For last week’s practice question, we quizzed test takers on pregnancy and diabetes. 63% of respondents chose the best answer. We want to share this important information, so you can pass it on to people living with diabetes and your colleagues, plus prepare for exam success!
Before we start though, if you don’t want any spoilers and haven’t tried the question yet, you can answer it below: Answer Question
Question: AR says they just found out they are pregnant. AR has type 2 diabetes and polycystic ovary syndrome and takes metformin 1000mg BID, semaglutide (Ozempic) 1.0mg weekly, and 30 units glargine insulin for diabetes management. Her most recent A1C was 8.2%. What is the most important action to take?
Answer Choices:
- Add bolus insulin to get A1C less than 6.5%.
- Increase the semaglutide (Ozempic) to 2.0mg weekly.
- Add a SGLT-2 Inhibitor to get glucose to target.
- Instruct AR to stop the semaglutide (Ozempic).
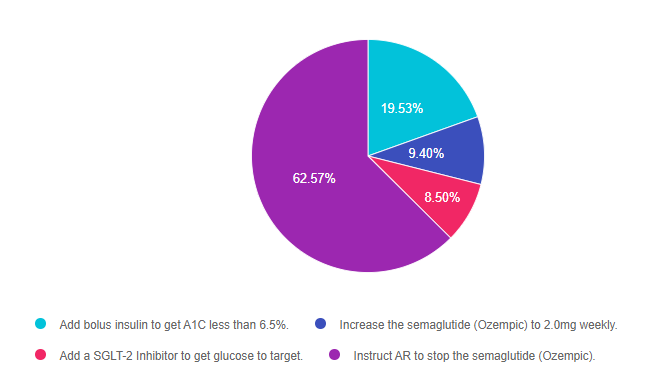
As shown above, the most common choice was option 4, the second most common answer was option 1, then option 2, and finally 3.
Getting to the Best Answer
Answer 1 is incorrect. 19.53% chose this answer, “Add bolus insulin to get A1C less than 6.5%.” This answer is accurate, but it is not the best answer. The A1C goal during pregnancy is less than 6.5% and in this case, AR will need to manage their diabetes using basal bolus insulin therapy. However, since semaglutide is not approved for pregnancy, the most important action is to stop the administration of this GLP-1 RA.
Answer 2 is incorrect. 9.40% of you chose this answer, “Increase the semaglutide (Ozempic) to 2.0mg weekly.” AR’s blood glucose levels are above the A1C pregnancy target of 6.5%, which means insulin intensification is needed. Insulin is safe during pregnancy. However, since semaglutide is not approved for pregnancy, the most important action is to stop the administration of this GLP-1 RA.
Answer 3 is incorrect. 8.50% of respondents chose this answer, “Add a SGLT-2 Inhibitor to get glucose to target.” AR’s blood glucose levels are above the A1C pregnancy target of 6.5%, which means insulin intensification is needed. Insulin is safe during pregnancy. However, SGLT-2s are not approved for pregnancy and the GLP-1 RA, semaglutide would also need to be discontinued.
Finally, Answer 4 is correct. 62.57% chose this answer, “Instruct AR to stop the semaglutide (Ozempic).” YES, GREAT JOB! AR’s blood glucose levels are above the A1C pregnancy target of 6.5%, which means insulin intensification is needed. Basal bolus insulin therapy is safe during pregnancy. However, since semaglutide is not approved for pregnancy, the most important action is to stop the administration of this GLP-1 RA. Metformin can be continued through the first trimester and the insulin would need to be intensified to get A1C to target.
Want to learn more about this question? Join us for our webinar
Pregnancy & Diabetes Standards | Level 2 | $29 for 1.5 CEs
Recorded & Ready to Watch!

Pregnancy with diabetes is confronted with a variety of issues that require special attention, education, and understanding. This course reviews those special needs while focusing on Gestational Diabetes and Pre-Existing Diabetes. Included are the most recent diagnostic criteria, management goals, and prevention of complications during pregnancy. A helpful review for the CDCES Exam and for those who want more information on people who are pregnant and live with Diabetes.
Objectives:
- Three issues that affect pregnancy with diabetes
- The unique attributes of pre-existing diabetes in pregnancy and gestational diabetes
- Diagnostic criteria and management goals for gestational diabetes
- Potential short term and long term complications of fetal exposure to hypoglycemia
- Prevention measures to keep parent and baby healthy
The use of DES products does not guarantee the successful passage of the CDCES exam. CBDCE does not endorse any preparatory or review materials for the CDCES exam, except for those published by CBDCE.