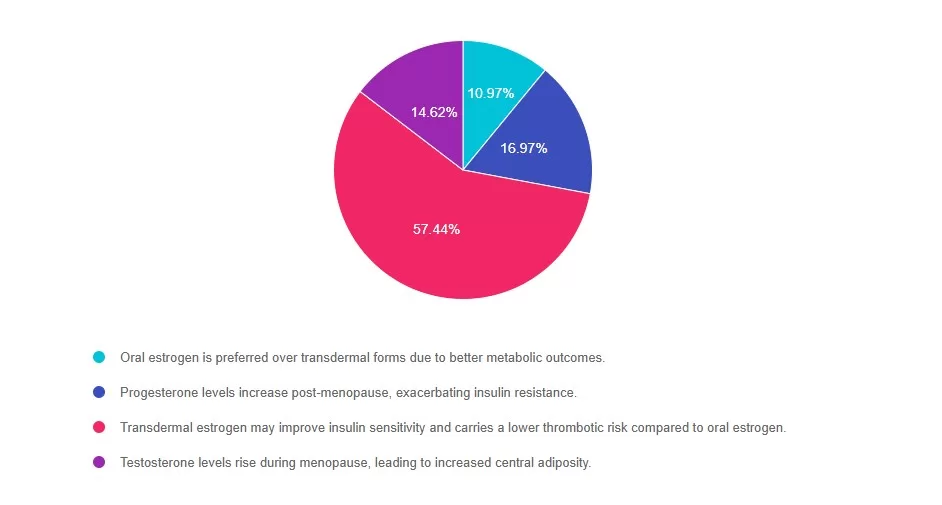
For last week’s practice question, our special guest expert Jill Schramm, DNP, FNP-C, BC-ADM, CDCES quizzed us on Current Hormone Therapy Guidance for people with T2D. 57% of respondents chose the best answer. We want to clarify and share this important information, so you can pass it on to people living with diabetes and your colleagues, plus prepare for exam success!
Before we start though, if you don’t want any spoilers and haven’t tried the question yet, you can answer it below: Answer Question

Question: Which statement accurately reflects current guidelines on hormone therapy (HT) in postmenopausal women with type 2 diabetes?
Answer Choices:
- Oral estrogen is preferred over transdermal forms due to better metabolic outcomes.
- Progesterone levels increase post-menopause, exacerbating insulin resistance.
- Transdermal estrogen may improve insulin sensitivity and carries a lower thrombotic risk compared to oral
estrogen. - Testosterone levels rise during menopause, leading to increased central adiposity.
Getting to the Best Answer
Answer 1 is incorrect. 10% chose this answer, “Oral estrogen is preferred over transdermal forms due to better metabolic outcomes.” Oral estrogen undergoes first-pass hepatic metabolism, which can negatively influence clotting factors. Transdermal estrogen bypasses the liver and is generally favored in women with cardiometabolic risk, such as those with type 2 diabetes.
Reference: The Menopause Society, 2022; American Diabetes Association (ADA) Standards of Care in Diabetes; 2025.
Answer 2 is incorrect. 16% of you chose this answer, “Progesterone levels increase post-menopause, exacerbating insulin resistance.” Progesterone levels actually decrease after menopause due to ovarian senescence. There is no physiological increase in progesterone levels that would worsen insulin resistance during the postmenopausal years.
Reference: The Menopause Society, 2022.
Answer 3 is correct. About 57% of respondents chose this, “Transdermal estrogen may improve insulin sensitivity and carries a lower thrombotic risk compared to oral estrogen.” GREAT JOB. This is the best answer and aligns with current guidelines. Transdermal estrogen has been shown to improve insulin sensitivity and does not increase hepatic production of clotting factors the way oral estrogen does. As a result, it is associated with a lower risk of venous thromboembolism, making it a safer option for postmenopausal women with metabolic concerns such as type 2 diabetes.
Reference: The Menopause Society (formerly NAMS), 2022 Position Statement
Finally, Answer 4 is incorrect. 14% chose this answer, “Testosterone levels rise during menopause, leading to increased central adiposity.“Testosterone levels generally decline with age and menopause, although the ratio of testosterone to estrogen may shift due to declining estrogen. While visceral adiposity does tend to increase in menopause, it is more directly related to estrogen deficiency rather than a surge in testosterone.
Reference: The Menopause Society, 2022.
Thanks to Jill Schramm, DNP, FNP-C, BC-ADM, CDCES for her providing us with these terrific insights into menopause. Join her presentation on August 27th to learn more! See info below. Thank you so much for taking the time to answer our Question of the Week and participate in this fun learning activity!
Want to learn more about this question?
Join us live on August 27th for our
Level 5: Hot Flashes & Hyperglycemia: What Clinicians Need to Know
Join us live on August 27th, 2025, at 11:30 am PST to watch our brand new webinar, Hot Flashes & Hyperglycemia: What Clinicians Need to Know by Dr. Jill Schramm, DNP, FNP-C, BC-ADM, CDCES
The intersection of menopause and diabetes is often underrecognized in clinical care, yet people with diabetes in menopausal transition face unique metabolic, hormonal, and lifestyle changes that can significantly impact glycemic control. This session explores the physiological shifts of menopause, the implications for insulin resistance, and evidence-based strategies for individualized care. Attendees will leave with practical guidance on hormone therapy, lifestyle management, and education tools to improve outcomes for people with diabetes navigating both diabetes and the menopausal transition.
All hours earned count toward your CDCES Accreditation Information
Sign up for Diabetes Blog Bytes – we post weekly Blog Bytes that are informative and FREE! Every week we post one exam practice Question of the Week and Rationale of the Week. Sign up below!
The use of DES products does not guarantee the successful passage of the certification exam. CBDCE and ADCES do not endorse any preparatory or review materials for the CDCES or BC-ADM exams, except for those published by CBDCE & ADCES.








