
For last week’s practice question, we quizzed test takers on abdominal lumps and insulin injections. Only 46% of respondents chose the best answer, which indicates that there was some confusion. We want to clarify and share this important information, so you can pass it on to people living with diabetes and your colleagues, plus prepare for exam success!
Before we start though, if you don’t want any spoilers and haven’t tried the question yet, you can answer it below: Answer Question
Question:
JL is 67 years old, with a BMI of 23 and A1C of 7.6% and injects insulin 4 times a day to manage their type 1 diabetes. On visual inspection, you notice that there are many areas of lipohypertrophy on JL’s abdominal region.
Which of the following interventions would be the best recommendation?
Answer Choices:
- Switch to 50/50 insulin twice daily.
- Stop bolus insulin and switch to a GLP-1 RA.
- Switch bolus injections to inhaled insulin.
- Use a higher gauge needles to enhance absorption.
Getting to the Best Answer
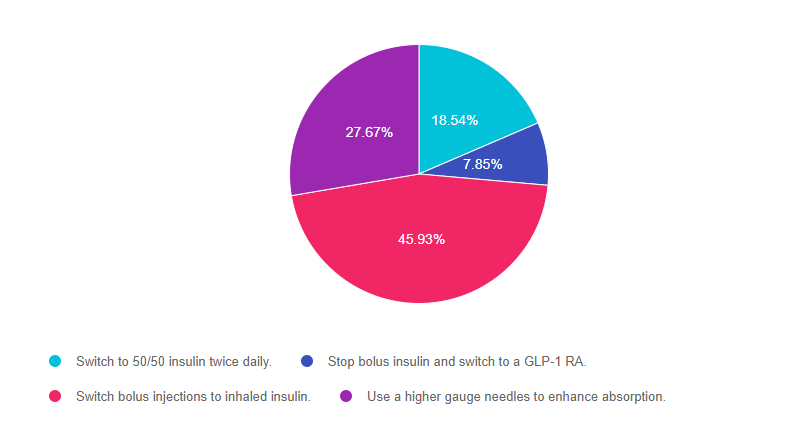
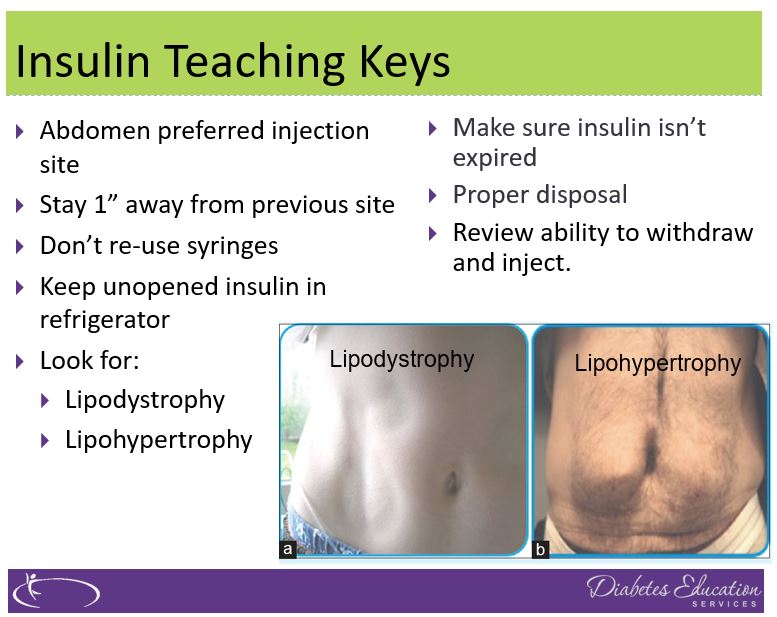
Answer 1 is incorrect. 18.54% chose this answer, “Switch to 50/50 insulin twice daily.” This is not the best answer since it doesn’t address the core issue of injection site overuse and fat accumulation. Switching to 50/50 insulin may even lead to worsening blood sugars since it is a premixed basal bolus insulin that would be difficult to fine tune for people with type 1 diabetes. (See photo of lipohypertrophy below)
Answer 2 is incorrect. 7.85% of you chose this answer, “Stop bolus insulin and switch to a GLP-1 RA.” This is not the best answer since GLP-1 RA’s are not FDA approved to treat people with type 1 diabetes*. If a person with type 1 diabetes stopped their bolus insulin, they would become very insulin deprived and likely experience severe blood glucose elevations and hyperglycemic crisis. Plus, this answer doesn’t address the core issue of injection site overuse and fat accumulation. *Footnote: some people with type 1 are prescribed a GLP-1 RA (off label) in ADDITION to basal bolus insulin to lower glucose levels and help with weight management. (See photo of lipohypertrophy below)
Answer 3 is correct. 45.93% of respondents chose this answer, “Switch bolus injections to inhaled insulin.” YES, GREAT JOB. Lipohypertrophy, a lump of fat accumulation due to frequent injections, has been shown to affect ?50% of people injecting insulin and results from lack of injection site rotation and needle. Injecting into these “lumps” reduces insulin absorption and action, raises postprandial glucose, and greatly increases insulin uptake variability. Despite this, inspection of injection sites is not routinely performed by health care professionals or people with diabetes, which reveals the “unexplained” nature of many blood glucose fluctuations. (Excerpted from this Article on Insulin Injection Technique- Clinical Diabetes, 2019).
To avoid lipohypertrophy, we can transition people to boluses of inhaled insulin to cover for food and hyperglycemia and still provide one basal injection a day, using sites free of fatty lumps. This reduction of the injection frequency allows time for tissue healing and reduces creation of new lipohypertrophy sites. Download our FREE Insulin PocketCards here.
If a person decides to stay on injections, encourage them to systematically space them at least 1 cm (about the width of an adult finger) from each other; this helps to avoid repeat tissue trauma. One approach involves dividing sites into quadrants (or halves when using the buttocks or thighs), using one quadrant per week and moving from quadrant to quadrant in a consistent direction (e.g., clockwise). Encourage people to rotate injections between sites, as well as within a site. Use needles once and toss, since excessive reuse of needles can traumatize the skin and underlying structures. (See photo of lipohypertrophy below)
Finally, Answer 4 is incorrect. 27.67% chose this answer, “Use a higher gauge needles to enhance absorption.” This is not the best answer since it doesn’t address the core issue of injection site overuse and fat accumulation. Switching to a higher gauge needle just means the barrel of the needle is thinner and hurts less when passing through the skin. Improper injection site rotation and needle reuse are the most common factors associated with lipohypertrophy. (See photo of lipohypertrophy below)
Read more great info here, The Injection Technique Factor: What You Don’t Know or Teach Can Make a Difference – Article from Clinical Diabetes, 2019. You are also invited to join our Virtual Conference where we tackle this topic and many more factors that affect diabetes self-care.
Sign up for Diabetes Blog Bytes – we post one daily Blog Byte from Monday to Friday. And of course, Tuesday is our Question of the Week. It’s Informative and FREE! Sign up below!
The use of DES products does not guarantee the successful passage of the CDCES exam. CBDCE does not endorse any preparatory or review materials for the CDCES exam, except for those published by CBDCE.









