
Subscribe
eNewsletter

Ready to get certified?
Free CDCES Coach App
Download
Free Med Pocket Cards

eNewsletter

Free CDCES Coach App
Free Med Pocket Cards

TC is a 15-year-old who was diagnosed with type 1 diabetes just over a year ago. Following their diagnosis, they quickly transitioned to sensor-augmented pump therapy and are not currently taking any other medications. Recent lab results show that lipid and renal profiles are on target, A1C of 7.5%, and a fasting glucose level of 148 mg/dL. Despite following a nutrient-rich diet, TC reports experiencing fatigue, difficulty gaining weight, frequent nausea, and diarrhea.
What Standard of Care recommendation may help explain TC’s reported symptoms?

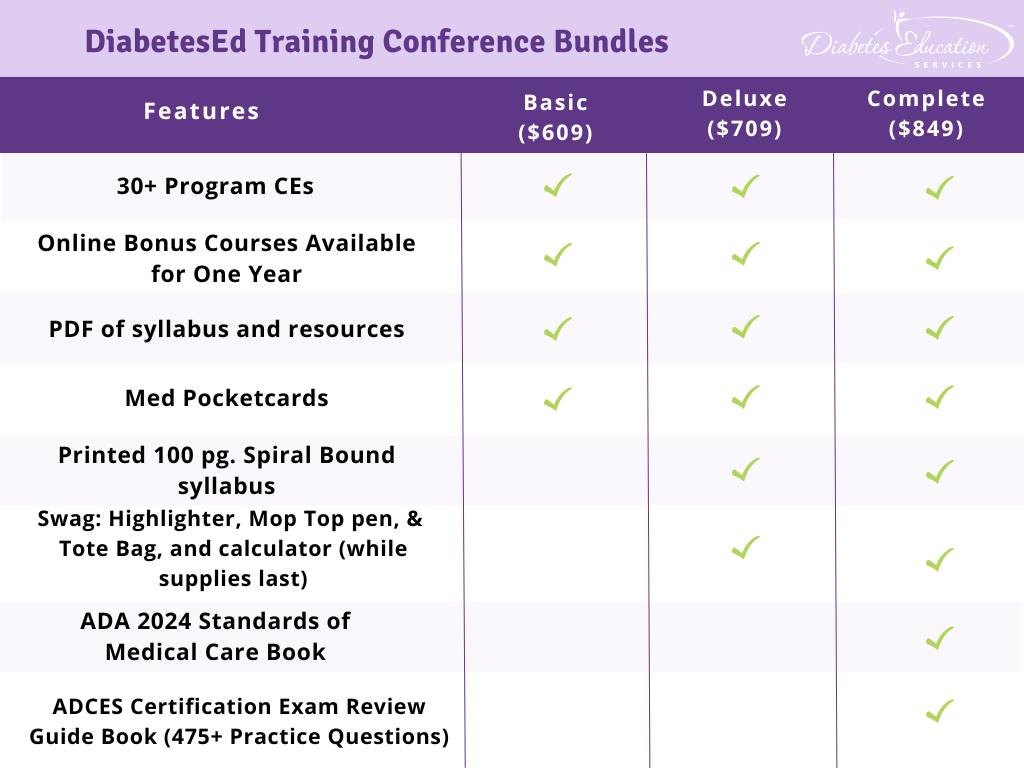
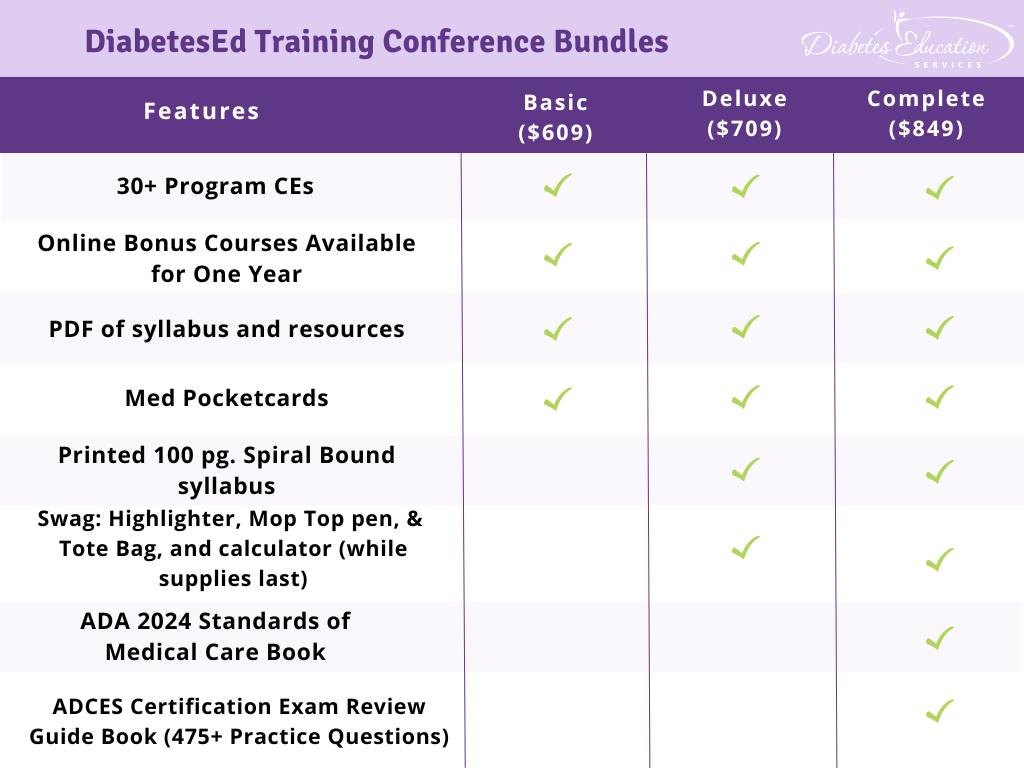
Join Coach Beverly and Team for two and a half days of knowledge-sharing, fun, networking, games with prizes, and “aha” moments in beautiful San Diego on October 9-11, 2024.
You don’t want to miss this one-of-a-kind learning opportunity. Get away from all those daily responsibilities and immerse yourself in a fun and intensive conference with plenty of networking opportunities.
Attendees will leave this conference with new tools and a more complete understanding of the latest advances in diabetes care, from medications to technology to Medical Nutrition Therapy!
