What are the treatment options for people with type 1 diabetes with a COVID infection hospitalized for Diabetes KetoAcidosis (DKA)?
The typical treatment for DKA is fluids coupled with an IV insulin drip. Given the frequent monitoring and ICU bed required for treatment of DKA with an insulin drip, there has been a renewed interest in treating DKA with subcutaneous or sub-q insulin.
But after doing some research, I discovered an excellent 2004 paper co-authored by Dr. Guillermo Umpierrez et al. on using Sub-Q Insulin to Treat DKA. After completing a study comparing treatment of DKA using sub-q insulin vs. insulin drip, the author’s conclude that sub-Q insulin treatment is a safe and effective alternative treatment to IV insulin in the management of people with mild or moderate DKA.
With a little more digging, I found 2 more recent papers that suggest considering Sub-Q insulin treatment as an option for mild or moderate DKA.
It is important to note that sub-Q insulin treatment for DKA is NOT recommended for patients with arterial hypotension, severe and complicated DKA, or with HHS.
Treating DKA with Sub-Q insulin Steps
Insulins: Use either rapid acting lispro or aspart insulin.
1st Bolus: Starting dose is 0.1 or 0.2 or 0.3 units/kg of insulin (depending on initial blood glucose and clinical presentation)
Example: Pt weighs 100 kg, give 100kg x 0.1 – 0.2 – 0.3 units/kg of insulin = 10 or 20 or 30 units insulin sub-q bolus respectively.
Next Step – Sub-q insulin every 2 hours | Give 0.1 – 0.2 units of insulin /kg every 2 hours until blood glucose is less than 250.
Example: Pt weighs 100 kg, give 100kg x 0.1 – 0.2 units/kg of insulin = 10 or 20 units insulin sub-q bolus respectively every 2 hours.
Blood glucose less than 250 | Now give 1/2 the sub-q insulin dose every 2 hours. Calculate 0.05 to 0.1 units/kg every 2 hours until glucose at target and ketosis is resolved.
Example: Pt weighs 100 kg, give 100kg x 0.05 – 0.1 units/kg of insulin = 5 or 10 units insulin sub-q bolus respectively every 2 hours.
Using scheduled subcutaneous insulin allows for safe and effective treatment in the emergency room and step-down units without the need for ICU care. Umpierrez et al
Please see reference chart and articles below for more detailed information.
Fluids and Electrolytes
Of course, fluid and electrolyte status needs to be assessed before starting insulin.
If the K+ is less than 3.3, hold insulin and start with IV fluids (NS or LR) first with potassium replacement. Once the K is stable, start the insulin injection every 2 hours (see article and flow chart below).
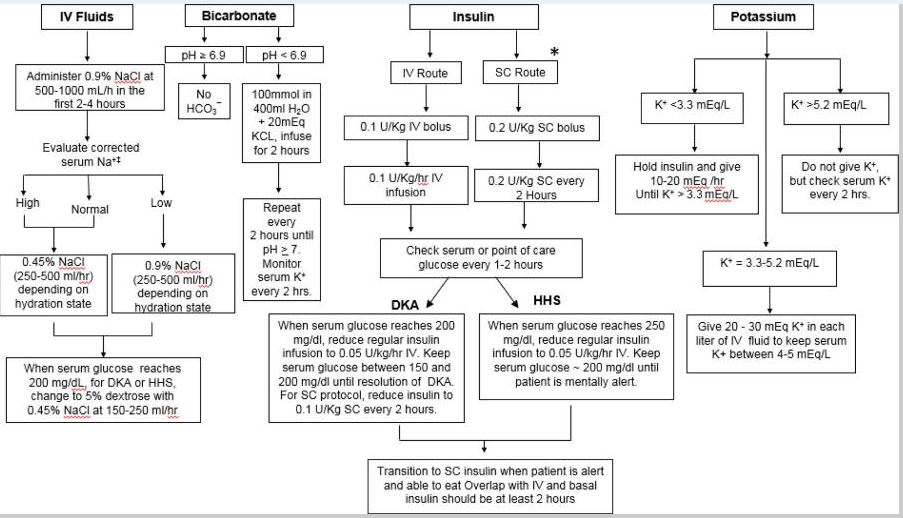
doi: 10.1016/j.mcna.2016.12.011
Management of Hyperglycemic Crises: Diabetic ketoacidosis and hyperglycemic hyperosmolar state
Thank you for reading this article. Please share any feedback or your experiences using sub-q insulin for DKA. We always love to hear from you. You can email us at [email protected]
Reference Articles
Eledrisi MS, Elzouki AN. Management of Diabetic Ketoacidosis in Adults: A Narrative Review. Saudi J Med Med Sci. 2020;8(3):165-173. doi:10.4103/sjmms.sjmms_478_19
Fayfman M, Pasquel FJ, Umpierrez GE. Management of Hyperglycemic Crises: Diabetic Ketoacidosis and Hyperglycemic Hyperosmolar State. Med Clin North Am. 2017;101(3):587-606. doi:10.1016/j.mcna.2016.12.011
Hyperglycemic Crises, DKA & HHS | 1.0 CEs
Join Coach Beverly to learn more about causes and treatment of hyperglycemic crisis. (opens in a new tab)”>Find out more here>>

This course is included in: Level 2 – Standards of Care. Purchase this course individually for $19 or the entire bundle and save 70%.
This 60-minute course discusses common causes of hyperglycemia crises. Topics include hyperglycemia secondary to medications and insulin deprivation. The difference and similarities between Diabetes Ketoacidosis and Hyperosmolar Hyperglycemic Syndrome are also covered. Treatment strategies for all situations are included.
Topics include:
- Common causes of hyperglycemic crises.
- The difference and similarities between DKA and HHS and treatment strategies
- Causes and treatment of hyperglycemic crises.
Sign up for Diabetes Blog Bytes – we post one daily Blog Byte from Monday to Friday. And of course, Tuesday is our Question of the Week. It’s Informative and FREE! Sign up below!
[yikes-mailchimp form=”1″]
Accreditation: Diabetes Education Services is an approved provider by the California Board of Registered Nursing, Provider 12640, and Commission on Dietetic Registration (CDR), Provider DI002. Since these programs are approved by the CDR it satisfies the CE requirements for the CDCES regardless of your profession.*
The use of DES products does not guarantee the successful passage of the CDCES exam. CBDCE does not endorse any preparatory or review materials for the CDCES exam, except for those published by CBDCE.