Besides being a diabetes educator and advocate for person-centered care, I am also a patient who has to navigate our healthcare system. I have regular appointments with my team of healthcare providers to address several chronic health issues I have acquired over the past decade. Like many of us, I have a difficult relationship with my weight and a long history of entangling my self-worth with the numbers on the scale. As a chunky kid, I never reached an “ideal body weight” until my twenties. Later, I fought hard to keep my BMI under 25, thinking that would increase my feelings of worth. I later realized this was a myth.
Since weighing myself caused such emotional turmoil, starting in my 30s, I refused to check my weight for the next twenty years (except during my pregnancies).
However, since I had a stroke eight years ago, and soon after that, I was diagnosed with Hashimoto’s thyroiditis, I decided to start weighing myself again. Then menopause hit.
My weight increased despite taking thyroid medication and maintaining an active lifestyle.
My weight distress re-emerged and reared its ugly head.
I knew I wanted to address my internalized weight stigma, and I devised several effective changes.
For example, when at the provider’s office, I would provide a “stated weight.” I would kindly let the medical assistant (MA) know there is no need to weigh me on your clinic scale.
As a knowledgeable healthcare professional in the current era, I know I can gently refuse to be weighed, and this does not mean I am ‘non-compliant”, difficult, or demanding. I am simply stating my needs.
I felt liberated and was no longer fearful of going to my doctor visits. This approach has been successful for the past six months, and l felt incredibly empowered.
Sadly, this sense of empowerment crumbled at my last provider visit. Here is how it all went down.
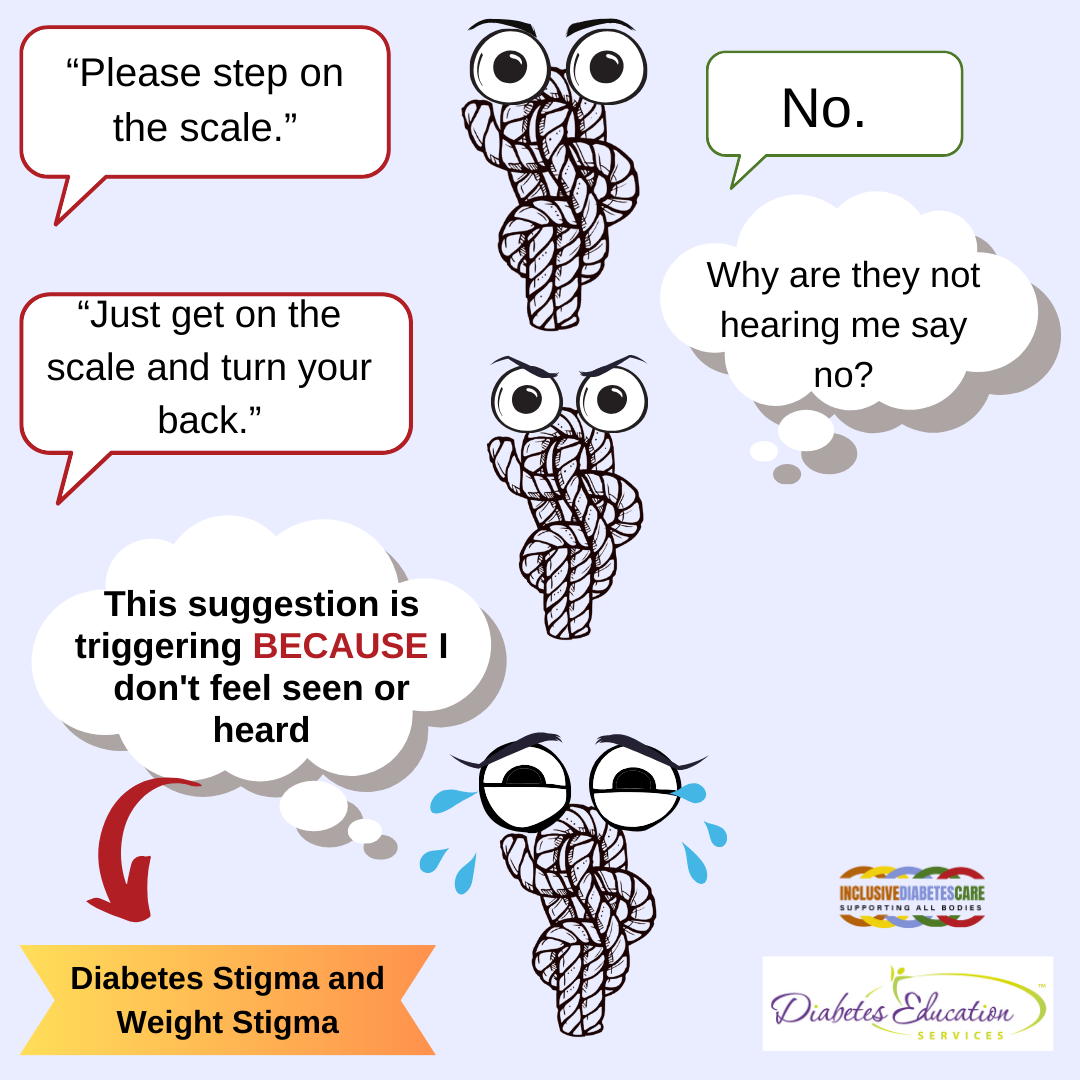
They called my name for my appointment, and MA greeted me with a warm smile and asked me to “please stand on the scale.” The scale is in the center of a busy office, where everyone can easily observe the measurement.
