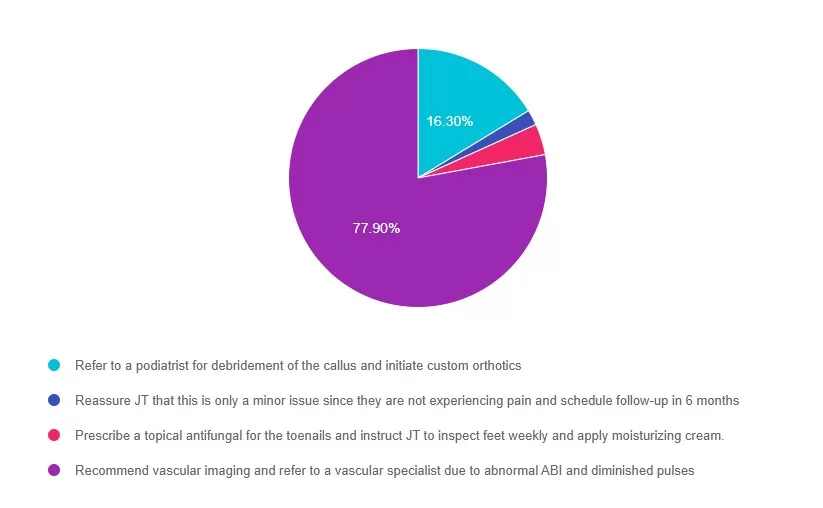
For last week’s practice question, we quizzed participants on Lower Extremity Recommendation for JT? . 77% of respondents chose the best answer. We want to clarify and share this important information, so you can pass it on to people living with diabetes and your colleagues, plus prepare for exam success!
Before we start though, if you don’t want any spoilers and haven’t tried the question yet, you can answer it below: Answer Question

Question:
JT is a 58-year-old with type 2 diabetes presents for a routine exam. Has a 20-year history of diabetes, hypertension, and peripheral neuropathy. Reports no foot pain, but partner notes they have been walking with a slight limp. On exam, you note dry skin, thickened toenails, a callus on the plantar aspect of the first metatarsal head, and diminished monofilament sensation at multiple sites on both feet. Pedal pulses are diminished bilaterally, and ABI (Ankle-Brachial Index) is 0.6 on the right and 0.7 on the left.
Which of the following is the most appropriate next step in managing this JT’s foot care?
Answer Choices:
- Refer to a podiatrist for debridement of the callus and initiate custom orthotics.
- Reassure JT that this is only a minor issue since they are not experiencing pain and schedule follow-up in 6 months.
- Prescribe a topical antifungal for the toenails and instruct JT to inspect feet weekly and apply moisturizing cream.
- Recommend vascular imaging and refer to a vascular specialist due to abnormal ABI and diminished pulses.
Getting to the Best Answer
Answer 1 is incorrect. 16% chose this answer, “Refer to a podiatrist for debridement of the callus and initiate custom orthotics.” While podiatry referral is important, vascular compromise must be evaluated first. Debridement in a patient with peripheral arterial disease (PAD) could lead to poor healing or ulceration.
Answer 2 is incorrect. 1% of you chose this answer, “Reassure JT that this is only a minor issue since they are not experiencing pain and schedule follow-up in 6 months.” Absence of pain does not exclude serious pathology, especially in individuals with neuropathy.
Answer 3 is incorrect. About 3% of respondents chose this, “Prescribe a topical antifungal for the toenails and instruct JT to inspect feet weekly and apply moisturizing cream.” This addresses a minor issue (onychomycosis), but ignores signs of ischemia and neuropathy.
Finally, Answer 4 is correct. 77% chose this answer, “Recommend vascular imaging and refer to a vascular specialist due to abnormal ABI and diminished pulses.” ABI values <0.9 indicate PAD; values <0.5 are considered severe. Given the ABI of 0.6 and 0.7, along with diminished pulses and gait change, vascular referral is necessary to assess perfusion and prevent future ulceration or amputation.
We hope you appreciate this week’s rationale! Thank you so much for taking the time to answer our Question of the Week and participate in this fun learning activity!
Want to learn more about this question?
Join us live on August 12th @ 11:30am PST for Level 4 | 3 Steps to DeFeet Amputation

Coach Beverly will walk participants through the 3-Step Process to Save Feet; Assess, Screen, & Report. She will provide simple and clear instructions on how to assess and inspect feet, along with risk assessment & action steps. We will share free teaching tools, strategies, & documentation forms adapted from the Lower Extremity Prevention Program (LEAP) that you can immediately implement in your practice setting. This course is free to attend without earning CEs, or you can choose the paid option if you wish to receive CE credits.
All hours earned count toward your CDCES Accreditation Information
Sign up for Diabetes Blog Bytes – we post weekly Blog Bytes that are informative and FREE! Every week we post one exam practice Question of the Week and Rationale of the Week. Sign up below!
The use of DES products does not guarantee the successful passage of the certification exam. CBDCE and ADCES do not endorse any preparatory or review materials for the CDCES or BC-ADM exams, except for those published by CBDCE & ADCES.