
Subscribe
eNewsletter

Ready to get certified?
Free CDCES Coach App
Download
Free Med Pocket Cards

eNewsletter

Free CDCES Coach App
Free Med Pocket Cards

The holiday season can be stressful and throw us off our normal routine. This can compromise sleep and disrupt usual eating habits. In addition, it can trigger feelings of distress and self-doubt for people with diabetes if blood sugars go outside of goal range.
To help everyone feel their best during this holiday season, we have created a handout that highlights ten strategies to survive the holiday commotion. And even if all ten aren’t possible, just pick one or a few to try out. In addition, we have compiled a list of strategies to help reframe and reset when individuals are experiencing feelings of diabetes distress.
These Cheat Sheets have lots of helpful tips that you can print and share with your friends, participants, and colleagues!

1. Be a sleep warrior – People living in the United States are chronically underslept. Not getting enough sleep is associated with increased hunger, higher blood sugars, poor concentration, frequent illness, and impaired problem-solving. Make sure to give yourself the gift of at least 7 hours of sleep a night. This sleep will help you make the best choices for your health and will protect against illness and fatigue. You got this.
Goal: Get at least 7 hours of sleep a night. You deserve it.

2. Keep active – Holidays can put our exercise plans to the test, but we have a few ideas for you. Take an after-meal stroll instead of plopping on the couch. After meal walks lower post-meal blood sugars and increases energy by getting muscles activated. Just 10 minutes of walking after meals can make a big difference. You can even put music on and have a small dance session, anything to get your body moving.
Goal: Work toward 30 minutes of activity a day.
3. Don’t forget the Fiber – With all the snacks and tempting foods, whole healthy foods may take a back seat. Enjoy the abundance of seasonal vegetables, fruits, nuts, and grains that are fiber-rich and that decrease inflammation. Examples include; yams, squash, mandarin oranges, almonds, pistachios, quinoa, kale, brown rice, warm oatmeal, salads, and broth-based soups.
Goal: Strive to eat at least 25gms of fiber a day.

4. Enjoy the ultimate beverage – H20. Water is the perfect way to keep hydrated, replenished, and keeps appetite in check. Add a splash of flavor with a jigger of fruit juice or fresh cucumbers, lime slices, or a sprig of rosemary. Be creative. Sparkling waters come in a vast variety of flavors, are calorie-free, and contain no artificial sweeteners.
Goal: Keep hydrated by enjoying plenty of water.

5. Keep an eye on alcohol – While it’s true that red wine offers a beneficial anti-inflammatory compound called resveratrol, drinking too much alcohol can lead to unintended outcomes. Studies show that we make poorer food choices if alcohol is on board. This can offer special challenges in party settings, where temptations are abundant. A drink of alcohol contains about 100 calories and mixed drinks have even more. In addition, alcohol can lead to low blood sugars, especially for those taking insulin or sulfonylureas.
Goal: Limit alcohol to one drink a day for women, two drinks a day for men.
6. You are already sweet enough – Holidays and sugar go hand in hand. If possible, try and eat less than 6 teaspoons of added sugar (does not include natural sugars found in fruit and milk). This goal may not be realistic on all days, but aim for success most of the time. Excess sugar intake can cause inflammation and buildup of fat in the liver. One strategy is to limit sugar intake during the day and save your 6 teaspoons for that special dessert or parties. When looking at labels, it is helpful to know that 1 teaspoon equals 4 gms of sugar.
Goal: Limit sugar to 6 teaspoons a day.