Each day, we provide a healthy breakfast, including fresh coffee, to kick off your morning. Our instructors co-teach the content to keep things fresh and lively. Plus, we play DiaBingo to reinforce key content and give away prizes. In addition, we provide plenty of movement breaks led by volunteers from the audience. Did we mention delicious lunches and a conference meeting space just minutes from San Diego Bay?
Friend Discount: 3 or more only $559-$799 (based on registration package) per person. Email us at [email protected] with the name and email of each registrant to get the discount!
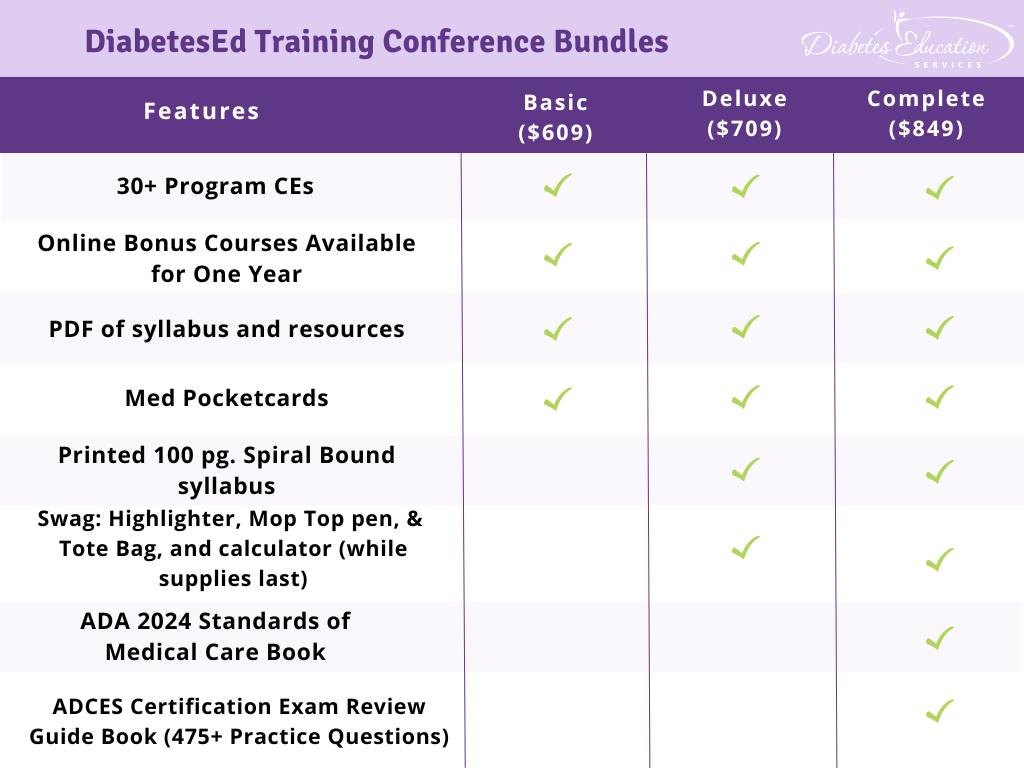
Time: The course is Wednesday through Friday. Join us for breakfast at 7:00 a.m. each day. The class begins at 8:00 a.m. and ends at 5:00 p.m. on Wednesday and Thursday and at 3:00 p.m. on Friday.
Accreditation: Diabetes Education Services is an approved provider by the California Board of Registered Nursing, Provider 12640, and our CPEU courses have received Prior Approval* from the Commission of Dietetic Registration (CDR), Provider DI002. Since our CPEU courses received Prior approval* from the CDR, these CPEU courses satisfy the CE requirements for the CDCES /BC-ADM regardless of your profession!
The use of DES products does not guarantee the successful passage of the certification exam. CBDCE and ADCES do not endorse any preparatory or review materials for the CDCES or BC-ADM exams, except for those published by CBDCE & ADCES.

