individuals in your care.
Continue reading to discover how making time for creative expression might offer you some unexpected benefits and opportunities for joy!
Did you know that Nobel Prize recipients are nearly three times more likely to engage in creative hobbies than their scientific counterparts?
Theoretical physicist Albert Einstein often played the violin when he encountered challenges in his theoretical work. He believed that music helped him think creatively and tap into his subconscious, enabling breakthroughs such as the theory of relativity.
Marie Curie, a two-time Nobel laureate for physics in 1903 and chemistry in 1911, went for frequent walks in the countryside, which allowed her to reflect and rejuvenate. These moments of tranquility likely helped her maintain focus during the grueling work of isolating radioactive elements.
It’s because they’re simply more open to having hobbies. They are more open to novel experiences and often turn to their creative endeavors when working through challenges. These seemingly unrelated scientific pursuits and personal hobbies can open doors for scientists to crosspollinate ideas across different fields, enabling them to gain fresh perspectives and uncover new insights.
Now, you may not be working toward securing the title of a Nobel laureate. Still, you might be interested in learning the secrets of expanding your mind, creating new connections, and better integrating the two sides of your brain hemispheres to provide better care or nurture your inner life.
You may be wondering how having an artistic hobby or winning a Nobel Prize in science relates to excelling as a diabetes specialist or healthcare professional. As a healthcare professional, you have likely lived through difficult experiences or witnessed profound suffering firsthand.
Plenty of science supports the idea that engaging in creative pursuits offers an outlet to express complex emotions that are not accessible through words alone.
The act of playing an instrument, taking an art class, exploring nature, or playing the bongo drums may provide a gateway to address unrequited trauma or pain, helping you to become more fully aware and present with your feelings. Did you have a childhood or adult hobby you loved doing? One that made you lose track of time as you entered the zone referred to as “flow”? Have you given yourself permission to make time for that hobby and lose yourself in that creative process?
You may want to take a ceramics or writing class, join the local choir, or start a band. Perhaps you found an old camera and want to learn more about photography or realized you’re good at painting. It can be hard to start as a beginner and potentially look silly or unskilled.
Here’s my advice: Let go of those sky-high expectations. No one expects you to paint like Monet in your first art class.
My motto is, if something makes me uncomfortable, I know I’m in the right place—because that’s where growth happens.
I encourage you to take that leap of faith and tolerate the momentary discomfort for long-term gain. It gets better, and before you know it, you will blossom in ways you never expected.
Download this worksheet to explore 20 creative endeavors that may spark inspiration within you. You may already be practicing some of these—or perhaps you have new ideas to add. Wonderful—keep going!
As a dance teacher for the past twenty years who can still balance a sword on her head, I am reminded every day that it is never too late to rediscover your joy.
Coach Beverly is honored to invite you to this special gathering and intimate conversation. During this virtual book launch, a special guest interviewer will join Coach Bev for a heartfelt conversation about why this book matters now and the real stories from clinical practice that inspired it.
Coach Bev will also share the personal journey of writing Healing through Connection and how she discovered her voice along the way. We will conclude with an interactive question-and-answer session and allow time for connection.
Come celebrate connection, healing, and the power of story as we honor the shared human experience at the heart of healthcare.
Thank you for YOUR support and commitment to promoting healing and connection every day!

Several years ago, I was nominated for Diabetes Educator of the Year. Being put forward by colleagues I deeply respected and admired was profoundly meaningful—and, honestly, a little overwhelming.
The nomination felt like recognition of decades of clinical work, teaching, mentoring, and advocacy for person-centered diabetes care. After submitting the detailed application, I allowed myself to feel hopeful. I imagined sharing my philosophy of judgment-free diabetes care with audiences across the country, offering a message of healing for both healthcare professionals and the people they serve. I even choreographed my walk-up dance in my head, ready to hit the ground running.
Then the email arrived from the board: I hadn’t been selected.
I won’t pretend it didn’t sting. I was devastated. Awards matter because they symbolize recognition; they affirm that your voice has value. When I wasn’t chosen, I found myself sitting with a familiar response that many healthcare professionals have experienced: a complicated mix of disappointment, sharp self-doubt, and the well-worn instinct to minimize the hurt and simply move on.
But once the initial ache softened, something important came into focus. I realized that while awards can amplify a message and provide a platform for it, they are not the source of the message itself. And my message was still burning—undiminished—inside me.
For years, I had been witnessing something under the surface of diabetes care and, more broadly, of healthcare. Earnest and compassionate clinicians were giving their all to provide the best care, but felt they weren’t breaking through or reaching people in ways that led to significant change. Many were questioning their worth, their effectiveness, and even their decision to enter healthcare at all.
