
For last week’s practice question, we quizzed test takers on glucose monitoring in the inpatient setting. 60% of respondents chose the best answer. We want to share this important information, so you can pass it on to people living with diabetes and your colleagues, plus prepare for exam success!
Before we start though, if you don’t want any spoilers and haven’t tried the question yet, you can answer it below: Answer Question
Question: JL is a new nursing graduate and asks you questions about glucose monitoring in the inpatient setting. Which of the following statements is most accurate regarding providing diabetes care in the hospital setting?
Answer Choices:
- If a patient is experiencing morning hypoglycemia, reduce basal insulin.
- Nursing staff can use the patient’s CGM glucose results to determine insulin dose.
- Any patient admitted with a glucose of 140 mg/dl or greater, confirmed on two different occasions, needs to be started on insulin.
- Hospital point-of-care glucose meters are mostly as accurate as lab glucose results.
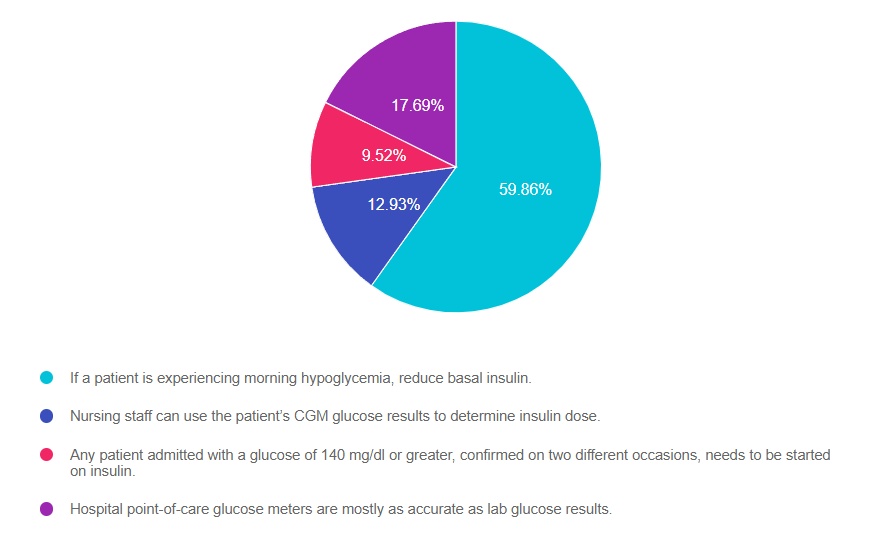
As shown above, the most common choice was option 1, the second most common answer was option 4, then option 2, and finally 3.
Getting to the Best Answer
Answer 1 is correct. 59.86% chose this answer, “If a patient is experiencing morning hypoglycemia, reduce basal insulin.” YES, GREAT JOB! During hospitalization, keeping glucose levels on target improves outcomes and decreases the length of stay. This includes preventing hypoglycemia, which can be life-threatening. The most common cause of morning hypoglycemia is basal insulin. Treating hypoglycemia rapidly with carbs and rechecking to make blood sugar is increasing is critical. However, to prevent future hypoglycemic events, determining the cause of the low blood sugar and taking corrective action is just as important. Reducing basal insulin by 20% or more when morning blood sugars are less than 100 mg/dL in the hospital setting makes a big difference in protecting against hypoglycemia.
Answer 2 is incorrect. 12.93% of you chose this answer, “Nursing staff can use the patient’s CGM glucose results to determine insulin dose.” This is a juicy answer, however, the FDA has not approved the dosing of insulin based on CGM results in the hospital setting. Inpatients with adequate cognition are allowed to use their CGM to monitor their blood sugar and keep an eye on trends based on the hospital’s policy. However, insulin dosing is based on the hospital-approved point-of-care glucose meter results.
Answer 3 is incorrect. 9.52% of respondents chose this answer, “Any patient admitted with a glucose of 140 mg/dl or greater, confirmed on two different occasions, needs to be started on insulin.” If a person is admitted with a glucose of 140 or greater, this would certainly catch our attention and require ongoing monitoring. They may have undiagnosed prediabetes or diabetes (depending on if the glucose was fasting or random). However, this glucose level of 140 does not meet the criteria to start insulin. According to the ADA Standards, insulin therapy is initiated when the admitting glucose is 180 or greater.
Finally, Answer 4 is incorrect. 17.69% chose this answer, “Hospital point-of-care glucose meters are mostly as accurate as lab glucose results.” This is another juicy answer. The lab glucose is the most accurate. Approved hospital glucose meters can read 15% higher or lower than the actual lab glucose. At home glucose meters, can be up read up to 20% higher or lower than lab glucose and still be within FDA approval parameters. For more info, see our blog, How Accurate are Glucose Meters?
Want to learn more about this question? Join us for our webinar
Hospitals & Hyperglycemia Standards | Level 2 | $29 for 1.5 CEs
Recorded & Ready to Watch!
Research clearly demonstrates the importance of glucose control during hospitalization to improve outcomes not only in the inpatient setting but after discharge. This course reviews the evidence that supports inpatient glucose control and outlines practical strategies to achieve targets in the inpatient setting. We incorporate the latest ADA Standards and provide links to resources and inpatient management templates.
Objectives:
- The impact of hyperglycemia in the hospital setting
- The importance of inpatient glucose control
- Three strategies to get glucose to the goal in the hospital setting
The use of DES products does not guarantee the successful passage of the CDCES exam. CBDCE does not endorse any preparatory or review materials for the CDCES exam, except for those published by CBDCE.









