 What Action Can I Take to Prevent Cognitive Decline?
What Action Can I Take to Prevent Cognitive Decline?
During a follow-up medical nutrition therapy visit for diabetes, LC shares that they are concerned about their family history of both type 2 diabetes and dementia. They inquire about actions and interventions they can take to prevent cognitive decline.
Although LC may have inherited familial risk factors, it is well known that both type 1 and type 2 diabetes increase the risk of cognitive impairment and can double the risk for the development of Alzheimer’s disease and vascular dementia.1 The link between diabetes and cognitive impairment is multifaceted, with contributing factors including insulin resistance, chronic hyperglycemia, glucose variability with hypoglycemia, inflammation and oxidative stress, and cardiometabolic vascular risks. As diabetes care and education specialists, LC’s inquiry presents an opportunity to explore interventions that not only improve blood glucose but also support vascular and cognitive health.
Diabetes and the Brain Age Gap
A recent article published in Diabetes Care explored using neuroimaging to estimate brain age.1 The difference between estimated brain age and chronological age is known as the Brain Age Gap (BAG). The World Health Organization defines dementia as “a syndrome in which there is deterioration in cognitive function beyond what might be expected from the usual consequences of biological aging.”2
A higher BAG indicates a brain that appears older than its chronological age and is associated with an increased risk of cognitive decline and dementia. In individuals with type 2 diabetes, researchers found a significantly increased BAG of 2.29 years, while those with prediabetes showed an increase of 0.50 years.
The most significant BAG was observed in individuals with two or more cardiometabolic risk factors (3.08 years) and individuals with a baseline A1C above 8.0% (4.18 years).
The study also revealed the beneficial effects of participation in healthy lifestyle behaviors, including:
- avoiding smoking,
- abstaining from heavy drinking, and
- meeting physical guidelines of at least 150 minutes of moderate exercise (or 75 minutes of vigorous exercise) per week.
These lifestyle behaviors significantly reduced the BAG to 0.78 years. Notably, dietary factors were not assessed in this study. These findings highlight potential interventions for improving brain in individuals with diabetes, including optimizing glycemic and cardiometabolic measures, smoking cessation, alcohol moderation, and incorporating physical activity into daily routines.
Primary intervention includes optimizing glucose.
Mitochondria, often described as the “powerhouse” of our cells, play a vital role in producing energy for the brain and other parts of the body. Besides energy production, mitochondria help our brain cells adapt and can protect brain cells during short-term stress. Chronic hyperglycemia and hypoglycemia can create chronic oxidative stressors, also called “allostatic overload,” that can cause mitochondrial damage and neural dysfunction.2
This damage can impair brain function, leading to long-term issues with memory, thinking, and other neurological disorders. When mitochondria are overwhelmed by chronic stress, they lose their capacity to help the brain adapt, contributing to cognitive decline. Additionally, hyperglycemia can increase beta-amyloid production, which interferes with cell signaling—a key feature of dementia. A recent 2024 article in JAMA indicated that an A1c target of 6.5-7.5 %, in individuals with type 2 diabetes managed in primary care, was associated with lower dementia incidence3. Other studies have shown the highest dementia risk in individuals with A1c > 9%.4 While A1c is a frequent measure within reported studies, glycemic variability is also a known risk factor; using time in the range may be a better future indicator, especially in individuals with increased hypoglycemia risk.
Nutrition's Role in Brain Health
Nutrition also has a significant impact on cognitive function. For individuals with Alzheimer’s dementia and diabetes, the Mediterranean, DASH, (Dietary Approaches to Stop Hypertension), and MIND diet (Mediterranean-DASH Intervention for Neurodegenerative Delay) have promising outcomes showing reduced risk of cognitive decline.5
These diets are rich in antioxidants like flavonoids and carotenoids, omega-3 fatty acids, and plant-based foods, all linked with improved brain health. The MIND diet, has also been associated with improvements in cardiometabolic measures.6
As indicated above, cardiometabolic health has a strong association with an increased risk of dementia, and managing cardiovascular risk factors such as hypertension, dyslipidemia, smoking cessation, stress reduction, and adequate sleep can also all play a role in preserving cognitive function.