I heard it in hallway conferences. In mentoring meetings. In calm moments after lectures when someone would come up to me and say, “I thought it was just me.”
I knew then that the story I was burning to share couldn’t be reduced to a title or an award category. The message I was holding wasn’t just about diabetes education and achieving an A1C of less than 7%. It was about the emotional gift of caring—and the healing strength of connection.
Not winning that award forced a reckoning moment: How could I share my message on a bigger stage?
The answer surprised me with its clarity. Write a book.
I wrote Healing through Connection for Healthcare Professionals because this story matters, award or no award.
The lived experiences and emotional well-being of healthcare professionals matter. You can make a bigger impact in the care you provide by taking inventory of your inner dialogue and beliefs.
Working with people living with diabetes can be filled with connection, joy, and revitalization. By leaving judgment at the door and accepting each other as we are – messy, complicated, and beautiful- you can deepen your connection. The unvoiced grief, the unresolved trauma, the silent resilience, can all have a voice at the table. As a healthcare professional, you deserve healing too.
Not winning hasn’t stopped me from sharing my message; it motivated me to find a different way to share it.
It pushed me to write honestly about:
This book is not a rebuttal to an award committee.
It’s a love letter to healthcare professionals who keep showing up even when recognition is scarce.
Today, when a nurse, pharmacist, dietitian, or physician tells me, “This book made me feel less alone,” I know I chose the right path.
I didn’t win an award, but I found my voice and shared my authentic life story in my book. This book is my commitment transparency with the hopes that it gives you permission to share your truth.
I wrote Healing through Connection so that other healthcare professionals can share their story and create a healing space for themselves and the people in their care.
Because in the end, the greatest legacy is knowing that your message touched the lives of your community and created space for more compassion, for us and those in our care.

Coach Beverly is thrilled to invite you to join this celebration of completing her book and finally getting the Audible and Kindle version up on Amazon.
We will be discussing why this book matters now more than ever. She will share real stories from her clinical practice and ask you to share yours.
Coach Bev will discuss the process involved in writing this book and how she found her voice. We will wrap up with a question-and-answer session. We hope you can join us.
Invite your friends and colleagues too!
Featured Articles & Announcements ___________________________ |
Webinars & Programs
___________________________
Greetings, healthcare colleagues!
As healthcare professionals, we’re often invited into the most tender moments of people’s lives. In these moments, you may notice your heart swell with compassion, sorrow, or deep gratitude. While this emotional labor is rarely acknowledged, I want you to know: I see it. I hear it.
We recognize the love and care you give each day. Whether it’s an after-hours check-in, helping with food access, volunteering at a community event, or offering a much-needed hug.
This February, let’s take a moment to honor you and the quiet heroism of showing up again and again with an open heart. In celebration, we are kicking off our “Spreading the Love Sale” starting today!
In this newsletter issue, I share how not being selected for a diabetes educator award led me to a deeper realization and lit a fire to share my message by writing a book.
We also highlight the power of professional connections and the importance of membership in shaping a healthcare future that reflects our values and vision. A special thanks to Sarah Hormachea, RD, MS, CDCES, BC-ADM for her meaningful insights and guest article contribution.
In celebration of fiber, don’t miss nutrition expert Christine Craig’s article featuring the unsung benefits of fiber plus a high five list.
A tech-focused feature from Dr. Beattie explores how technology and diabetes distress can be linked, along with tools to address it.
You are the heartbeat of health care! Here’s to leading with love this month and every month.
With hearts full of gratitude,
Coach Beverly, Bryanna, Astraea & Katarina
Use Code “LOVE15“ at Checkout!

Basic & e-Deluxe CDCES Boot Camp Bundle includes:
CDCES Boot Camp | 50+ CEs
Starting: $449 | Sale Price: $381.65
Use the Code “LOVE15” for 15% Off at Checkout!
Our CDCES Boot Camp Online Prep Bundle is a comprehensive, high-impact program built specifically for healthcare professionals preparing for the Certified Diabetes Care and Education Specialist (CDCES) exam.
✔ Earn CE/CPE credit through AMA PRA Category 1 Credits™, ACPE, ANCC, and CDR. For more information on accreditation, visit the registration page on our Online Store and click the “Accreditation” tab.
✔ Learn at your pace with expert-led, exam-focused content
✔ Everything you need—organized, practical, and in one place
✔ Perfect for self-directed learners who want complete, person-centered content for clinical practice and exam prep.