I smile back at him and say, “No, thank you. I am happy to share my stated weight.”
Confused, he looked at me and said, “No, you need to get on the scale.”
Still smiling, I pleasantly said, “No, I’m happy to give you my stated weight.”
The MA was bewildered by my continued refusal and unsure what to do next. We stood at the scale in an uncomfortable silence.
A provider who overheard the conversation came out of their office and walked over. The provider had two choices: to support my autonomy or to go with the status quo. It takes courage to buck the system, and my courage as a patient wasn’t enough.
Like many of us, they repeated the instructions and stated, “Just get on the scale and turn your back so you don’t have to see the number.”
In a last desperate attempt to lower the number on the scale, I toss off my shoes, let out a big sigh, and stand on the scale with my back to the readout.
“I am being bullied into getting weighed.”
Tears of anger and humiliation rolled down my cheeks.
Despite my privilege as a medical professional, my simple, repeated requests not to be weighed were ignored.
I started thinking about all the people living with diabetes who struggle with internalized weight stigma and how this intersects with diabetes stigma. Understanding intersectional stigma is hard, and change takes time, even for well-meaning healthcare professionals.
I reached out to Megrette Fletcher, M.Ed., R.D., CDCES, owner of Inclusive Diabetes Care, a continuing education company that created the Inclusion Pyramid, to help me make sense of this uncomfortable interaction with my healthcare team.
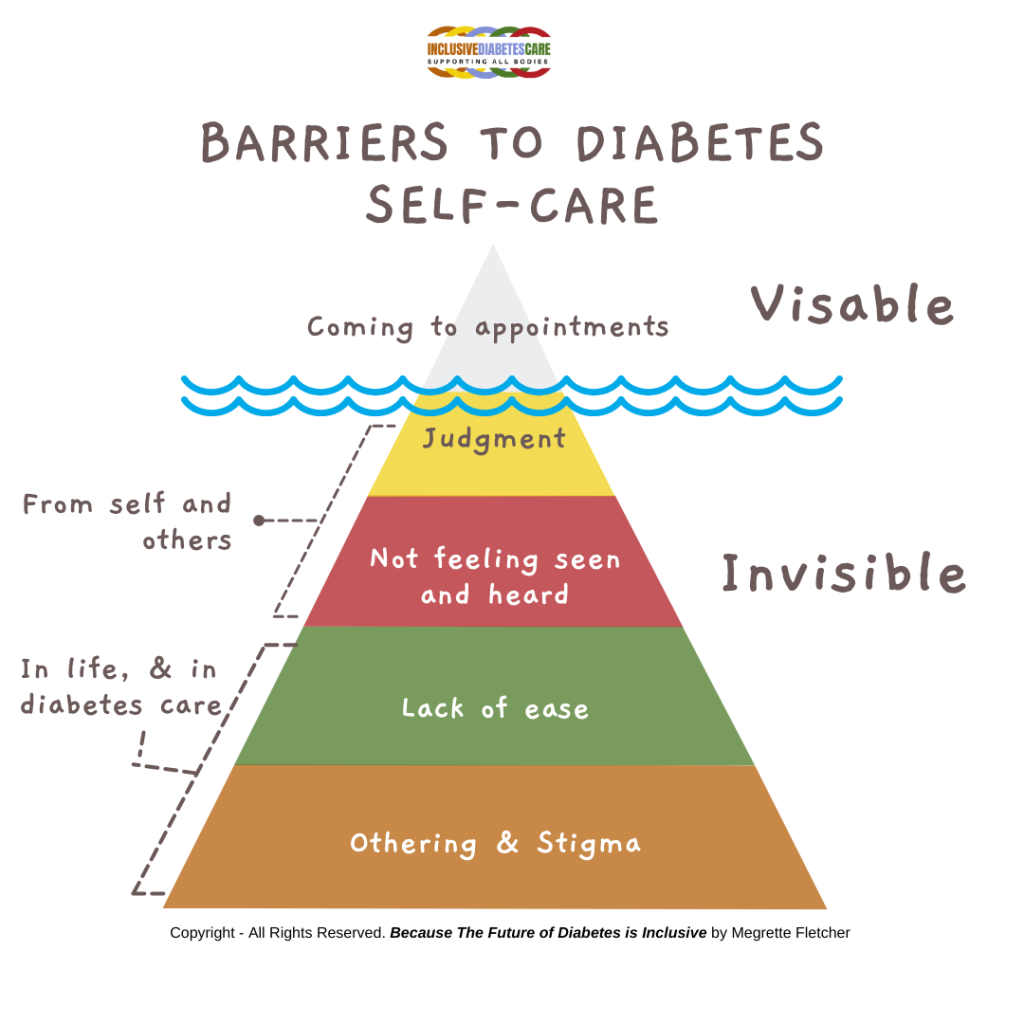
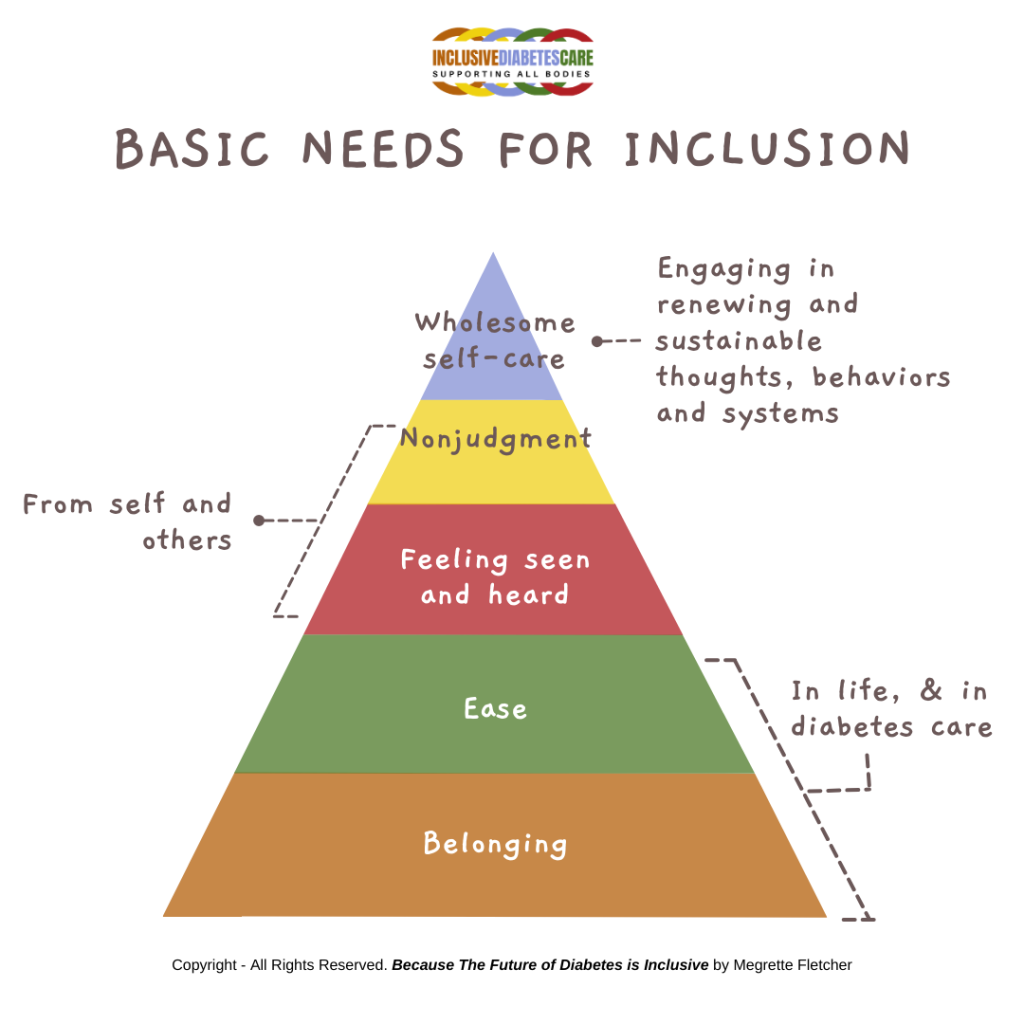
This simple model illustrates the often-invisible need for belonging, ease, feeling seen and heard, and nonjudgment are not met, and this creates invisible barriers to sustainable self-care.