7. Your teeth need extra special attention – Taking care of our teeth and gums improves health. Gum inflammation is associated with blood vessel inflammation. Swollen gums can also lead to an increase in blood sugars. During the holidays, find time for regular oral hygiene. Your mouth (and dental team) will thank you.
Goal: Brush teeth at twice daily and floss at least once daily.
8. Keep connected to friends and family who love you just the way you are! – As enjoyable as holidays can be, reuniting with family can also cause stress and stir-up emotions. Feeling out of sorts can lead to stress eating and decrease self-care. If possible, reach out to a trusted friend to share your feelings or keep a holiday journal. Consider bringing a favorite book along during your travels that you find inspiring and comforting. Give yourself permission to steal away for some quiet time.
Goal: Self-care is important during the holidays.
9. Enjoy an Oxygen Cocktail – Studies show that when humans venture into natural outdoor settings, heart rate and blood pressure improve. Take a moment to appreciate the feeling of the air on your skin, take a deep breath of fresh air, try to find nests in leafless trees, listen to the animal sounds and bird songs and just enjoy that moment.
Goal: Step into nature daily.

10. Take inventory of things that you are grateful for – Find a moment each day to reflect on a few things that brought you joy or good feelings. Maybe it was your cousin who lent you her favorite sweater. Or an Aunt who gave you the best hug. Special moments with a best friend or an after-dinner walk enjoying the fall leaves. These small moments of connection and beauty are one of the most treasured gifts of the holiday season that linger in our hearts and memory long after we say our goodbyes.
Goal: Take note of special moments.
Click here to download 10 Steps to Survive the Holidays PDF – a great handout that includes the info above to print and share with your friends, patients, and colleagues!
Sign up for Diabetes Blog Bytes – we post one daily Blog Byte from Monday to Friday. And of course, Tuesday is our Question of the Week. It’s Informative and FREE! Sign up below!
[yikes-mailchimp form=”1″]The use of DES products does not guarantee the successful passage of the CDCES exam. CBDCE does not endorse any preparatory or review materials for the CDCES exam, except for those published by CBDCE.”**To satisfy the requirement for renewal of certification by continuing education for the Certification Board for Diabetes Care & Education (CBDCE), continuing education activities must be applicable to diabetes and approved by a provider on the CBDCE List of Recognized Providers (www.ncbde.org). CBDCE does not approve of continuing education. Diabetes Education Services is accredited/approved by the Commission of Dietetic Registration which is on the list of CBDCE Recognized Providers.”

In celebration of National Diabetes Month, DiabetesEd Services is hosting a T-shirt and Book Give Away! We’d love to hear what you’ll be doing to observe this important month—share your plans with us, and we may feature your response! Submissions due by Nov 29th!! Thank you and we appreciate your participation. Be sure to take a moment to explore our website for resources designed to support Diabetes Educators!
For last week’s practice question, we quizzed participants on a person’s concerns about metformin use & potential side effects. 41% of respondents chose the best answer. We want to clarify and share this important information, so you can pass it on to people living with diabetes and your colleagues, plus prepare for exam success!
Before we start though, if you don’t want any spoilers and haven’t tried the question yet, you can answer it below: Answer Question