✔ Build knowledge, sharpen test-taking skills, and prepare with confidence—on your schedule.
Focused. Flexible. Proven.
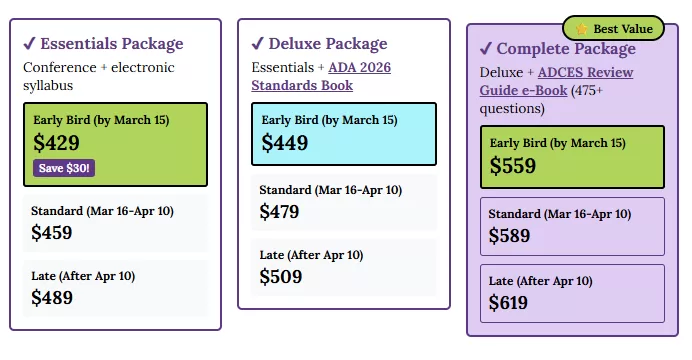
Starting: $429 | Sale Price: $364.65
Use the Code “LOVE15“ for 15% Off at Checkout!
Gain fresh insights, practical tools, and a deeper understanding of the latest in person-centered diabetes care. Our expert team brings the ADA Standards of Care to life—covering medications, behavior change, technology, and more!
If you’re renewing your CDCES or BC-ADM certification this live conference, paired with a handful of free bonus courses, serves as the ideal renewal companion!

Feb. 19th, 2026 at 11:30 AM PST
Join this FREE, pharmacist-focused webinar Co-led by Diana Isaacs, PharmD, BCPS, BC-ADM, BCACP, CDCES, FADCES, FCCP, Endocrinology Clinical Pharmacy Specialist and Coach Beverly Thomassian, RN, MPH, CDCES, BC-ADM.
Leave with a practical roadmap for achieving Certification Diabetes Care and Education Specialist (CDCES) or Board Certification in Advanced Diabetes Management (BC-ADM).
March 31st, 2026 at 11:30 AM PST
Taking the CDCES Exam in the next 6 months? Register for our Step 2, “Prep to Take the CDCES Exam” FREE Webinar today!
Coach Beverly will review examination process, sample test questions, and the reasoning behind choosing the BEST answers. Gain valuable insights on the exam content and boost your knowledge and test taking confidence. Hope to see you there.

Featured Articles __________________________ |
Today marks Martin Luther King Jr Day, which gives us pause to reflect on his ideals of equality and justice through acts of service and community care.
Our Bridge Scholarship is rooted in these ideals of service and reciprocity. Our Scholar and Mentorship program goes beyond education—it’s about building connections, fostering professional growth, and creating a vibrant community of passionate diabetes care providers.
We are proud to offer 14 “Making a Difference” Scholarship spots for healthcare professionals to attend our Virtual DiabetesEd Training Conference at no cost or a reduced registration fee. If you or a colleague is seeking to achieve diabetes certification and improve the health of your community, you may qualify for this scholarship opportunity.
Two exciting opportunities to help you on your way!
We are deeply grateful to all the mentors and healthcare professionals who are on their journey toward becoming certified diabetes specialists and leaders in diabetes care.
With heartfelt gratitude,
Coach Beverly, Bryanna, Astraea & Katarina
You are invited to join our FREE Test-Taking Success Webinar on January 23rd, 2026, designed specifically for busy healthcare professionals preparing for diabetes certification.
During this webinar, you will have the opportunity to answer and dissect 20 sample exam questions alongside Coach Bev. Learn how to avoid common exam pitfalls and get to the best answer!
This content will boost your confidence and clarity so you can walk into exam day feeling prepared, calm, and in control. Coach Beverly has helped thousands of candidates cross over the finish line to success. She has passed her CDCES exam 7 times and counting.
🎯 Gain Confidence with Proven Strategies —save your spot today.
We are geared up to help grow and mentor future Certified Diabetes Care and Education Specialists (CDCES) to meet the increasing and varied needs of our diabetes community.
We are offering 14 Bridge Scholarships, which cover the registration cost for our “Virtual DiabetesEd Conference” on April 15-17, 2026. This program will provide you with diabetes fundamentals and beyond! Earn 30+ CEs with access to the courses for one year!
Over the next 10 years we are “Building a Bridge” to welcome a thousand new diabetes educators into the field. If you know a healthcare professional seeking a new challenge and eager to pursue a meaningful and rewarding specialty, please invite them to consider becoming a Certified Diabetes Care and Education Specialist (CDCES).