My personal experience of being weighed is just one example of how othering and stigma can be experienced in medicine. As diabetes care and education specialists, we can role model weight inclusivity and make sure that each individual we serve, feels seen, heard and respected. We know that many people with diabetes in larger bodies may skip their medical appointments due to fear of being weighed or judged by healthcare professionals.
As you can see in the Inclusive Care pyramid below, we all have Basic Needs for Inclusion to actualize wholesome self-care. In the Barriers to Diabetes Self-Care Pyramid, feelings of othering, lack of ease, judgment and not feeling heard or seen can lead to no-shows and act as a barrier to receiving health care. When we focus on weight as a primary health indicator, we are missing opportunities to make meaningful connections with individuals and discover other contributing factors to their disease.
Weight stigma in medical appointments is a significant issue that can have detrimental effects on the individuals’ physical and mental health. It refers to the negative attitudes, beliefs, and stereotypes healthcare providers may hold towards individuals with extra weight. This stigma can manifest in various ways during medical appointments, including biased treatment, assumptions about the person’s lifestyle or health behaviors, and even neglect of legitimate health concerns unrelated to weight.
My goal in sharing my personal experience with all of you is not only to raise awareness of this often-overlooked barrier to care but a call to take action in our places of work.
Action Steps to Untangle Weight Stigma in Medical Appointments:
Awareness and Education: participate in training programs to help care providers recognize and address weight bias. A great resource is Inclusive Diabetes Care.
Language Matters: Use neutral and respectful language when discussing weight-related issues.
Focus on Health, Not Weight: Shift the focus of medical appointments from weight to overall health and well-being.
Individualized Care: Recognize the individual and understand their story around weight.
Create Supportive Environments: Design healthcare settings that are inclusive and welcoming to individuals of all sizes.
Advocate for Systemic Change: Addressing weight stigma requires systemic change within the healthcare system and society as a whole. Healthcare providers can advocate for policies that promote health equity, combat weight bias in research and media, and support initiatives that address social determinants of health.
By implementing these strategies, healthcare providers can help untangle weight stigma in medical appointments and create a more supportive and inclusive environment for all patients, regardless of their size.
We invite you to share your comments and experiences.
Have you experienced weight stigma and would like to share your story? Have you taken actions in your work setting to promote body positivity?
Please feel free to share anonymously on this google doc so we can continue this conversation.
Sign up for Diabetes Blog Bytes – we post weekly Blog Bytes that are informative and FREE! Every week we post one exam practice Question of the Week and Rationale of the Week. Sign up below!
Recent Blog Bytes
Accreditation: Diabetes Education Services is an approved provider by the California Board of Registered Nursing, Provider 12640, and our CPEU courses have received Prior Approval* from the Commission of Dietetic Registration (CDR), Provider DI002. Since our CPEU courses received Prior approval* from the CDR, these CPEU courses satisfy the CE requirements for the CDCES /BC-ADM regardless of your profession!
The use of DES products does not guarantee the successful passage of the certification exam. CBDCE and ADCES do not endorse any preparatory or review materials for the CDCES or BC-ADM exams, except for those published by CBDCE & ADCES.