Question: LS is reluctant to start on metformin because they heard it can cause diarrhea and kidney problems. You reassure LS that metformin doesn’t harm the kidneys and can actually improve gut health.
Based on the most recent evidence, which of the following is true?
Answer Choices:
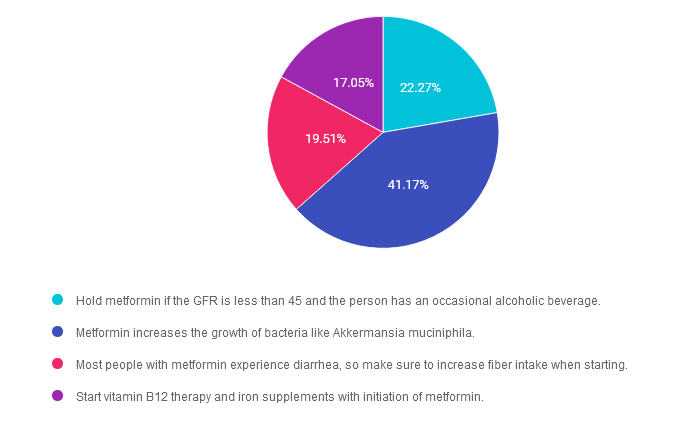
Answer 1 is incorrect. 22.27% chose this answer. “Hold metformin if the GFR is less than 45 and the person has an occasional alcoholic beverage.” The guidelines state not to start metformin is the GFR is less than 45. But if someone is already on metformin their GFR drops below 45 we can continue it with caution and we might reduce the dose. We stop metformin if the GFR is less than 30. We don’t recommend metformin if someone is binge drinking due to the potential risk of lactic acidosis. An “occasional drink” would not reach the threshold to stop the metformin. Download Med PocketCards for more info.
Answer 2 is correct. 41.17% of you chose this answer. “Metformin increases the growth of bacteria like Akkermansia muciniphila.” Yes, this is the best answer. Metformin has been shown to increase gut bacterial diversity with a special nod to one of our favorite mucus protective bacteria known as “Akk”. This beneficial bacteria increase levels of butyrate and protects intestinal mucous lining, which helps to decrease inflammation. Cheers for AKK! Download Med PocketCards for more info.
Answer 3 is incorrect. About 19.51% of respondents chose this. “Most people with metformin experience diarrhea, so make sure to increase fiber intake when starting.” This is not accurate, since only a small percentage of people experience diarrhea. And, if they do, switching them to metformin extended release can decrease intestinal discomfort. Download Med PocketCards for more info.
Finally, Answer 4 is incorrect. 17.05% chose this answer. “Start vitamin B12 therapy and iron supplements with initiation of metformin.” Some, but not all individuals experience B12 deficiency on long term metformin therapy. We would only start B12 replacement therapy after confirming low B12 levels. Download Med PocketCards for more info.
We hope you appreciate this week’s rationale! Thank you so much for taking the time to answer our Question of the Week and participate in this fun learning activity!
All hours earned count toward your CDCES Accreditation Information
The use of DES products does not guarantee the successful passage of the certification exam. CBDCE and ADCES do not endorse any preparatory or review materials for the CDCES or BC-ADM exams, except for those published by CBDCE & ADCES.
by Christine Craig, MS, RD, CDCES
Recent research highlights the role of diet in preventing and slowing the progression of diabetes retinopathy, which is the leading cause of vision impairment among individuals with diabetes.
While glucose management is essential in reducing the risk of retinopathy, nutritional strategies that target reduced glycemic variability, blood pressure, inflammation, and oxidative stress significantly impact retinal health and vision.
In 2021, it was estimated that 26.43% of individuals with diabetes in the US have diabetic retinopathy, and 5.06% of individuals have vision-threatening diabetic retinopathy.1