KR is a 49-year-old with a learning disability and diabetes for over 20 years and is taking the following classes of diabetes medications at maximum doses; SGLT-2, Sulfonylurea, GLP-1 RA, biguanide and a TZD. Over the past month, KR’s blood glucose levels have increased to over 300 despite a 20-pound weight loss. The endocrinologist starts KR on basal insulin plus bolus insulin at each meal based on blood glucose and carbohydrates consumed. KR arrives for their education appointment in tears, saying “I feel completely overwhelmed and confused about all this insulin stuff.”
What is the best response?

Join Coach Beverly and Team for two and a half days of knowledge-sharing, fun, networking, games with prizes, and “aha” moments in beautiful San Diego on October 9-11, 2024.
You don’t want to miss this one-of-a-kind learning opportunity. Get away from all those daily responsibilities and immerse yourself in a fun and intensive conference with plenty of networking opportunities.
Attendees will leave this conference with new tools and a more complete understanding of the latest advances in diabetes care, from medications to technology to Medical Nutrition Therapy!
Each day, we provide a healthy breakfast, including fresh coffee, to kick off your morning. Our instructors co-teach the content to keep things fresh and lively. Plus, we play DiaBingo to reinforce key content and give away prizes. In addition, we provide plenty of movement breaks led by volunteers from the audience. Did we mention delicious lunches and a conference meeting space just minutes from San Diego Bay?
Friend Discount: 3 or more only $559-$799 (based on registration package) per person. Email us at [email protected] with the name and email of each registrant to get the discount!
Time: The course is Wednesday through Friday. Join us for breakfast at 7:00 a.m. each day. The class begins at 8:00 a.m. and ends at 5:00 p.m. on Wednesday and Thursday and at 3:00 p.m. on Friday.
Accreditation: Diabetes Education Services is an approved provider by the California Board of Registered Nursing, Provider 12640, and our CPEU courses have received Prior Approval* from the Commission of Dietetic Registration (CDR), Provider DI002. Since our CPEU courses received Prior approval* from the CDR, these CPEU courses satisfy the CE requirements for the CDCES /BC-ADM regardless of your profession!
The use of DES products does not guarantee the successful passage of the certification exam. CBDCE and ADCES do not endorse any preparatory or review materials for the CDCES or BC-ADM exams, except for those published by CBDCE & ADCES.
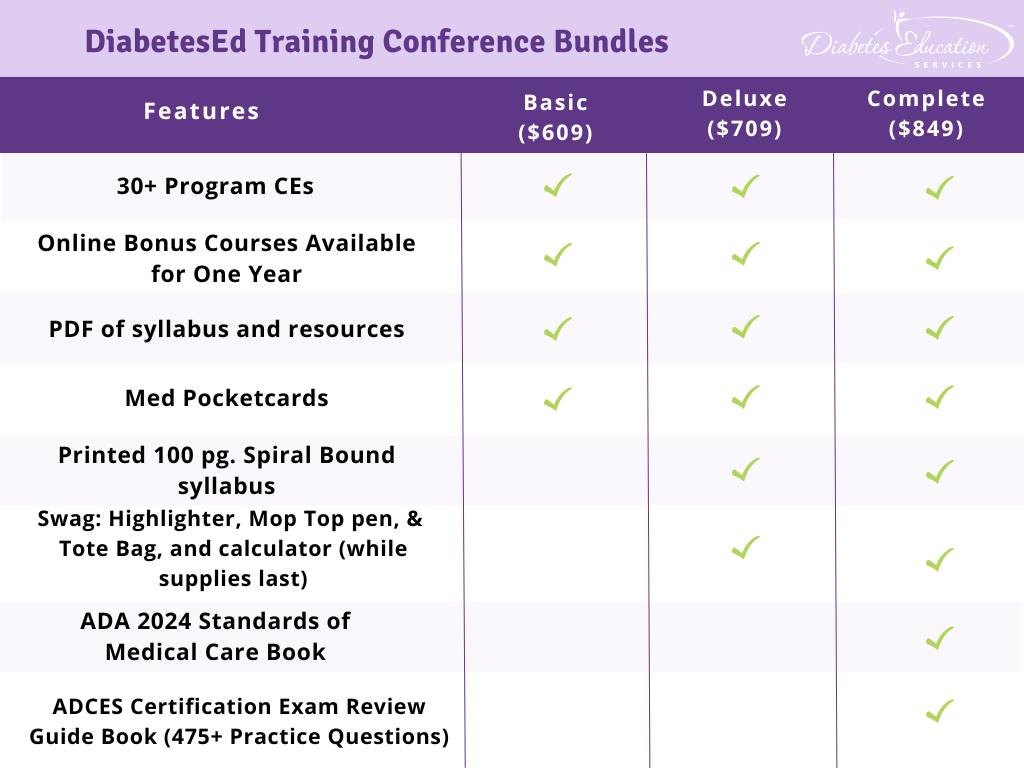
For last week’s practice question, we quizzed participants on the connection with hypoglycemia and hospitalizations. Almost all of the respondents chose the best answer. We want to clarify and share this important information, so you can pass it on to people living with diabetes and your colleagues, plus prepare for exam success!
Before we start though, if you don’t want any spoilers and haven’t tried the question yet, you can answer it below: Answer Question

