JR is 64 years old, in hospital with type 2 diabetes and COVID. JR normally manages their diabetes with metformin, but during this inpatient stay, JR is on prednisone therapy which has spiked sugar levels into the 250 mg/dl to 350 range. JR is receiving bolus insulin sliding scale with meals and bedtime glargine, but blood sugars are persistently elevated. To improve outcomes for JR, it is important to keep blood glucose levels less than 180 mg/dl, but what should we recommend to get glucose to goal?
What are some strategies to get blood sugar to target while on steroids?
There is no consensus on the best approach to manage this situation. Up until this point in history, steroid-induced hyperglycemia was mostly found in people with diabetes in COPD, those undergoing chemotherapy or in post-transplant situations.

Oral Meds plus an Old Friend
With the COVID pandemic, many people with diabetes in hospitals and at home, are on steroids. Health care professionals are trying to figure out how to lower glucose levels.
For people with type 2 diabetes and COVID, the latest research indicates that sitagliptin (Januvia) not only helps maintain blood glucose but also decreases the inflammatory response associated with COVID infections. If not contraindicated, sitagliptin can be used in conjunction with insulin, to treat the extreme insulin resistance and hyperglycemia caused by steroid therapy.
To treat steroid induced hyperglycemia, we are going to call on our old insulin friend, NPH. Neutral Protamine Hagedorn (NPH) is an intermediate acting basal insulin. NPH insulin is made by mixing regular insulin and protamine in exact proportions with zinc and phenol such that a neutral-pH is maintained and crystals form.
NPH insulin’s peak action time matches steroid’s action time
NPH insulin is cloudy and has an onset of 1–4 hours. Its peak is 6–10 hours and its duration is about 10–16 hours.
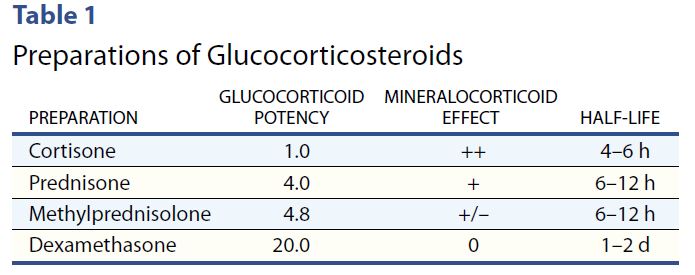
Steroids have their highest potency at 4-12 hours, with the exception of the very potent dexamethasone, which has a half life of 1-2 days.
However, with all steroids, including dexamethasone, people will experience elevated glucose values after breakfast, lunch, dinner, and at bedtime but will have a significant drop toward normal glucose overnight.
Therefore, hyperglycemia is greatest 1–2 hours after a meal, with persistent elevation until the following meal, followed by a return to normal overnight.

NPH Insulin Dosing Strategies
There are several articles (see below) that recommend a variety of NPH dosing strategies. Generally, insulin dosing is based on a combination of steroid dose and body weight. For those on lower dose steroid (ie less than 40 mg prednisone daily) a starting NPH insulin dose of 0.1 – 0.2 units per kg is reasonable. If JR weighs 100 kg, that means 10 to 20 units of NPH daily.
If JR is on a higher steroid dose, or blood sugars are extremely elevated, JR may need 0.3 units/kg or 30 units of NPH daily. Of course, we also need to keep nutritional status in mind as we determine best dose. People who are not eating or NPO, will require less insulin, even in the presence of steroids.
The timing of NPH administration matches the timing of the steroid therapy.
In addition, coverage for carbohydrates at meals and correction insulin bolus for hyperglycemia can help prevent post-prandial hyperglycemia.
A simple getting started strategy – 70/30 Insulin
A simple strategy I have used over many years, that I find safe and effective, is giving the basal-bolus premixed 70/30 insulin with the morning dose of steroid. A safe starting range is around 10 units in the morning and gradually increases 10-20% daily to get glucose to target. In addition, bolus coverage for carbs and hyperglycemia can be given at lunch and dinner.
Since blood sugars trend down overnight, nighttime NPH insulin is not usually needed.
Keeping it flexible
As the person starts recovering and steroid doses are gradually tapered down, it is important to also decrease the NPH insulin dose and bolus insulins to prevent hypoglycemia.
In conclusion:
Keeping blood sugars on target improves outcomes. For people with diabetes, steroids can cause a hyperglycemic crisis. Thoughtful and progressive management using NPH and bolus insulins can turn the tide and help get blood glucose levels to goal.
Join Coach Beverly at our Virtual Conference for more information on COVID and Diabetes Management Strategies.
Reference Articles
Glycemic Control in Hospitalized Patients with Diabetes Receiving Corticosteroids Using a Neutral Protamine Hagedorn Insulin Protocol: A Randomized Clinical Trial. Khowaja A, Alkhaddo JB, Rana Z, Fish L. Diabetes Ther. 2018 Aug;9(4):1647-1655.
How to Manage Steroid Diabetes in the Patient With Cancer
David S. Oyer, MD, FACE, Ajul Shah, BS, and Susan Bettenhausen, APRN, CDE, 2006
Virtual DiabetesEd Specialist Course
Earn 30+ CEs | April 15-17, 2021
Virtual DiabetesEd Specialist Program
Whether you are new to diabetes or a seasoned expert, you’ll benefit from this virtual conference with the latest research plus critical content that you can immediately apply to your clinical practice.
DiabetesEd Virtual Conference Flyer 2021
Diabetes Ed Virtual 3-Day Schedule 2021
Prepare for CDCES or BC-ADM certification or earn hours for renewal.
If you are interested in taking the CDCES or BC-ADM exam or are seeking a state of the art review of current diabetes care, this course is for you. Our team has been fine-tuning this course for over fifteen years, and we know what you need.
Can’t join live? No worries, your registration guarantees access to the recorded content through Dec 31, 2021!
Team of expert faculty includes:
- Diana Isaacs, PharmD, BCPS, BC-ADM, BCACP, CDCES – Educator of the Year, 2020
- Coach Beverly Thomassian, RN, MPH, CDCES, BC-ADM
- Ashley LaBrier, MS, RD, CDCES, Diabetes Program Coordinator
In addition to informative lectures, we also use group activities and case studies to highlight the essential knowledge, skills, and strategies needed to succeed in diabetes education today!
Your registrations include access to all the Online Sessions plus Bonus Courses through December 31st, 2021.