Non-Proliferative and Proliferative Retinopathy
Clinically, diabetic retinopathy presents as non-proliferative diabetic retinopathy (NPDR) and proliferative diabetic retinopathy (PDR).
Chronic hyperglycemia, dyslipidemia, nephropathy, and hypertension are factors that increase the risk of diabetic retinopathy.3 In type 1 diabetes, the DCCT and EDIC studies identified that higher mean HgbA1c is the strongest predictor of retinopathy progression. A 1% reduction in HgbA1c was associated with a 35% reduction in the risk of developing diabetic retinopathy.
Screening is essential; 2019 data indicates that 64.8% of individuals with diabetes had completed an eye exam in the past 12 months.2
The ADA Standards of Care recommends that adults with type 1 diabetes be screened within five years of diagnosis and individuals with type 2 diabetes be screened at the time of diagnosis. followed by an annual screening. If the eyes are healthy on exam and glucose is within the target range, eye specialists can consider extending screening to every 2 years.3
Diet and Retinopathy Risk
An individual’s diet plays in important role in retinal health.
Research has associated the consumption of fatty fish, fruits, vegetables, and antioxidant-rich foods with a reduced risk of diabetic retinopathy.4
In contrast, dietary patterns that contribute to glucose elevation and increase advanced glycation end-products (AGEs) contribute to retinal inflammation and microvascular damage.4 Focus on dietary interventions that support glycemic, lipid and blood pressure management help reduce risks or slow profession of this condition.3
Just as in general diabetes management, no one diet pattern is recommended; however, there is some evidence for specific nutrients. Research on nutrients such as omega-3 fatty acids, fiber, lutein and zeaxanthin, Vitamin C, Vitamin E, and Zinc have shown positive association with lowering diabetic retinopathy risk.4 To meet these nutrient needs, whole food-based diets rich in vegetables, whole grains, legumes, lean proteins, and healthy fats may be considered.
The Dietary Inflammatory Index (DII)
The Dietary Inflammatory Index (DII) is a scoring system that measures the inflammatory potential of individual diets based on 45 parameters, including various macronutrients, micronutrients, and phytochemicals. Liu and colleagues5 found that a one-point increase in the DII score was associated with 38% increased odds of having diabetic retinopathy. Their research also noted the relationship between higher HbgA1c, duration of diabetes, and increased retinopathy risk. While the research used NHANES data, the small sample size and retrospective cross-sectional analysis limit the ability to conclude causation.
We can consider the benefits of increasing anti-inflammatory foods and decreasing inflammatory foods, but additional information is needed to implement direct recommendations.
Role of Diabetes Educators in Prevention
As Diabetes Care and Education Specialists (DCES), we can support the prevention of diabetic retinopathy by helping individuals manage glucose through dietary patterns to reduce risk and slow progression. Although barriers exist to adopting anti-inflammatory diets rich in whole foods, antioxidants, and essential nutrients, understanding the potential connection beyond glycemic management can guide additional nutrition interventions.
Programs that support retinal photography with remote reading can increase access to screening in areas lacking accessible services. Additionally, ensuring blood pressure, lipid and renal screening and management, understanding the role of physical activity, and long-term glucose management can support vision health. DCES can empower patients to make sustainable lifestyle changes that support retinal health through individualized counseling and interdisciplinary collaboration with eye care providers.
References:


JR is excited about enjoying Thanksgiving with family but is a little worried about post-Thanksgiving meal blood sugar elevations. JR takes 1 unit bolus insulin for every 10 gms of carb, with a correction factor of 1 unit for every 50 points above 120, plus 23 units of basal insulin at night. For Thanksgiving JR plans to eat:
If JR’s blood Sugar is 173 before the meal, what is the best approach?


Register above or simply visit DiabetesEd.net and browse the Free Resources Tab. While most webinars are available to attend at no cost, you have the option to purchase the session if you wish to earn Continuing Education (CE) credits.
All hours earned count toward your CDCES Accreditation Information
The use of DES products does not guarantee the successful passage of the certification exam. CBDCE and ADCES do not endorse any preparatory or review materials for the CDCES or BC-ADM exams, except for those published by CBDCE & ADCES.

November is Diabetes Awareness Month, and there’s no better way to expand your knowledge than by attending one of the many free webinars hosted by Diabetes Education Services. These webinars provide essential insights that can help you stay informed and empowered in your journey to becoming a Diabetes Educator.
This month, join Coach Beverly—a trusted expert in diabetes education—as she leads a series of engaging and informative webinars. With her wealth of experience and passion for helping others, Coach Beverly will guide you through topics ranging from the basics of diabetes to more advanced management strategies. Don’t miss these valuable opportunities to learn from one of the top educators in the field. Be sure to register for the upcoming sessions and make the most of Diabetes Awareness Month!

