
Written by Diana Isaacs, PharmD, BCPS, BC-ADM, BCACP, CDCES & ADCES 2020 Diabetes Educator of the year
The cost of insulin is a real problem. It can lead to insulin rationing and at its worst, people have died due to a lack of insulin.
A recent survey reported that 26% of respondents living in the US rationed insulin at last once in the last year.
The retail price for a box of insulin pens is about $500. Many people need more than one box of pens per month. Even with health insurance, people struggle to afford this. I remember one of my patients telling me she was only taking half of her prescribed dose of insulin glargine because her daughter was taking the same insulin and they both needed it. This just broke my heart!
Fortunately, the Food and Drug Administration (FDA), as well as drug companies, have heard the outcries from people who require insulin to live. In response, there are some helpful new programs that make insulin more affordable. However, it can be difficult to navigate all of the new information. To help make navigation easier, we have created an ADCES Access & Affordability page with Insulin Cost-Savings Resource Guide.
Here is a list of different strategies to access affordable insulin.
Why is insulin so expensive?
Insulin is considered a Biologic Drug, which makes it more expensive to produce.
Insulin is made from recombinant DNA technology, making it a biologic drug. Biologic drugs depend on unique manufacturing conditions that are proprietary and difficult to exactly replicate. Therefore, when the drug brand name patent expires, other companies can’t make true generics.
Until recently, the pathway for approval was called a follow-on biologic. This is how Basaglar (insulin glargine) and Admelog (insulin lispro) are classified. In March 2020, the FDA announced that regulatory requirements would change allowing for biosimilar products. This may ultimately increase market competitiveness in hopes to further reduce insulin prices. Basaglar and Admelog offer about a 15-20% discount from their reference products of Lantus and Humalog, respectively. Many argue these cost savings is just not enough.
Generic Insulins
Because insulin is a biologic drug, a true generic must come from the same manufacturer. Recently Lilly and Novo Nordisk have created generic insulins.
Lilly offers generics of insulin lispro, insulin lispro mix 75/25, and insulin lispro junior kwik pen.
Novo Nordisk offers generics of their insulin, which they are calling a “follow on Brand” and includes insulin apart and insulin aspart mix 70/30.
Both Lilly and Novo offer approximately a 50% cost savings from the original insulin product and the pharmacist can make an automatic substitution if you ask.
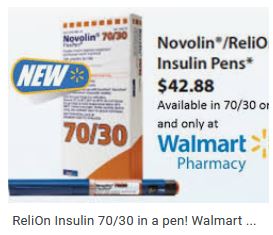
Walmart and some other pharmacies also offer ReliOn insulins. These include Novolin R, Novolin N, and Novolin 70/30. These are slower acting insulins that may predispose people to more hypoglycemia, but they are only $25/vial or $44/5 pack of pens and do not require a prescription in most states. Access to these insulins can be truly life-saving in some circumstances. Every person with diabetes needs to be aware that they can purchase these insulins without a prescription if they are ever out of insulin.

New Programs that Cap Insulin Pricing
Lilly announced a program capping insulin co-pays at $35/month for those paying with cash or commercial insurance. This will dramatically lower monthly costs for many people with diabetes.
Sanofi has a Valyou program that allows up to 10 vials or 10 boxes of insulin pens for a maximum of $99/month. Of note, Sanofi’s program will only work for those without insurance.
Novo Nordisk recently started the My $99 insulin program. What’s unique about this program is that it will work for those with commercial insurance or government plans like Medicare. Most other programs exclude people with Medicare. This program covers up to 3 vials or 2 packs of pens.
Co-Pay Cards
Most insulins offer a co-pay card which can bring down the price of insulin most commonly to $0 to $25/month depending on the manufacturer and type of insulin. For any person with a commercial insurance plan, it’s good to check if a co-pay card is available for the insulin before picking it up from the pharmacy.
The things to be aware of about these cards are that they have maximum savings and sometimes that is much less than the total cost of the insulin. Also, they only work for people with commercial insurance meaning they won’t for people without health insurance or that have a government insurance plan like Medicare. They also do not always work if the drug is not covered on the insurance plan. In that case, it would be preferable to switch to an insurance-covered on the insurance plan.
Patient Assistance Plans
These are programs offered through pharmaceutical companies for people without health insurance or that have Medicare but still struggle to pay for medications. There are various income requirements to be eligible, but depending on the program it can be 250-400% above the Federal poverty line. Many people are surprised to find that they are eligible, so this is a good option to look into which can make the insulin completely free. There is typically a packet of information that needs to be completed and then if eligible, the insulin is shipped to the prescriber’s office for the patient to pick up.
In summary, It can be challenging to keep all of this information straight. This is why I worked with a team of amazing diabetes care and education specialists at ADCES to create the ADCES Access & Affordability page with Insulin Cost-Savings Resource Guide. We update this resource frequently and it includes links to patient assistance programs, co-pay cards, and other cost savings programs. We hope you find it useful and that your patients with diabetes will benefit.
Special thanks to our guest contributor for this article: Diana Isaacs, PharmD, BCPS, BC-ADM, BCACP, CDCES & ADCES 2020 Diabetes Educator of the year
References:
Conner F, Pfiester E, Elliott J, Slama-Chaudhry A. Unaffordable insulin: patients pay the price. The Lancet Diabetes & Endocrinology 7 (10), 748,2019.
For a summary of all this information, see the ADCES Insulin Cost Savings Resources Page.
Sign up for Diabetes Blog Bytes – we post one daily Blog Byte from Monday to Friday. And of course, Tuesday is our Question of the Week. It’s Informative and FREE! Sign up below!
[yikes-mailchimp form=”1″]Accreditation: Diabetes Education Services is an approved provider by the California Board of Registered Nursing, Provider 12640, and Commission on Dietetic Registration (CDR), Provider DI002. Since these programs are approved by the CDR it satisfies the CE requirements for the CDCES regardless of your profession.*
The use of DES products does not guarantee the successful passage of the CDCES exam. CBDCE does not endorse any preparatory or review materials for the CDCES exam, except for those published by CBDCE.