Question: JR is 79 years old and takes insulin 3 times daily. Lately, they have been experiencing increased episodes of hypoglycemia.
Which of the following statements is true regarding hypoglycemia and the risk of hospitalization?
Answer Choices:
Answer 1 is incorrect. 1.4% chose this answer. “Hypoglycemia is a minor concern and rarely leads to hospitalization.” Hypoglycemia can lead to falls, confusion and loss of consciousness, all of which can precipitate hospitalization.
Answer 2 is incorrect. 1.4% of you chose this answer. “Only severe hypoglycemia results in hospitalization.” Even mild hypoglycemia can lead to falls and confusion, and if not treated, can worsen and result in loss of consciousness and hospitalization.
Answer 3 is correct. About 93.95% of respondents chose this. “Hypoglycemia, whether mild or severe, significantly increases the risk of hospitalization.” GREAT JOB! This is the best answer. Creating a collaborative plan to PREVENT hypoglycemia is especially important for people taking secretagogues or using insulin therapy.
Finally, Answer 4 is incorrect. 3.26% chose this answer. “Hospitalization from hypoglycemia is mainly a concern for people with type 1 diabetes.” Older people with type 2 diabetes and diminished renal function, who use insulin or secretagogues to lower glucose levels, are at risk of severe hypoglycemia and require close glucose monitoring.
We hope you appreciate this week’s rationale! Thank you so much for taking the time to answer our Question of the Week and participate in this fun learning activity!

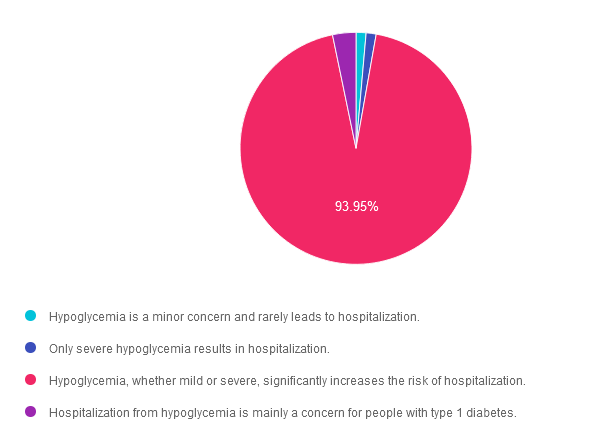
Join Coach Beverly and Team for two and a half days of knowledge-sharing, fun, networking, games with prizes, and “aha” moments in beautiful San Diego on October 9-11, 2024.
You don’t want to miss this one-of-a-kind learning opportunity. Get away from all those daily responsibilities and immerse yourself in a fun and intensive conference with plenty of networking opportunities.
Attendees will leave this conference with new tools and a more complete understanding of the latest advances in diabetes care, from medications to technology to Medical Nutrition Therapy!
Each day, we provide a healthy breakfast, including fresh coffee, to kick off your morning. Our instructors co-teach the content to keep things fresh and lively. Plus, we play DiaBingo to reinforce key content and give away prizes. In addition, we provide plenty of movement breaks led by volunteers from the audience. Did we mention delicious lunches and a conference meeting space just minutes from San Diego Bay?
Friend Discount: 3 or more only $559-$799 (based on registration package) per person. Email us at [email protected] with the name and email of each registrant to get the discount!
Time: The course is Wednesday through Friday. Join us for breakfast at 7:00 a.m. each day. The class begins at 8:00 a.m. and ends at 5:00 p.m. on Wednesday and Thursday and at 3:00 p.m. on Friday.
Accreditation: Diabetes Education Services is an approved provider by the California Board of Registered Nursing, Provider 12640, and our CPEU courses have received Prior Approval* from the Commission of Dietetic Registration (CDR), Provider DI002. Since our CPEU courses received Prior approval* from the CDR, these CPEU courses satisfy the CE requirements for the CDCES /BC-ADM regardless of your profession!
The use of DES products does not guarantee the successful passage of the certification exam. CBDCE and ADCES do not endorse any preparatory or review materials for the CDCES or BC-ADM exams, except for those published by CBDCE & ADCES.

During a hospital stay, JR, who has no prior history of diabetes experiences elevated blood glucose levels.
Which of the following factors is the most likely cause of this hyperglycemia during hospitalization?