To celebrate 25 years as the CEO of Diabetes Education Services and 30 years of specializing in diabetes, I am excited to offer my ADCES presentation, Strategies to Revitalize your Diabetes Program or Business.
If you are starting a diabetes self-management program or want to revitalize your current practice, we invite you to join this one-hour webinar full of practical tips on advocating for the best health care in a variety of practice settings.
Register for our FREE Preparing for BC-ADM Exam Webinar!
Interested in learning more about Board Certification in Advanced Diabetes Management?
This webinar will answer your questions.
Register above or simply visit DiabetesEd.net and browse the Free Resources Tab. While most webinars are available to attend at no cost, you have the option to purchase the session if you wish to earn Continuing Education (CE) credits.
For more information or any questions, please email [email protected].
Accreditation: Diabetes Education Services is an approved provider by the California Board of Registered Nursing, Provider 12640, and our Level 4 | The Impact of Adverse Childhood Experiences on Health awards 1.0 CPEUs in accordance with the Commission on Dietetic Registration’s CPEU Prior Approval Program.
The use of DES products does not guarantee the successful passage of the certification exam. CBDCE and ADCES do not endorse any preparatory or review materials for the CDCES or BC-ADM exams, except for those published by CBDCE & ADCES.
How You Can Participate:
Share your plans and activities for National Diabetes Month by Submitting the activities form by November 29th. Tell us what you’re doing to spread awareness, provide education, or advocate for diabetes prevention and management. Your ideas have the power to motivate others to take action, and we’d love to amplify your voice by sharing your initiatives on our social media channels or website.

As we celebrate National Diabetes Month, we have the opportunity to inspire change, build stronger communities, and help individuals affected by diabetes lead healthier lives. Whether you’re just starting your diabetes education journey or have been in the field for years, your contributions are vital to improving diabetes care. By sharing your plans and participating in our giveaway, you’re helping to spread the word and create a more informed, supportive environment for everyone impacted by diabetes.
We can’t wait to hear from you and see how you’re making a difference this National Diabetes Month. Together, we can create a lasting impact!
Submit your Diabetes Ed Awareness activity by Nov 29th and enter to win—we look forward to celebrating your efforts with you! 💙
The use of DES products does not guarantee the successful passage of the certification exam. CBDCE and ADCES do not endorse any preparatory or review materials for the CDCES or BC-ADM exams, except for those published by CBDCE & ADCES.
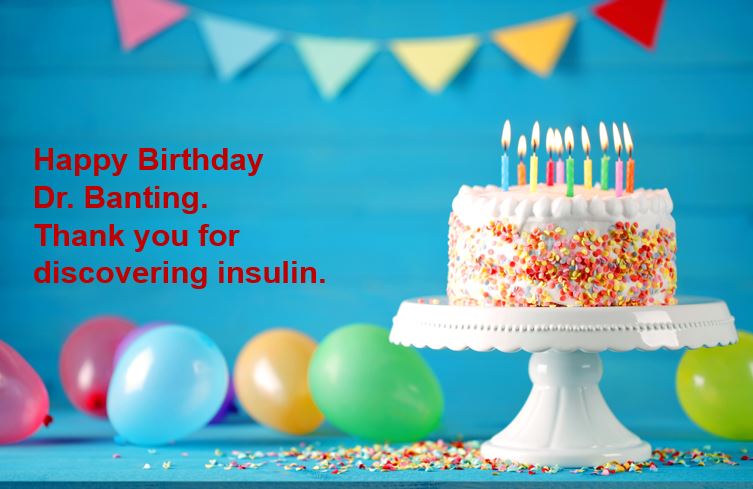
Over one hundred years ago, two researchers kick-started the production of insulin, making it available for worldwide use and saving millions of lives. Now, that’s a real cause for celebration. The discovery of insulin by Banting, Best, and team was no easy feat. They encountered resistance, setbacks, and failures.
Dr. Banting secured space to test out his theory at the University of Toronto during a hot summer in 1921.

