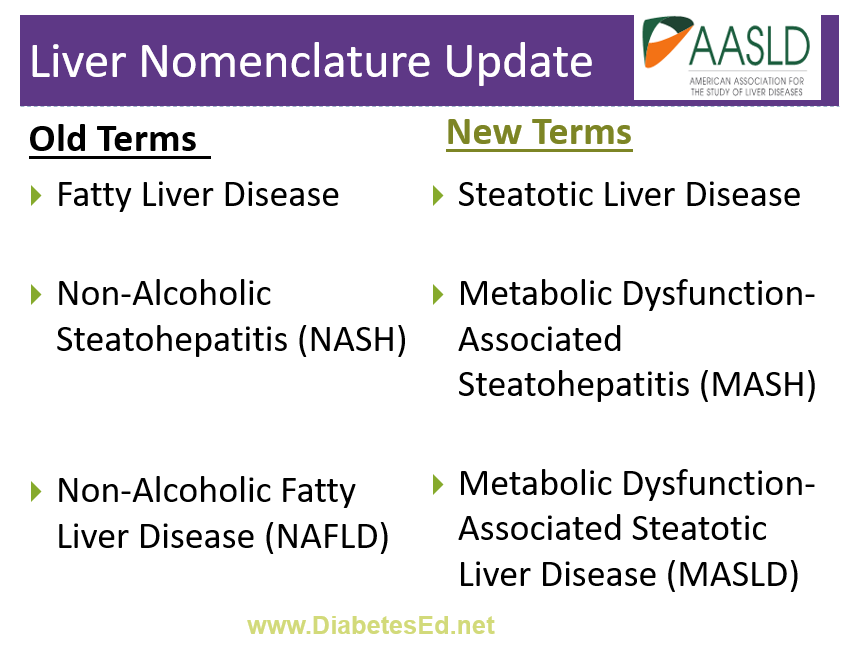
The American Association for the Study of Liver Diseases recently announced that they are updating their terms for Non-Alcoholic Steatohepatitis (NASH) and Non-Alcoholic Fatty Liver Disease (NAFLD).
Since NAFLD is considered the “hepatic manifestation of metabolic syndrome,” the organization wants the terminology to better reflect this metabolic inflammation and update the language to remove the stigma associated with the terms “fatty” and “non-alcoholic.”
According to the American Diabetes Association, NAFLD is prevalent in more than 70% of people living with diabetes. Early detection and intervention can decrease fat accumulation in the liver and lead to improved health. As diabetes care and education specialists, we can increase awareness and screenings while promoting lifestyle changes and medication therapy to save lives. One way to start the conversation is to share this updated Liver Nomenclature List with your colleagues.
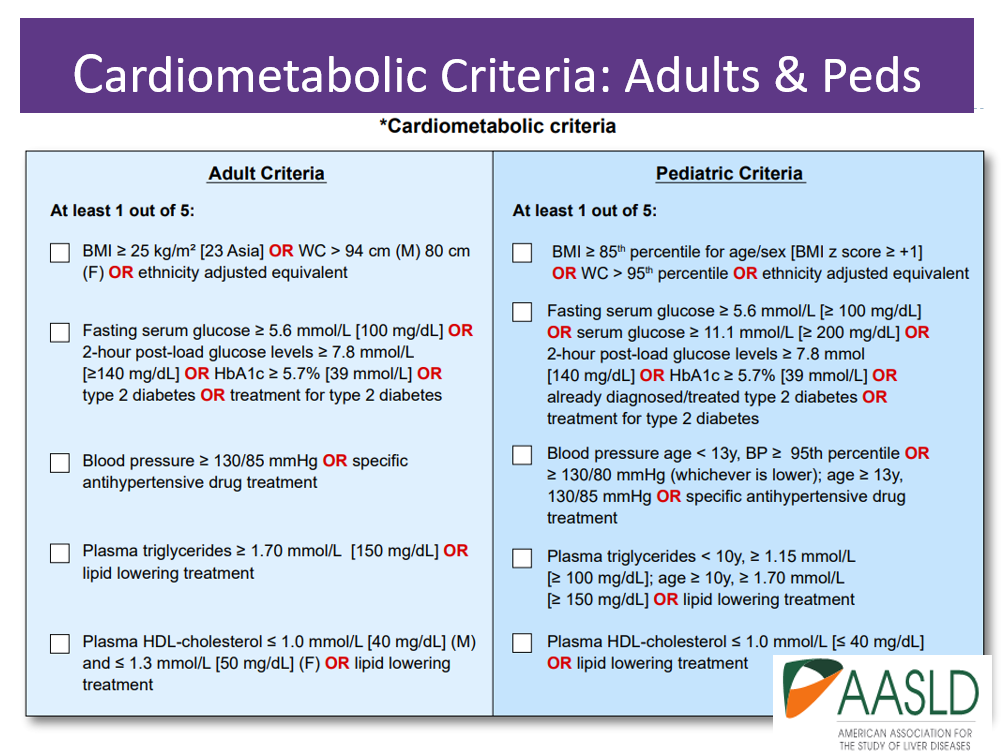
The new names, MASH and MAFLD, take into account the presence of liver disease along with cardiometabolic risk factors such as body weight, glucose levels, blood pressure, triglycerides, and HDL cholesterol levels (see CardioMetabolic table below).
Updated Liver Nomenclature List:
- Say goodbye to “Fatty Liver Disease”. The new overarching term to encompass the various presentations of liver steatosis is Steatotic Liver Disease (SLD)
- Instead of “Fatty Liver” use the term Hepatic Steatosis. This is a more technical and less stigmatizing term that simply means that the liver has an excessive amount of fat.