Glucose control in the hospital matters! This course provides participants with a step-by-step approach to safely & effectively implement Basal-Bolus Insulin Therapy in the inpatient setting. We discuss appropriate insulin dosing based on the individual’s clinical presentation & apply dosing strategies to a variety of case studies. Included are hard-to-manage situations that commonly occur in hospital settings & a discussion of solutions that will keep people living with diabetes safe & get glucose levels to goal. In addition, sample basal/bolus & insulin drip guidelines plus lots of resource articles are included.
Objectives:
Learning Outcome:
The diabetes care team will gain insights into adjusting basal-bolus therapy for inpatients with diabetes to improve glycemic management.
Target Audience:
This course is a knowledge-based activity designed for individuals or groups of diabetes professionals, including RNs, RDs/RDNs, Pharmacists, Nurse Practitioners, Clinical Nurse Specialists, Physician Assistants, and other healthcare providers interested in staying up to date on current practices of care for people with prediabetes, diabetes, and other related conditions. The practice areas for RDs/RDNs for CDR reporting are healthcare, preventative care, wellness, and, lifestyle along with, education and research.
CDR Performance Indicators:
Instructor: Beverly Thomassian RN, MPH, CDCES, has been Board Certified in Advanced Diabetes Management for over 15 years. She is an Associate Clinical Professor at UCSF, a working educator, and a nationally recognized diabetes expert.
Accreditation: Diabetes Education Services is an approved provider by the California Board of Registered Nursing, Provider 12640, and our Level 4 | Basal Bolus Therapy in Hospitals awards 1.5 CPEUs in accordance with the Commission on Dietetic Registration’s CPEU Prior Approval Program.
The use of DES products does not guarantee the successful passage of the certification exam. CBDCE and ADCES do not endorse any preparatory or review materials for the CDCES or BC-ADM exams, except for those published by CBDCE & ADCES.
For last week’s practice question, we quizzed participants on older adults and goals for care. 62% of respondents chose the best answer. We want to clarify and share this important information, so you can pass it on to people living with diabetes and your colleagues, plus prepare for exam success!
Before we start though, if you don’t want any spoilers and haven’t tried the question yet, you can answer it below: Answer Question

Question: TS is 82 years old, living with type 1 diabetes for the past 56 years. They present to the clinic with their family for diabetes care and education. TS’s last A1c was 7.6%, with a Time in the Range of 64% and Time below the Range of 1%. TS lives alone and self-manages their medications, and the family reports concern of potential missed insulin doses and dietary intake patterns are less consistent over the past few months.
Considering diabetes management in older adults, what recommendations would you give TS and his family?
Answer Choices:
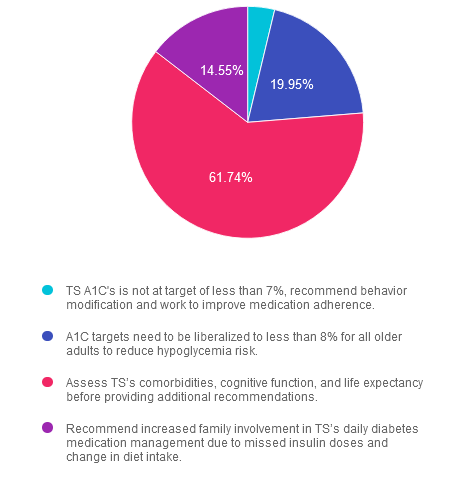
Answer 1 is incorrect. 3.76% chose this answer. “TS’s A1c is not at target of less than 7%, recommend behavior modifications and work to improve medication adherence.” Answer 1 is incorrect. The American Diabetes Association 2024 Standards of Care recommends personalizing glycemic targets for adults over 65 depending on comorbidities, cognitive and functional status, and living situations. An A1c of less than 7% may not be appropriate.
Answer 2 is incorrect. 19.95% of you chose this answer. “A1c targets should be liberalized to less than 8% for all older adults to reduce hypoglycemia risk.” Answer 2 is incorrect. While it is true we may liberalize A1c targets for older adults to prevent hypoglycemia, it is not the best answer. Older adults over 65 who are otherwise healthy, have stable coexisting chronic conditions, and have intact functional and cognitive status may benefit from lower glycemic goals (less than 7 to less than 7.5%).
Answer 3 is correct. About 61.74% of respondents chose this. “Assess TS’s comorbidities, cognitive function, and life expectancy before providing additional recommendations.” Answer 3 is the correct action. In older adults with diabetes, assessing comorbidities, cognitive function, and life expectancy is important to allow for the personalization of diabetes management recommendations and care goals.
Finally, Answer 4 is incorrect. 14.55% chose this answer. “Recommend increased family involvement in TS’s daily diabetes medication management due to missed insulin doses and change in diet intake.” Answer 4 is incorrect. We need more information to conclude that TS needs additional family support today. Completing a comprehensive evaluation, including cognitive function screening, is essential before providing recommendations.
We hope you appreciate this week’s rationale! Thank you so much for taking the time to answer our Question of the Week and participate in this fun learning activity!

