The world of diabetes technology is advancing at a record pace. There is no doubt that technology intends to make life with diabetes a bit easier. In the United States, over 50% of adults living with diabetes have experienced some level of diabetes distress.¹ The impact of diabetes technology on mental well-being is complicated. Diabetes technology, including insulin pumps, continuous glucose monitors (CGMs), and connected insulin pens, can either lessen or aggravate diabetes distress.

Understanding Diabetes Distress
The American Diabetes Association (ADA) defines diabetes distress as “significant negative psychological reactions related to emotional burdens and worries specific to an individual’s experience in having to manage a demanding chronic condition such as diabetes.”.² Diabetes distress is a natural reaction to the daily burden of managing diabetes. Signs of diabetes distress can include avoiding blood glucose monitoring, omitting medications, and struggling to achieve personal hemoglobin A1c targets.
The ADA recommends screening for diabetes distress at least annually. More frequent screening is recommended if clients are not meeting treatment goals, develop diabetes-related complications, and during times of life transitions.²
To access these validated diabetes distress screening tools in English and Spanish, I encourage you to visit this helpful website, DiabetesDistress.org
- Diabetes Distress Scale (DDS-17)
- Type 1 Diabetes Distress Scale (T1-DDS)
- The Type 2-Diabetes Distress Assessment System (T2-DDAS)
Can Technology Improved Diabetes Distress?
Let’s explore how diabetes technology can have a positive impact on diabetes distress.
✅ CGMs: With current CGMs, fewer fingerstick readings are needed to make treatment decisions. CGMs provide information on blood glucose trends and impending hyperglycemia or hypoglycemia, creating more peace of mind.
✅ Record Keeping: Various forms of diabetes technology can log blood glucose values, insulin doses, site changes, and total daily doses of insulin. This eliminates the need for clients to worry about detailed record-keeping.
✅ Automated Insulin Delivery: Automated insulin pumps can decrease decision fatigue by making automated adjustments to both basal and correction insulin doses. This approach to insulin delivery can also benefit individuals with an active lifestyle. Utilizing wearable insulin delivery devices and algorithms can reduce the mental burden of diabetes self-management.
✅ Connectivity: Remote data sharing supports communication with parents, caregivers, and friends to create a diabetes support team. Connectivity with healthcare providers enhances communication with the care team, allowing adjustments to treatment plans between clinic visits.
✅ Empowerment: The data trends can empower individuals living with diabetes to take control and gain confidence in making and evaluating medication and lifestyle adjustments in response to changes in glycemic control.
Can Technology Worsen Diabetes Distress?
As diabetes healthcare professionals, it is important to understand how diabetes technology can negatively impact diabetes distress.
❌ Information Overload: Diabetes technology generates an enormous amount of data. This can cause distress by constantly feeling the need to monitor glucose trends and numbers throughout the day and night, leading to feelings of anxiety and overwhelm.
❌ Alarms: Alarms on diabetes technology are rooted in safety, but for those living with these devices, this can lead to diabetes distress. Alarms can disrupt sleep or bring unwanted attention from others in public. Erroneous alarms for hyperglycemia or hypoglycemia can cause stress, frustration, and alarm fatigue.
❌ Perfectionism: Diabetes technology provides a continuous insight into glycemic control, which for some can create a need for perfection. Some clients feel like they fail when they don’t reach their time-in-range goal each day.
❌ Physical Impact: Wearable devices not only carry a psychological burden but can also cause physical distress. Skin irritation and allergic reactions to adhesives cause physical pain and embarrassment. Those who wish to keep diabetes private, wearing a CGM, insulin pump, or other wearable device that puts diabetes on display, causing distress.
❌ Technical issues: Losing connectivity with CGMs or an AID system can cause frustration and make it challenging to achieve optimal glycemic control. Insurance coverage, prior authorizations, out-of-pocket costs, and access to supplies for diabetes technology can all contribute to or worsen diabetes distress.
Diabetes Healthcare Professionals Help – Recognize and Address
The 7A’s Framework provides a useful interview tool when assessing for Diabetes Distress:
- Aware: Be aware of diabetes distress.