Along with his colleague, Charles Best, and a bare-bones lab, they conducted dozens of experiments on dogs. Marjorie (dog 408) lived for 70 days without a pancreas due to receiving life-saving insulin injections.
This success was replicated in other experimental dogs and ultimately provided the first step toward producing insulin from pig and cow pancreases.
In 1922, children with type 1 diabetes started receiving early doses of this newly available life-saving hormone. Leonard Thompson, was the first recipient in January 1922, followed by many thereafter. Here is a heartbreaking then uplifting photo of J.L., who after 2 months of receiving insulin, transformed into a healthy young boy.
Sign up for Diabetes Blog Bytes – we post one daily Blog Byte from Monday to Friday. And of course, Tuesday is our Question of the Week. It’s Informative and FREE! Sign up below!
[yikes-mailchimp form=”1″]
Accreditation: Diabetes Education Services is an approved provider by the California Board of Registered Nursing, Provider 12640, and Commission on Dietetic Registration (CDR), Provider DI002. Since these programs are approved by the CDR it satisfies the CE requirements for the CDCES regardless of your profession.*
The use of DES products does not guarantee the successful passage of the CDCES exam. CBDCE does not endorse any preparatory or review materials for the CDCES exam, except for those published by CBDCE.
For last week’s practice question, we quizzed participants on concerns with diabetes risk and statin use. 95% of respondents chose the best answer. We want to clarify and share this important information, so you can pass it on to people living with diabetes and your colleagues, plus prepare for exam success!
Before we start though, if you don’t want any spoilers and haven’t tried the question yet, you can answer it below: Answer Question

Question: LC is a 49-year-old living with type 2 diabetes and reports during their appointment they have stopped their statin because of concern over risk of type 2 diabetes incidence with statin use.
Using the ADA Standards of Care as a guide, what would be the best response to LC concerns?
Answer Choices:
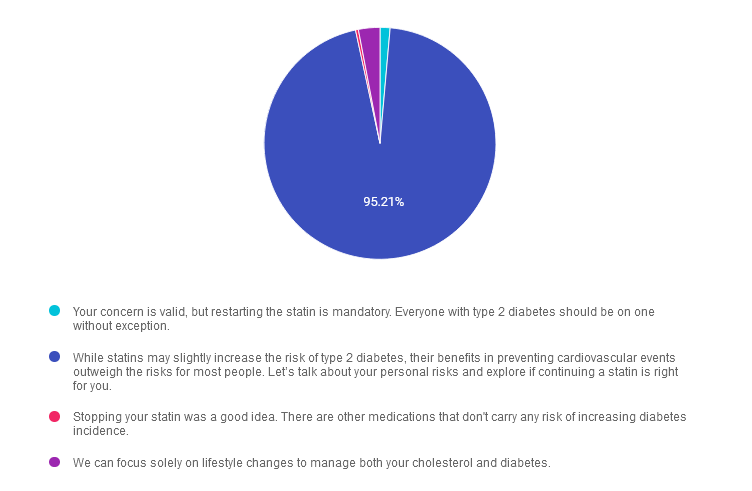
Answer 1 is incorrect. 1.40% chose this answer. “Your concern is valid, but restarting the statin is mandatory. Everyone with type 2 diabetes should be on one without exception.” Although statins are recommended for most people with diabetes, especially those over 40, the ADA emphasizes individualized care. There may be specific cases where statin use is not appropriate. Mandatory recommendations fail to consider individual preferences and circumstances, which are central to person-centered care.
Answer 2 is correct. 95.21% of you chose this answer. GREAT JOB! “While statins may slightly increase the risk of type 2 diabetes, their benefits in preventing cardiovascular events outweigh the risks for most people. Let’s talk about your personal risks and explore if continuing a statin is right for you.” This response acknowledges LC’s concern while addressing the evidence-based benefits of statin therapy for cardiovascular disease prevention. Statins are generally recommended for people with diabetes because cardiovascular protection outweighs the slight increase in diabetes incidence. This option promotes person-centered care by encouraging a collaborative approach.
Answer 3 is incorrect. About 0.40% of respondents chose this. Stopping your statin was a good idea. “There are other medications that don’t carry any risk of increasing diabetes incidence.” This response is misleading and may not be the best recommendation for LC. The ADA recommends considering the individual’s cardiovascular risk profile, not discontinuing statins simply because of concerns about diabetes incidence.
Finally, Answer 4 is incorrect. 2.99% chose this answer. “We can focus solely on lifestyle changes to manage both your cholesterol and diabetes.” Discontinuing statins without clinical justification could increase LC’s risk of cardiovascular events. The ADA recommends a combination of lifestyle changes and pharmacotherapy, when appropriate, for optimal outcomes.
We hope you appreciate this week’s rationale! Thank you so much for taking the time to answer our Question of the Week and participate in this fun learning activity!