Cognitive decline and dementia can be a significant concern for individuals living with diabetes, but there are steps we can take to protect brain health.
Not all factors are modifiable, but managing contributing factors like chronic hyperglycemia, hypoglycemia severity and frequency, insulin resistance, and cardiometabolic risks can slow brain aging and narrow the brain age gap (BAG).
Article Contributor: Christine Craig, MS, RDN, CDCES is the winner of the 2023 Impact on Diabetes Award. She is a leader in the field of nutrition, technology, and diabetes care. She has served as a preceptor, lecturer, researcher, and is an active association board member. She has worked across health systems; within Diabetes Care Centers, Endocrinology clinics, Primary Care, Telemedicine Rural Health, and Virtual-First Primary Care. Currently she is owner of Nutrition for Daily Living, where it is her mission to increase access to compassionate and evidenced-based nutrition and diabetes care.
- Abigail Dove, Jiao Wang, Huijie Huang, Michelle M. Dunk, Sakura Sakakibara, Marc Guitart-Masip, Goran Papenberg, Weili Xu; Diabetes, Prediabetes, and Brain Aging: The Role of Healthy Lifestyle. Diabetes Care2024; dc240860. https://doi.org/10.2337/dc24-0860
- Sebastian MJ, Khan SK, Pappachan JM, Jeeyavudeen MS. Diabetes and cognitive function: An evidence-based current perspective. World J Diabetes. 2023 Feb 15;14(2):92-109. doi: 10.4239/wjd.v14.i2.92
- Wang K, Zhao S, Lee EK, et al. Risk of Dementia Among Patients With Diabetes in a Multidisciplinary, Primary Care Management Program. JAMA Net Op.2024;7(2):e2355733. doi:10.1001/jamanetworkopen.2023.55733
- Moran C, Lacy ME, Whitmer RA, et al. Glycemic Control Over Multiple Decades and Dementia Risk in People With Type 2 Diabetes. JAMA Neurol.2023;80(6):597–604. doi:10.1001/jamaneurol.2023.0697
- Li Z, Li S, Xiao Y, Zhong T, Yu X, Wang L. Nutritional intervention for diabetes mellitus with Alzheimer’s disease. Front Nutr. 2022 Nov 15;9:1046726. doi: 10.3389/fnut.2022.1046726.
- Akbar Z, Fituri S, Ouagueni A, Alalwani J, Sukik A, Al-Jayyousi GF, Bassil M, Tayyem R. Associations of the MIND Diet with Cardiometabolic Diseases and Their Risk Factors: A Systematic Review. Diabetes Metab Syndr Obes. 2023 Oct 26;16:3353-3371. doi: 10.2147/DMSO.S427412.
Join us Live in Beautiful San Diego for our
Annual DiabetesEd Training Conference
October 9th-11th, 2024

Join Coach Beverly and Team for two and a half days of knowledge-sharing, fun, networking, games with prizes, and “aha” moments in beautiful San Diego on October 9-11, 2024.
You don’t want to miss this one-of-a-kind learning opportunity. Get away from all those daily responsibilities and immerse yourself in a fun and intensive conference with plenty of networking opportunities.
Attendees will leave this conference with new tools and a more complete understanding of the latest advances in diabetes care, from medications to technology to Medical Nutrition Therapy!
Each day, we provide a healthy breakfast, including fresh coffee, to kick off your morning. Our instructors co-teach the content to keep things fresh and lively. Plus, we play DiaBingo to reinforce key content and give away prizes. In addition, we provide plenty of movement breaks led by volunteers from the audience. Did we mention delicious lunches and a conference meeting space just minutes from San Diego Bay?
Friend Discount: 3 or more only $559-$799 (based on registration package) per person. Email us at [email protected] with the name and email of each registrant to get the discount!