Get exam-ready with confidence. Our CDCES Boot Camp Online Prep Bundle is a comprehensive, high-impact program built specifically for healthcare professionals preparing for the Certified Diabetes Care and Education Specialist (CDCES) exam. ✔ Earn CE/CPE credit through AMA PRA Category 1 Credits™, ACPE, ANCC, and CDR. For more information on accreditation, visit the registration page on our Online Store and click the “Accreditation” tab. ✔ Learn at your pace with expert-led, exam-focused content ✔ Everything you need—organized, practical, and in one place Perfect for self-directed learners who want complete, person-centered content for clinical practice and exam prep. Focused. Flexible. Proven. Build knowledge, sharpen test-taking skills, and prepare with confidence—on your schedule. |
Get ready for Exam Success Starting Today! Sale ends January 26, 2026! |
CDCES Boot Camp Bundle includes:
Levels 1, 2, and 3 of our Online University
30+ expert-led courses
50 CE/CPEUs
400+ online practice questions
Handouts, podcast, video and one year access—all in one streamlined platform.
Take 15% OFF with coupon code Community15.
Sale ends January 26, 2026!
We are geared up to help grow and mentor future Certified Diabetes Care and Education Specialists (CDCES) to meet the increasing and varied needs of our diabetes community.
We are offering 14 Bridge Scholarships, which cover the registration cost for our “Virtual DiabetesEd Conference” on April 15-17, 2026. This program will provide you with diabetes fundamentals and beyond! Earn 30+ CEs with access to the courses for one year!
Over the next 10 years we are “Building a Bridge” to welcome a thousand new diabetes educators into the field. If you know a healthcare professional seeking a new challenge and eager to pursue a meaningful and rewarding specialty, please invite them to consider becoming a Certified Diabetes Care and Education Specialist (CDCES).
Diabetes Education Services is committed to improving equity and access to diabetes training and education for a diverse group of healthcare professionals. We don’t want financial barriers to stop anyone from attending this conference. In appreciation of those who are role models and advocates for practicing the best diabetes care in their communities.
The Bridge Scholarship program is not just about learning—it’s about creating connections, fostering growth and building a community of passionate diabetes care professionals. We are excited to offer this incredible opportunity to those who are committed to advancing their skills and knowledge in diabetes education. Together, we can make a real difference in the lives of those living with diabetes.
These scholarships are awarded to healthcare professionals who provide care and education to under-served communities that lack access to Diabetes Specialists and healthcare resources. Applicants must be in the process of gaining practice hours and planning to take their CDCES Exam within the next 3 years.
Gain fresh insights, practical tools, and a deeper understanding of the latest in person-centered diabetes care. Our expert team brings the ADA Standards of Care to life—covering medications, behavior change, technology, and more!
If you’re preparing for the CDCES or BC-ADM exam, this conference, paired with a handful of free bonus courses, serves as the ideal study companion! Plus, this content counts toward the ADA Standards requirements for CDCES Renewal.
Featured Articles ___________________________ |
Greetings, wonderful healthcare colleagues!
You are going to love all the updates to our cheat sheets, online university courses, and PocketCards.
Coach Beverly has been excitedly scanning the 2026 ADA Standards to discover updates and advances in diabetes care. She and her team are hustling to integrate these new findings across our platforms, including the CDCES Coach App, handouts, courses, and web content, so that you can access the latest information with confidence.
In our first newsletter of 2026, we are excited to share that we have made significant changes to our Medication PocketCards in the GLP-1/GIP RA section. Now included are the diabetes and weight-loss versions of this popular medication class, with indications for each. You can compare and contrast at a glance. Download your free version and read more below.
Our library of Cheat Sheets is updated and includes a few new additions! These sheets are available on our website and the CDCES Coach App for easy access, with the option to download and share with your colleagues and people living with diabetes alike.
Christine Craig, MS, RD, CDCES, explores her experience with a client who arrived at her office distraught and struggling with the loss of his lifelong partner. Pass the tissues.
Our Tech contributor, Dr. Beattie, provides a summary of red flag statements that may indicate a person is experiencing barriers to effectively using technology in their day-to-day management.
We encourage you to test your knowledge with our Question and Rationale of the Week. January kicks off our Level 1 Fundamental Series, followed by our annual ADA Standards of Care update on January 29th and Level 2 Mastery Course Series in February. We hope to see you there!
Here is to a 2026 filled with self-compassion and moments of awe.