Register above or simply visit DiabetesEd.net and browse the Free Resources Tab. While most webinars are available to attend at no cost, you have the option to purchase the session if you wish to earn Continuing Education (CE) credits.
For more information or any questions, please email [email protected].
The use of DES products does not guarantee the successful passage of the certification exam. CBDCE and ADCES do not endorse any preparatory or review materials for the CDCES or BC-ADM exams, except for those published by CBDCE & ADCES.

According to the latest CDC Data, over 16% of Americans are living with diabetes and 38% have prediabetes. This means about half of our communities are living with hyperglycemia.
Advocacy and education play essential roles in diabetes care and prevention. By equipping individuals with knowledge about diabetes management, healthy lifestyle choices, and preventative measures, we empower them to take ownership of their health and inspire change within their communities.
Community-centered education can be incredibly powerful—when people feel informed and supported, they’re more likely to make meaningful changes and encourage others to do the same. This creates a ripple effect, fostering healthier communities and potentially reducing the prevalence of diabetes over time.
We have put together a list of FREE Webinars and diabetes resources in English and Spanish to share with people living with prediabetes and diabetes. Thank you for your advocacy and belief that we can make a difference.
ADA’s Diabetes Food Hub – English and Spanish! Web site filled with information on healthy eating and an abundance of delicious recipes.
ADA Resources in Spanish – this newly opened information hub is perfect for those who prefer to learn and read in Spanish.
ADA’s FREE Life with Diabetes Program: ADA’s program includes six digital, printable journeys to teach how to live well with diabetes; a monthly e-newsletter with tips, stories, and more resources; six free issues of the Diabetes Forecast® magazine; access to an online community and local events. (The program is available in both English and Spanish).
ADA’s Risk Quiz: 60-second online risk assessment for type 2 diabetes. ADA created a self-assessment and a version to fill out the assessment for others. There’s also a printable version in English & Spanish that can be distributed to help ascertain risk. This is a great first step in helping individuals consider coming in for an appointment
CDC Diabetes Prevention Program Curricula and Handouts This site offers excellent resources for those interested in offering Diabetes Prevention Education in English and Spanish.
National Diabetes Education Program is an online library of resources compiled by the NDEP to help provide accurate information and support for people living with prediabetes and diabetes.
Spanish Language Resources: language can be a barrier to adequate and quality care. ADCES has created a number of free downloads for people with diabetes and prediabetes, which have been translated into Spanish.
Type 1 Diabetes Resource Page – Includes is a list of helpful online resources for Type 1 Diabetes. It include sites for national organizations like the American Diabetes Association (ADA), sites for diabetes interest groups, and other participant organizations that provide helpful diabetes tips and opportunities to join online groups.
DiabetesWisePro for Clinicians A non-biased web site for health care professionals that has a quick tool to access insurance coverage information, how to order devices, what to include and where to go for support.
DiabetesWise A non-biased website that helps people with diabetes learn about different diabetes devices and determine the best match for their needs
Insulin Cost Savings Toolkit Resource Page – An ADCES complete listing of low cost insulin options and resources.
Technology Cost Savings Resource Page – An ADCES listing of websites and information to obtain pumps and sensors for a lower cost.