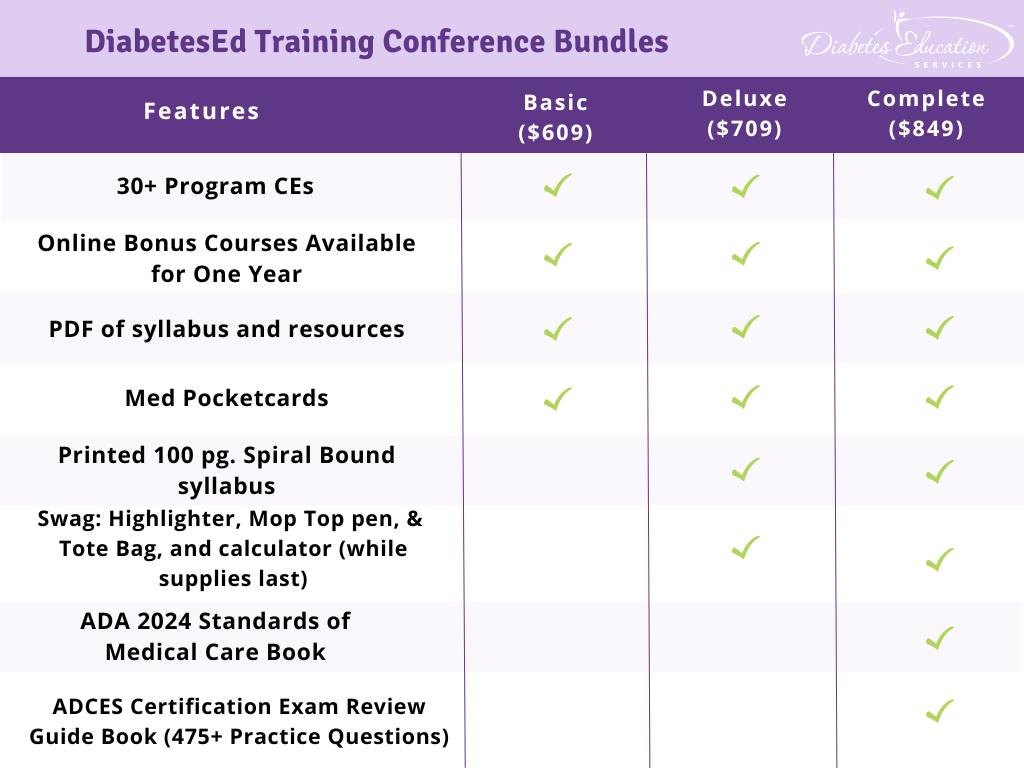
Join Coach Beverly and Team for two and a half days of knowledge-sharing, fun, networking, games with prizes, and “aha” moments in beautiful San Diego on October 9-11, 2024.
You don’t want to miss this one-of-a-kind learning opportunity. Get away from all those daily responsibilities and immerse yourself in a fun and intensive conference with plenty of networking opportunities.
Attendees will leave this conference with new tools and a more complete understanding of the latest advances in diabetes care, from medications to technology to Medical Nutrition Therapy!
Each day, we provide a healthy breakfast, including fresh coffee, to kick off your morning. Our instructors co-teach the content to keep things fresh and lively. Plus, we play DiaBingo to reinforce key content and give away prizes. In addition, we provide plenty of movement breaks led by volunteers from the audience. Did we mention delicious lunches and a conference meeting space just minutes from San Diego Bay?
Friend Discount: 3 or more only $559-$799 (based on registration package) per person. Email us at [email protected] with the name and email of each registrant to get the discount!
Time: The course is Wednesday through Friday. Join us for breakfast at 7:00 a.m. each day. The class begins at 8:00 a.m. and ends at 5:00 p.m. on Wednesday and Thursday and at 3:00 p.m. on Friday.
Accreditation: Diabetes Education Services is an approved provider by the California Board of Registered Nursing, Provider 12640, and our CPEU courses have received Prior Approval* from the Commission of Dietetic Registration (CDR), Provider DI002. Since our CPEU courses received Prior approval* from the CDR, these CPEU courses satisfy the CE requirements for the CDCES /BC-ADM regardless of your profession!
The use of DES products does not guarantee the successful passage of the certification exam. CBDCE and ADCES do not endorse any preparatory or review materials for the CDCES or BC-ADM exams, except for those published by CBDCE & ADCES.

JR is 79 years old and takes insulin 3 times daily. Lately, they have been experiencing increased episodes of hypoglycemia.
Which of the following statements is true regarding hypoglycemia and the risk of hospitalization?

Join Coach Beverly and Team for two and a half days of knowledge-sharing, fun, networking, games with prizes, and “aha” moments in beautiful San Diego on October 9-11, 2024.
You don’t want to miss this one-of-a-kind learning opportunity. Get away from all those daily responsibilities and immerse yourself in a fun and intensive conference with plenty of networking opportunities.
Attendees will leave this conference with new tools and a more complete understanding of the latest advances in diabetes care, from medications to technology to Medical Nutrition Therapy!
Each day, we provide a healthy breakfast, including fresh coffee, to kick off your morning. Our instructors co-teach the content to keep things fresh and lively. Plus, we play DiaBingo to reinforce key content and give away prizes. In addition, we provide plenty of movement breaks led by volunteers from the audience. Did we mention delicious lunches and a conference meeting space just minutes from San Diego Bay?
Friend Discount: 3 or more only $559-$799 (based on registration package) per person. Email us at [email protected] with the name and email of each registrant to get the discount!
Time: The course is Wednesday through Friday. Join us for breakfast at 7:00 a.m. each day. The class begins at 8:00 a.m. and ends at 5:00 p.m. on Wednesday and Thursday and at 3:00 p.m. on Friday.
Accreditation: Diabetes Education Services is an approved provider by the California Board of Registered Nursing, Provider 12640, and our CPEU courses have received Prior Approval* from the Commission of Dietetic Registration (CDR), Provider DI002. Since our CPEU courses received Prior approval* from the CDR, these CPEU courses satisfy the CE requirements for the CDCES /BC-ADM regardless of your profession!
The use of DES products does not guarantee the successful passage of the certification exam. CBDCE and ADCES do not endorse any preparatory or review materials for the CDCES or BC-ADM exams, except for those published by CBDCE & ADCES.