- Ask: Ask about diabetes distress.
- Assess: Use a validated screening tool for assessment.
- Advise: Explain diabetes distress.
- Assist: Develop an action plan.
- Assign: If you are not equipped to help, assign the client to another healthcare professional.
- Arrange: Set up follow-up as needed. 3
Here are some other actionable tips you can use to help those with diabetes distress:
- Refer clients to local or virtual diabetes support groups.
- Discuss with clients that diabetes distress is common and not a character flaw or failure
- Collaborate to choose the best technology based on their technology readiness, skill level, and comfort level.
- Set realistic goals for time-in-range and other data metrics.
- Educate clients on how to troubleshoot their devices regarding alarms or connectivity issues.
- Support a healthy relationship with diabetes tech.
References
Alexander, D.S., Saelee, R., Betsy Rodriguez, B., Koyama, A. K., Cheng, Y. J., Tang, S., Rutkowski, R. E., & Bullard, K. M. (2025). Diabetes distress among US adults with diagnosed diabetes, 2021. Preventing Chronic Disease: Public Health Research, Practice, and Policy, 22(E07), 1-7. https://www.cdc.gov/pcd/issues/2025/24_0287.htm#:~:text=Among%20US%20adults%20with%20diabetes%2C%20an%20estimated%201.6%20million%20(6.6,income%20compared%20with%20their%20counterparts.
- American Diabetes Association Professional Practice Committee. (2025). Facilitating positive health behaviors and well-being to improve health outcomes: Standards of care in diabetes—2025. Diabetes Care, 48(Supplement_1): S86–S127. https://diabetesjournals.org/care/article/48/Supplement_1/S86/157563/5-Facilitating-Positive-Health-Behaviors-and-Well?searchresult=1
- American Diabetes Association. (n.d.). Professional development: Behavioral health toolkit. https://professional.diabetes.org/professional-development/behavioral-mental-health/behavioral-health-toolkit
- Healing through Connection for Healthcare Professionals by Beverly Thomassian
Learn More From the Experts:
Coach Beverly Thomassian, Dr. Diana Isaacs, & Christine Craig
Virtual DiabetesEd Training Conference | April 15th-17th, 2026
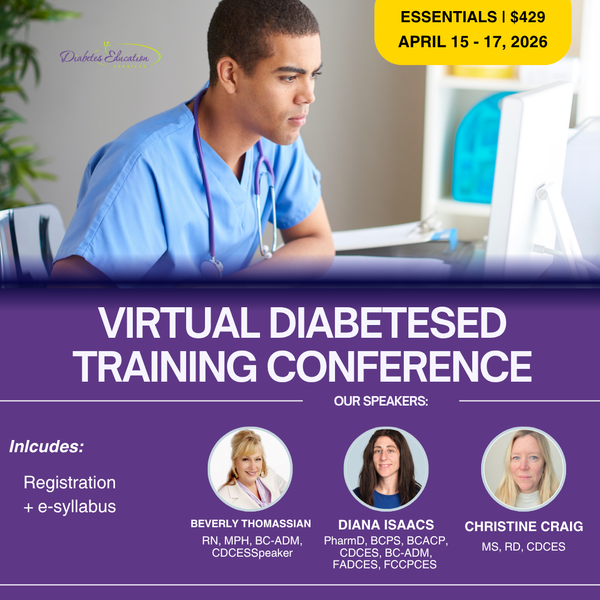
Gain fresh insights, practical tools, and a deeper understanding of the latest in person-centered diabetes care. Our expert team brings the ADA Standards of Care to life—covering medications, behavior change, technology, and more!
Registration Options at a Glance
- 📜 Essentials: Includes registration and electronic syllabus.
- 🌟 Deluxe: Includes registration, electronic syllabus, and the ADA Standards Book for deeper study.
- 🏆 Complete: Best value! Includes everything listed above, plus the ADCES Review Guide of over 400 practice questions for exam prep.
Registration Fee includes
- 🎤 3 days of engaging, expert-led education
- 📘 100-page electronic syllabus +
- 🎓 12 FREE bonus online courses ($375 value) to boost your prep