Coach Beverly, Bryanna, Astraea & Katarina
If you’ve considered not renewing your professional practice group membership this year, you’re not alone. Membership in professional organizations has declined as many turn to social media and AI-driven platforms for information and connection. Still, I encourage you not to abandon professional membership in favor of options that may seem cheaper or more convenient.
In a noisy, chaotic landscape of information overload, professional practice groups remain a refuge from the storm. They offer a trusted alternative to clickbait, providing vetted expertise, meaningful connection, and true professional community.
No amount of viral TikTok videos or LinkedIn commentary can replace the depth of connection and sense of purpose that come from active engagement in a professional practice organization. And, here’s why.
Professional practice groups, also known as professional practice organizations, are designed to advance a specific field by providing members with networking opportunities, professional development, and practice resources. In healthcare, these organizations may be tailored to the needs of a single discipline, such as the American Nurses Association, or span interdisciplinary areas of practice, like the Association of Diabetes Care and Education Specialists or the American Diabetes Association.
Some organizations focus primarily on education and credentialing, while others emphasize leadership development and community building. Still others center their work on advocacy related to patient care, access, and insurance coverage.
At its core, most professional practice groups are founded and driven by their members, with membership dues supporting the administrative needs required to operate. As groups grow, they often engage professional management or organizational leadership teams to oversee day-to-day operations such as membership services, programming, finances, legal compliance, and other administrative functions.
Strategic direction and oversight typically remain the responsibility of an elected or appointed governing body. In some cases, professional organizations may choose to hire members, transitioning them from volunteer roles into paid staff positions.
As operating costs rise, often without corresponding increases in salaries or reimbursement, many professional practice groups partner with industry or government organizations for additional financial support. These partnerships can help keep membership dues, educational programming, and events accessible and affordable for members.
It would be easy to blame declining professional membership on COVID, but the reality is this trend started long before the pandemic. Across healthcare, fewer clinicians are joining or renewing professional organizations. Cost is often the biggest factor. When budgets are tight, many people feel forced to choose one membership instead of several. Others question whether the return on investment is still there, especially when education, networking, and professional content are now easy to find online for free.
In my own field of dietetics, I also hear concerns about transparency and alignment with the future of the profession. The move to a master’s degree requirement without a meaningful increase in entry-level pay has created real frustration, particularly for early-career professionals and those from underrepresented backgrounds. Many feel their needs were not fully considered or advocated for during that transition.
These frustrations are valid. But they are also exactly why walking away may not be the answer. Professional practice groups are shaped by the people who show up. If something isn’t working, the most effective way to change it is to get involved.
Despite the challenges, the benefits of professional membership far outweigh the drawbacks, and the opportunity to influence the future of your profession is worth staying engaged.
Social media platforms like LinkedIn, Substack, and X (formerly Twitter) are great for ideas and inspiration, but they rarely offer sustained, reciprocal mentorship. Most interactions are brief, one-sided, or tied to someone selling something.
Professional practice groups offer something different. They foster trusted relationships with people who have walked the same path and understand the realities of the work. Advice is shared openly, support develops over time, and there is no sales funnel attached. It is not a transaction. It is a co-op.
Professional practice groups offer a space to ask questions without worrying about who is watching or how you are being perceived. There is room to be unsure, curious, or quietly ambitious, especially early in your career or during periods of transition.
Unlike social media, which often rewards confidence and visibility, professional groups tend to reward competence, growth, and thoughtful engagement. The focus is less on performance and more on learning and supporting one another as professionals.
Most online content is designed for reach, not rigor. Professional practice groups focus on depth, offering evidence-based, peer-reviewed insights shared by professionals, for professionals. It is not about trends. It is about trust. As these professional practice groups evolve, many are also opening the door to honest conversations about topics once considered off-limits, such as workplace culture, compensation, and career options.
I’ve made meaningful connections on social media and learn something new every day from tools like ChatGPT. Those platforms have their place.
But when I want to understand where a profession is really headed, I look to professional practice groups. Who is presenting the research? What study resources are being recommended? Who is mentoring, volunteering, and helping shape the future of the field? These groups create space to contribute, learn, and grow alongside peers who care deeply about the work.
I’ve always respected my work colleagues, but I truly value my professional practice peers. I hope you will, too.
References:
Sarah is the owner of Sarah Hormachea: Diabetes Care and Education, LLC. She is a long-time member of the Academy of Nutrition and Dietetics, the Association of Diabetes Care and Education Specialists (ADCES), and the American Diabetes Association (ADA). She currently serves as Webinar Chair for the Academy’s Diabetes Practice Group and is an incoming member of the ADCES Board of Directors. She is also enrolled in a women’s leadership development program through the ADA.