With fall around the corner, we have an exciting line-up of announcements and activities to share with our community.
We are overjoyed to welcome Jessica Jones, MS, RDN, CDCES, to our San Diego DiabetesEd speaking team. Jessica’s unique blend of clinical expertise and Health At Every Size approach to nutrition therapy promises to bring a fresh perspective to our team. Get to know Jessica better in our exclusive interview below.
In addition, enjoy highlights from the most recent ADCES meeting in New Orleans. This year, a particular focus was on promoting inclusivity and individualized care management. Our on-the-scene expert, Christine Craig, MS, RDN, CDCES, provides a focused review of her 3 top takeaways from this annual meeting.
For those renewing your CDCES, please note the additional continuing education requirement on ADA Standards of Care. Read our article below to learn more.
As we kick off Hispanic Heritage Month in September, let’s take this opportunity to celebrate this community’s rich culture and raise awareness of the health disparities that need attention.
We invite you to challenge yourself with our question and rationale of the week and consider joining our three-day live training program in beautiful San Diego.
Lastly, we hope you can pop in for our CDCES or BC-ADM Prep webinars, which Coach Beverly will broadcast from her international office in Portugal.
We are grateful for your continued support and participation in our community. With best wishes for your health and happiness,
Warmly, Coach Beverly, Bryanna, Tiffany, and Christine |
Featured Articles

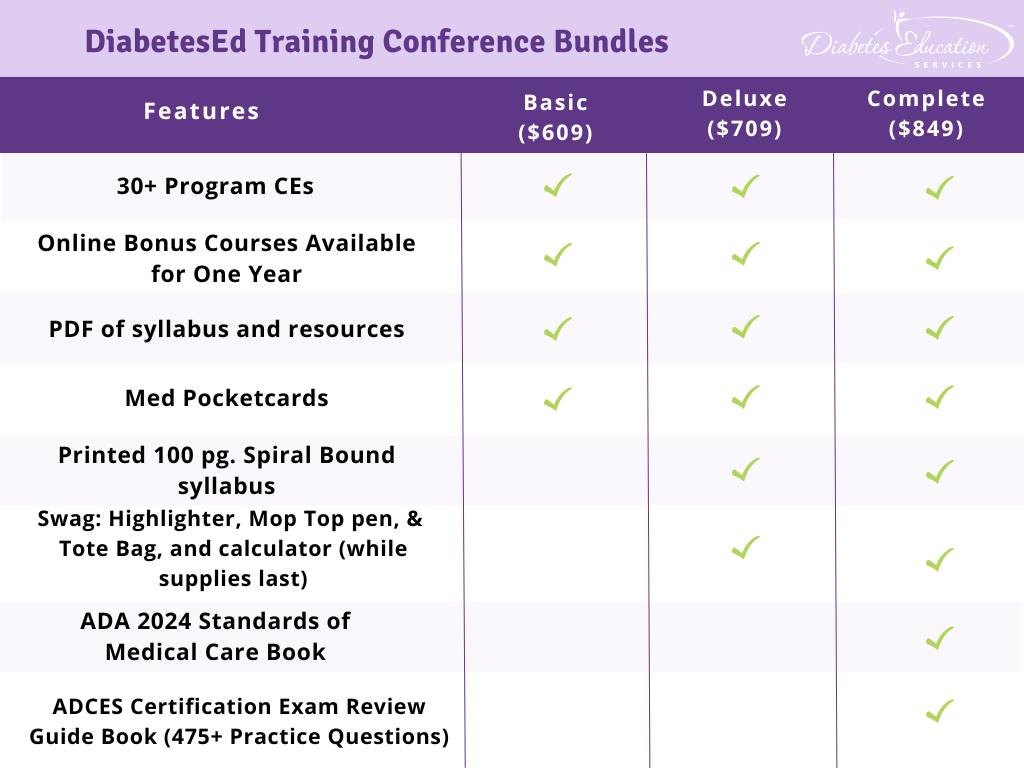
Join Coach Beverly and Team for two and a half days of knowledge-sharing, fun, networking, games with prizes, and “aha” moments in beautiful San Diego on October 9-11, 2024.
You don’t want to miss this one-of-a-kind learning opportunity. Get away from all those daily responsibilities and immerse yourself in a fun and intensive conference with plenty of networking opportunities.
Attendees will leave this conference with new tools and a more complete understanding of the latest advances in diabetes care, from medications to technology to Medical Nutrition Therapy!
Each day, we provide a healthy breakfast, including fresh coffee, to kick off your morning. Our instructors co-teach the content to keep things fresh and lively. Plus, we play DiaBingo to reinforce key content. In addition, we provide plenty of movement breaks led by volunteers from the audience. Did we mention delicious lunches and a conference meeting space just minutes from San Diego Bay?
Friend Discount: 3 or more only $559-$799 (based on registration package) per person. Email us at [email protected] with the name and email of each registrant to get the discount!
Time: The course is Wednesday through Friday. Join us for breakfast at 7:00 a.m. each day. The class begins at 8:00 a.m. and ends at 5:00 p.m. on Wednesday and Thursday and at 3:00 p.m. on Friday.
Accreditation: Diabetes Education Services is an approved provider by the California Board of Registered Nursing, Provider 12640, and our CPEU courses have received Prior Approval* from the Commission of Dietetic Registration (CDR), Provider DI002. Since our CPEU courses received Prior approval* from the CDR, these CPEU courses satisfy the CE requirements for the CDCES /BC-ADM regardless of your profession!
The use of DES products does not guarantee the successful passage of the certification exam. CBDCE and ADCES do not endorse any preparatory or review materials for the CDCES or BC-ADM exams, except for those published by CBDCE & ADCES.

