
For our February 9th Question of the Week, over 50% of respondents chose the best answer!
Before we start though, if you don’t want any spoilers and haven’t tried the question yet, you can answer below: Answer Question
Question: RT is a 49-year-old with type 1 diabetes, admitted to a local hospital to treat Diabetes Ketoacidosis (DKA). RT is on an insulin drip, fluids and potassium replacement therapy and is getting hungry. The IV insulin is running at 2 units an hour and the RTs usual insulin dose at home is 12 units glargine at bedtime and 3-4 units of lispro before meals.
Before stopping the IV insulin, what is the most important action?
Answer Choices:
- Maintenance of glucose less than 200 for at least 4 hours
- Give 3 units of bolus insulin via IV and at least 6 units of glargine
- Evaluate labs to make sure that RT is ketone negative
- Determine if potassium replacement is still needed
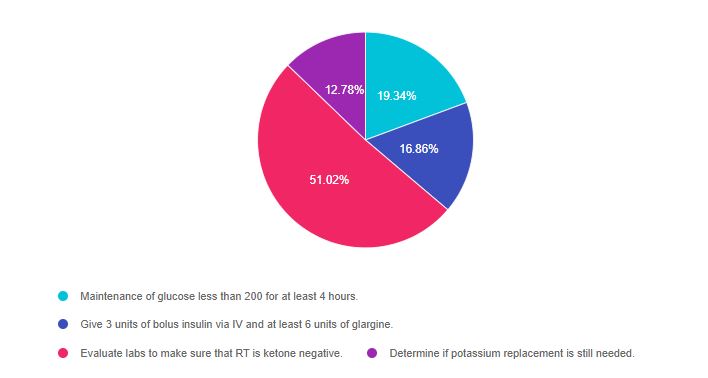
As shown above, the most common choice was option 3, the second most common answer was option 1, then option 2, and finally option 4.
Getting to the Best Answer
If you are thinking about taking the certification exam, the content of this practice test question will set you up for success. There are questions on in-hospital care of diabetes and treating hyperglycemic crises.
DKA Quick Review
Before we answer this question, we thought we would provide a quick summary of the basics of DKA.

Diabetes Ketoacidosis occurs because there is not enough insulin to use glucose for fuel. The body turns to fat for fuel and this causes a build-up of ketone bodies in the blood and urine. Since ketone bodies are acids, they lower the pH of the blood potentially causing a life-threatening acidosis.
Insulin therapy is required to stop acidosis.
Additionally, even if the glucose is under 200, the person can still be “under insulinized” and ketotic. That is why the insulin drip can only be stopped when the person is ketone negative and no longer burning fat for fuel. One sign that they are moving out of ketosis is that they become hungry. Ketone bodies are very irritating to the GI system and cause nausea and sometimes significant abdominal pain.
If the insulin drip is stopped too early, when the person is still positive for ketones, they are at risk of going back into DKA.
Potassium – When people are experiencing ketosis they are insulin deprived. This lack of insulin allows potassium to leave the cells and enter the bloodstream. Much of this excessive extracellular potassium is then renally excreted. When insulin therapy is started, this pushes potassium back into the cells and can cause a dangerous drop in serum potassium levels. For this reason, most people with DKA will need potassium replacement.
It is critically important to evaluate potassium before starting insulin therapy in someone with DKA. If the potassium is less than 3.3 mEq/L, the guidelines recommend providing potassium replacement therapy first, then starting insulin when potassium levels are stable.
See our blog Treating DKA with SubQ Insulin here for more details.
Answers & Rationale
Answer 1 is incorrect, 19.34% chose this answer. “Maintenance of glucose less than 200 for at least 4 hours”. Even if the glucose is under 200, the person can still be “under insulinized” and ketotic. That is why the insulin drip can only be stopped when the person is ketone negative and no longer burning fat for fuel.
Answer 2 is incorrect 16.86% of you chose this answer. “Give 3 units of bolus insulin via IV and at least 6 units of glargine”. It is true that subq insulin needs to be administered about 2 hours before stopping the IV insulin since the half-life of IV insulin is only minutes. But, most important is that we need to make sure their acidosis is resolved. If the insulin drip is stopped too early, when the person is still positive for ketones, they are at risk of going back into DKA.
Answer 3 is correct 51.02% of you chose this answer “Evaluate labs to make sure that RT is ketone negative” YES, this is the BEST Answer. If they are ketone negative and blood sugars are under 200, we can inject subq basal insulin about 2 hours before stopping the drip to stabilize glucose levels. Then we provide subq insulin replacement therapy based on prior history and body weight.
Answer 4 is incorrect 12.78% of you chose this answer. “Determine if potassium replacement is still needed” Of course, we are keeping a close eye on potassium, but an IV is not required to administer potassium since it can be given orally. In addition, the most important factor in determining if the IV insulin can be stopped is the state of ketosis.
We hope you appreciate this week’s rationale! Thank you so much for taking the time to answer our Question of the Week and participate in this fun learning activity!
Hyperglycemic Crises, DKA & HHS | 1.0 CEs
Join Coach Beverly to learn more about the causes and treatment of hyperglycemic crisis.

This course is included in: Level 2 – Standards of Care. Purchase this course individually for $19 or the entire bundle and save 70%.
This 60-minute course discusses common causes of hyperglycemia crises. Topics include hyperglycemia secondary to medications and insulin deprivation. The difference and similarities between Diabetes Ketoacidosis and Hyperosmolar Hyperglycemic Syndrome are also covered. Treatment strategies for all situations are included.
Topics include:
- Common causes of hyperglycemic crises.
- The difference and similarities between DKA and HHS and treatment strategies
- Causes and treatment of hyperglycemic crises.
Sign up for Diabetes Blog Bytes – we post one daily Blog Byte from Monday to Friday. And of course, Tuesday is our Question of the Week. It’s Informative and FREE! Sign up below!
[yikes-mailchimp form=”1″]
Accreditation: Diabetes Education Services is an approved provider by the California Board of Registered Nursing, Provider 12640, and Commission on Dietetic Registration (CDR), Provider DI002. Since these programs are approved by the CDR it satisfies the CE requirements for the CDCES regardless of your profession.*
The use of DES products does not guarantee the successful passage of the CDCES exam. CBDCE does not endorse any preparatory or review materials for the CDCES exam, except for those published by CBDCE.









