For last week’s practice question, we quizzed test takers on if insulin is safe for older adults. 78% of respondents chose the best answer. We want to share this important information, so you can pass it on to people living with diabetes and your colleagues, plus prepare for exam success!
Before we start though, if you don’t want any spoilers and haven’t tried the question yet, you can answer it below: Answer Question
Question: For older adults with diabetes using insulin therapy, which of the following is the most accurate statement?
Answer Choices:
- Due to cognitive decline, continuous glucose monitoring is not recommended for older adults.
- Older adults are at greater risk of hypoglycemia than younger adults.
- Divide basal insulin into two separate doses to enhance absorption.
- Give insulin after meals to prevent hypoglycemia.
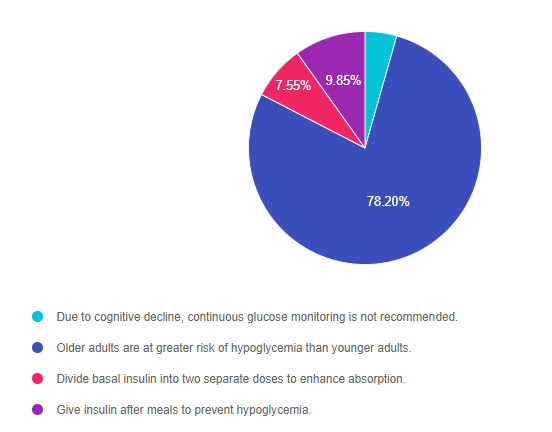
As shown above, the most common choice was option 2, the second most common answer was option 4, then option 3, and finally 1.
Getting to the Best Answer
Answer 1 is incorrect. 4.40% chose this answer, “Due to cognitive decline, continuous glucose monitoring is not recommended for older adults.” Many older adults on intensive insulin therapy with a history of hypoglycemia can benefit from CGM technology to prevent low blood sugars and fine tune carb intake and insulin dosing. Each older adult needs a individualized assessment to determine if a CGM is right for them. The rate of cognitive decline is complex and is a result of genetics, other chronic conditions and overall health combined with aging.
Answer 2 is correct. 78.20% of you chose this answer, “Older adults are at greater risk of hypoglycemia than younger adults. GREAT JOB, almost 80% of you chose this best answer. As people with diabetes age, they are at higher risk for low blood sugars for many reasons, especially if they are taking insulin or a secretagogue. Older individuals may have diminished renal function, which increases the duration of the action of insulin and secretagogues. Some can experience lower calorie intake due to decreasing appetite, trouble chewing, lack of resources, forgetfulness or depression and feelings of isolation. Others may have difficulty administering their insulin or medications accurately or may forget to eat after injections. For this reason, the ADA Standards recommends that older adults are assessed for hypoglycemia risk at each visit coupled with problem solving as needed.
Answer 3 is incorrect. 7.55% of respondents chose this answer, “Divide basal insulin into two separate doses to enhance absorption.” This is a juicy answer. For older adults at risk for hypoglycemia, the ADA does recommend scheduling the basal insulin for the morning instead of evening.
Finally, Answer 4 is incorrect. 9.85% chose this answer, “Give insulin after meals to prevent hypoglycemia.” Another juicy answer. This answer implies that all older people should take their insulin after meals. Some individuals might benefit from post-meal insulin, especially if they are not sure how much they are going to eat and they have a history of hypoglycemia. However, insulin works best when given before the meal so it peaks at the same time the post meal glucose is peaking.
Studying for the CDCES Exam?
Enroll in CDCES Online Prep Bundle + 5th Ed ADCES Review Guide Book | 47 CEs
This bundle includes our CDCES Online Prep Bundle plus the ADCES Review Guide.
The online bundle includes Level 1, Level 2, and Level 3 (Boot Camp), plus two bonus courses. The ADCES Review Guide offers over 480+ practice questions and is a fantastic independent study tool and comprehensive resource for the Diabetes Care and Education Specialist Exam.
What is a Certified Diabetes Care and Education Specialist?
Read More: What is a CDCES? First awarded in 1986, as Certified Diabetes Educator (CDE) credential and in 2020 with a new name: Certified Diabetes Care and Education Specialist (CDCES) to more accurately reflect the specialty. CDCES has become a standard of excellence for the delivery of quality diabetes education. Those who hold this certification are known to possess comprehensive knowledge of and experience in diabetes prevention, management, and prediabetes. “Becoming a Certified Diabetes Care and Education Specialist (CDCES) is one of the best professional and personal decisions I have ever made.” – Coach Beverly Thomassian, RN, MPH, CDCES, BC-ADM
Why become a CDCES?
Three Reasons from Coach Beverly
Read More: 3 Reasons to Become a CDCES “The best part of becoming a CDCES is working with my colleagues and people living with diabetes. As diabetes educators, we hear compelling and beautiful life stories. I am astounded by the barriers they face and inspired by their adaptability, problem-solving skills, and resilience.” Reason 1: CDCES is a widely recognized certification by employers and health care professionals throughout the U.S. This credential demonstrates a specialized and in-depth knowledge in the prevention and treatment of individuals living with pre-diabetes and diabetes. Reason 2: Currently, 10% of people in the U.S. have diabetes and another 35% have pre-diabetes which means 45% of Americans are running around with elevated blood glucose levels. Given this epidemic, there will be plenty of future job opportunities. Reason 3: Having my CDCES along with my nursing degree, has opened many doors of opportunity; from working as an inpatient Diabetes Nurse Specialist in a hospital to working as a Manager of Diabetes Education in the outpatient setting to starting my own consulting company.
Sign up for Diabetes Blog Bytes – we post one daily Blog Byte from Monday to Friday. And of course, Tuesday is our Question of the Week. It’s Informative and FREE! Sign up below!
The use of DES products does not guarantee the successful passage of the CDCES exam. CBDCE does not endorse any preparatory or review materials for the CDCES exam, except for those published by CBDCE.