TS is 82 years old, living with type 1 diabetes for the past 56 years. They present to the clinic with their family for diabetes care and education. TS’s last A1C was 7.6%, with a Time in the Range of 64% and Time below the Range of 1%. TS lives alone and self-manages their medications, and the family reports concern of potential missed insulin doses and dietary intake patterns are less consistent over the past few months.
Considering diabetes management in older adults, what recommendations would you give TS and his family?

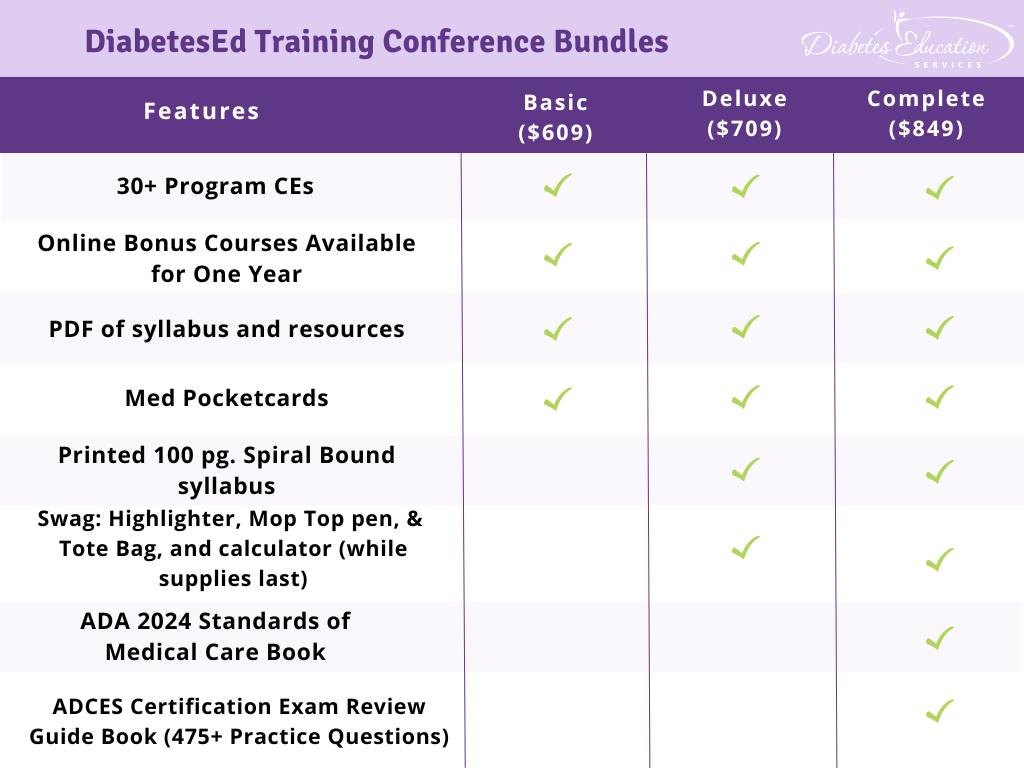
Join Coach Beverly and Team for two and a half days of knowledge-sharing, fun, networking, games with prizes, and “aha” moments in beautiful San Diego on October 9-11, 2024.
You don’t want to miss this one-of-a-kind learning opportunity. Get away from all those daily responsibilities and immerse yourself in a fun and intensive conference with plenty of networking opportunities.
Attendees will leave this conference with new tools and a more complete understanding of the latest advances in diabetes care, from medications to technology to Medical Nutrition Therapy!
Each day, we provide a healthy breakfast, including fresh coffee, to kick off your morning. Our instructors co-teach the content to keep things fresh and lively. Plus, we play DiaBingo to reinforce key content. In addition, we provide plenty of movement breaks led by volunteers from the audience. Did we mention delicious lunches and a conference meeting space just minutes from San Diego Bay?
Friend Discount: 3 or more only $559-$799 (based on registration package) per person. Email us at [email protected] with the name and email of each registrant to get the discount!
Time: The course is Wednesday through Friday. Join us for breakfast at 7:00 a.m. each day. The class begins at 8:00 a.m. and ends at 5:00 p.m. on Wednesday and Thursday and at 3:00 p.m. on Friday.
Accreditation: Diabetes Education Services is an approved provider by the California Board of Registered Nursing, Provider 12640, and our CPEU courses have received Prior Approval* from the Commission of Dietetic Registration (CDR), Provider DI002. Since our CPEU courses received Prior approval* from the CDR, these CPEU courses satisfy the CE requirements for the CDCES /BC-ADM regardless of your profession!
The use of DES products does not guarantee the successful passage of the certification exam. CBDCE and ADCES do not endorse any preparatory or review materials for the CDCES or BC-ADM exams, except for those published by CBDCE & ADCES.