- The term NASH is now MASH – MASH stands for Metabolic Dysfunction-Associated Steatohepatitis. This name emphasizes that the condition is a metabolic condition not related to alcohol consumption.
- No more NAFLD. The updated term is MASLD (pronunciation: Ma-zuld), which stands for Metabolic Dysfunction-Associated Steatotic Liver Disease. This term recognizes the various risk factors beyond alcohol consumption, such as body weight, insulin resistance, and other cardiometabolic risk factors.
- The alcohol intake threshold for Alcohol-related Liver Disease ALD starts with a weekly intake of 140 g (10 drinks) for females and 210 g (15 drinks) for males.
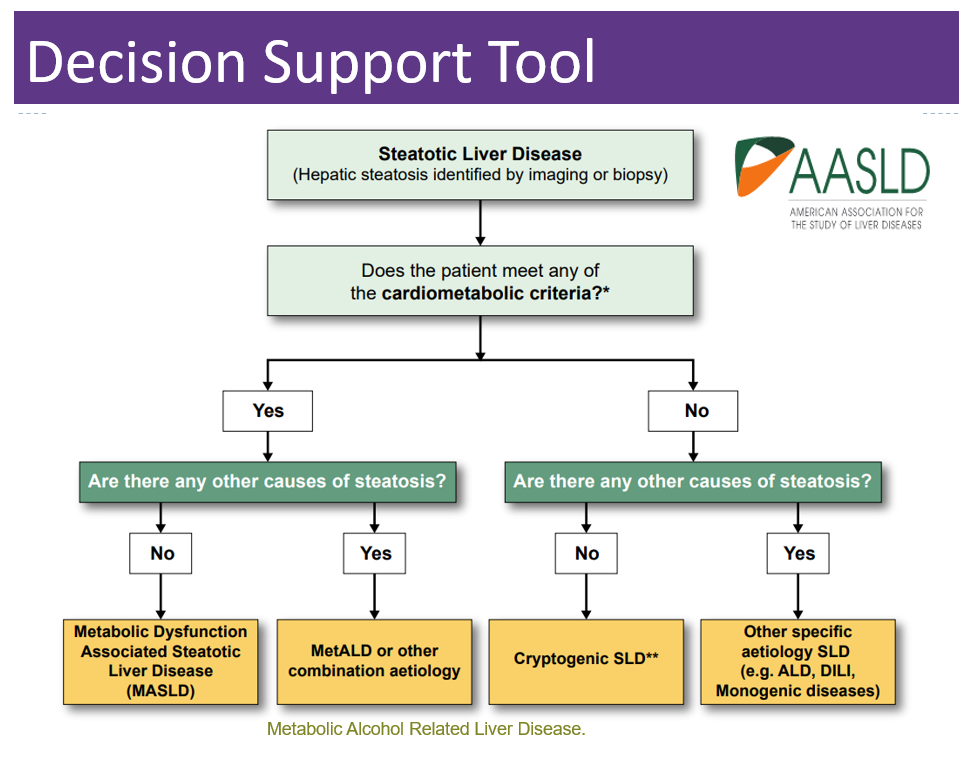
- Someone can have MASLD and it can be due to metabolic factors (MASLD) or it can be considered MetALD (pronunciation: Met A-L-D) predominant if they meet the alcohol intake threshold.
- There are other factors that can cause Steatotic Liver Disease (SLD), including drug-induced, genetic conditions and other unknown reasons (see algorithm below).
Below is a summary chart from the AADSL that reflects these important changes.
These new terms may not be universally accepted at first and the choice of name may vary by region and among healthcare professionals. Regardless of the name used, the management and understanding of the condition remain crucial to screening, identifying, and treating Steatotic Liver Disease.
Want to learn more about the GI System and Diabetes?
From the Gut to the Butt – Exploring the GI System FREE Webinar
Now Recorded & Ready to Watch

Coach Bev invites you to join this 60-minute webinar that covers gastrointestinal health from top to bottom. Topics include; fatty liver disease diagnosis and treatment, intestinal complications associated with diabetes, keeping the microbiome healthy, and more. Join us to explore the magnificent wonders of diabetes and the gut.
Getting to the Gut Topics:
- From the Mouth to Intestines: Periodontal disease, Gastroparesis, Fatty liver disease, pancreas disorders
- Intestine as an Endocrine Organ & Bacterial Host
- NASH Treatment Options including lifestyle and pharmacotherapy
- State the relationship between gut health, microbiome and diabetes and inflammation
- Describe 3 strategies to get our microbiome back to better health.
Can’t make it live? No worries. We will send post the recorded version to the Online University within 24 hours of the broadcast
Instructor: Beverly Thomassian RN, MPH, CDCES, has been Board Certified in Advanced Diabetes Management for over 20 years. She is an Associate Clinical Professor at UCSF, a working educator, and a nationally recognized diabetes expert. She has a Master’s Degree in Public Health from UCLA, with a focus on behavioral health and education.
All hours earned count toward your CDCES Accreditation Information
Sign up for Diabetes Blog Bytes – we post one daily Blog Byte from Monday to Friday. And of course, Tuesday is our Question of the Week. It’s Informative and FREE! Sign up below!
The use of DES products does not guarantee the successful passage of the CDCES exam. CBDCE does not endorse any preparatory or review materials for the CDCES exam, except for those published by CBDCE.









