
For our January 12th Question of the Week, over 58% of respondents chose the best answer!
Before we start though, if you don’t want any spoilers and haven’t tried the question yet, you can answer below: Answer Question
Question:
JR is on metformin 2000mg, empagliflozin 25mg, semaglutide 1.0mg, and 100 units of glargline insulin. A1C is 8.9% and JR weighs 100kg.
What best describes this clinical picture?
Answer Choices:
- Overbasalization
- Non-compliance
- Fear of hypoglycemia
- Clinical inaction
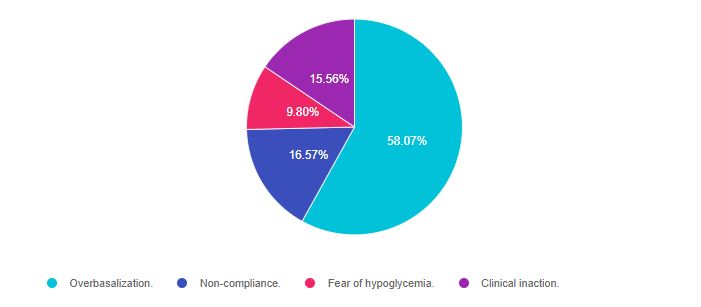
As shown above, the most common choice was option 1, the second most common answer was option 2, then option 4, and finally option 3.
Getting to the Best Answer
If you are thinking about taking the certification exam, the content of this practice test question will set you up for success. It addresses a common ADA Standard 9 and approaches to managing hyperglycemia with type 2 diabetes. This standard is brief with very helpful tables and algorithms. A must-read section for anyone ready to be more actively involved in advocacy and pharmacologic management of diabetes.
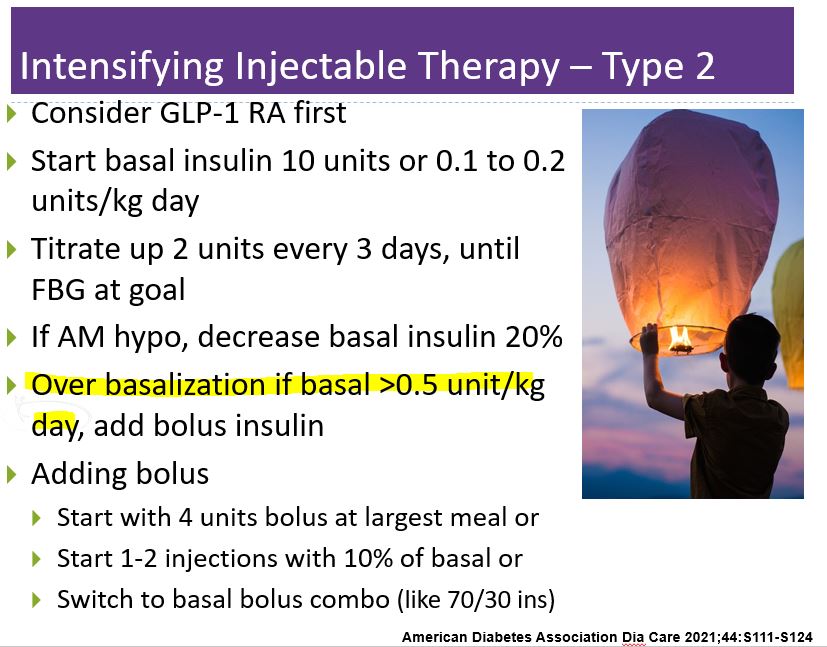
Answer 1 is correct. 58.07% chose this answer. ” Overbasalization.” This is the best answer, because JR is on 3 diabetes medications plus 100 units of basal insulin, and their glucose is still above target. This treatment plan isn’t working. If we look at the ADA Guidelines, (section 9 outlined on a slide below), it states if the basal insulin is more than 0.5 units/kg/day, we need to take further action.
Too much basal
JR weighs 100kg. The max dose of basal insulin based on his body weight should be 50 units (100kg x 0.5 = 50 units). Yet, JR is on 100 units. What are possible solutions?
Getting to basal + bolus
According to ADA Algorithm, we could add 10% of the current basal as bolus insulin, or 10 units one or two meals a day.
Or we could convert it to combo insulin, like 70/30 insulin. To do that conversion, first, decrease total basal insulin by 80% for safety.
100 units x 0.8 = 80 units. Then give 2/3 in the morning and 1/3 before dinner.
80 x 2/3 = about 50 units in the morning and 80 x 1/3 or about 30 units before dinner. If worried about potential hypoglycemia, the dose could be decreased even further. The main goal is to get glucose to the goal.
Answer 2 is incorrect. 16.57% of you chose this answer. “Non-compliance.” According to the information in the case study, JR is taking all of the medications as directed. The issue is that the medication plan is not effective. And, more than that, the term “non-compliance” has been replaced with focusing on the person’s strengths (strength based approach) and what the actions the individual IS taking.
Answer 3 is incorrect, 9.80% of you chose this answer “Fear of hypoglycemia.” The answer is tempting. Since JR is on 100 units of basal insulin, hypoglycemia seems like a looming possibility. However, we see that the A1c is 8.9% and JR doesn’t mention hypoglycemia. It is very unlikely that low blood sugar is an issue.
Answer 4 is incorrect, 15.56% of you chose this answer. “Clinical inaction.” It is true that more action is required, and the term we use for this is lack of movement to improve glucose levels is called “Clinical inertia”. However, in answering the question, “what best describes this clinical picture”, “overbasalization” is the standout answer.
We hope you appreciate this week’s rationale! Thank you so much for taking the time to answer our Question of the Week and participate in this fun learning activity!