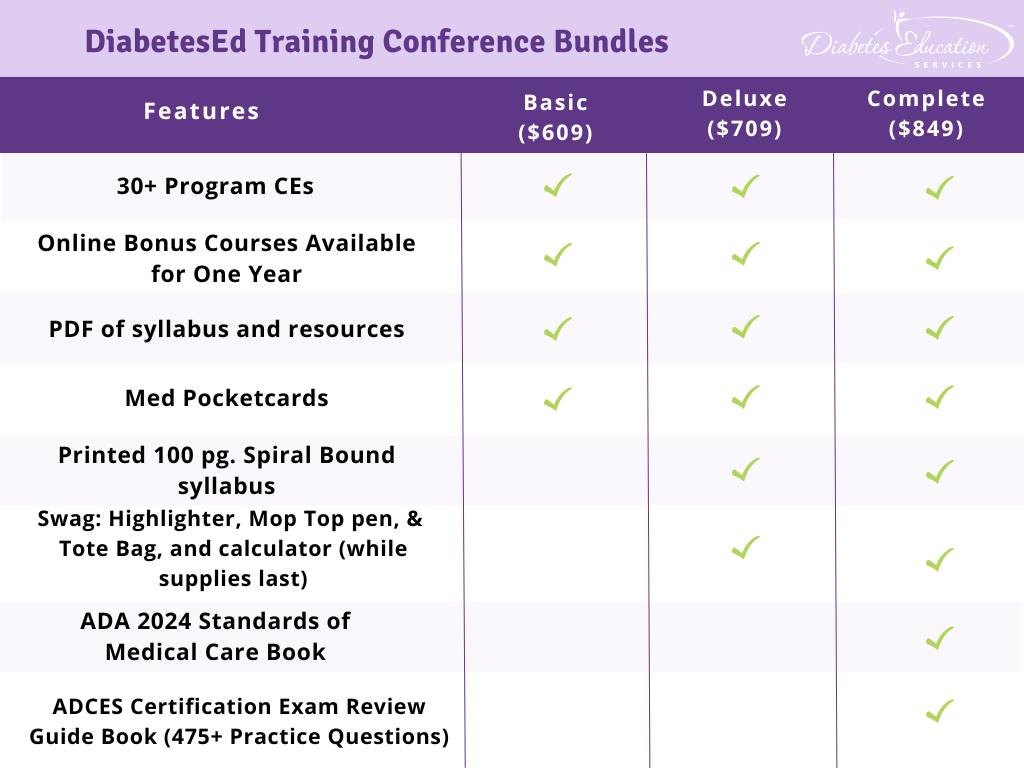
Time: The course is Wednesday through Friday. Join us for breakfast at 7:00 a.m. each day. The class begins at 8:00 a.m. and ends at 5:00 p.m. on Wednesday and Thursday and at 3:00 p.m. on Friday.
- 3 Days: of critical information delivered by passionate speakers in an engaging and fun format!
- 18+ CEs: earned at the Live Seminar (RDs earn 18.75 CEs while Nurses & CA Pharmacists earn 22.75 CEs)
- 10 Bonus Online Courses, Earn 10+ CEs: As a course attendee, you automatically receive a bonus online course bundle of 13 online courses valued at over $179. Coach Beverly carefully chose each of these courses based on student feedback on which content best helped them succeed at the certification exams and in their clinical practice. You will be given instructions after you purchase the course on how to enroll in our Online University and get started!
- Healthy breakfast all days, gourmet lunch both days and refreshments.
- E-version of the syllabus
Sign up for Diabetes Blog Bytes – we post weekly Blog Bytes that are informative and FREE! Every week we post one exam practice Question of the Week and Rationale of the Week. Sign up below!
Accreditation: Diabetes Education Services is an approved provider by the California Board of Registered Nursing, Provider 12640, and our CPEU courses have received Prior Approval* from the Commission of Dietetic Registration (CDR), Provider DI002. Since our CPEU courses received Prior approval* from the CDR, these CPEU courses satisfy the CE requirements for the CDCES /BC-ADM regardless of your profession!
The use of DES products does not guarantee the successful passage of the certification exam. CBDCE and ADCES do not endorse any preparatory or review materials for the CDCES or BC-ADM exams, except for those published by CBDCE & ADCES.









