In preparation for my updating my class “Basal Bolus Therapy in the Hospital Setting“, a quick google search on the latest trends in hospital and diabetes care highlighted this just-published article to my immediate attention.
Management of diabetes and hyperglycemia in the hospital – Lancet 2021: 9 174-288 published in March 2021, provides evidence-based information and easy-to-use algorithms on managing hyperglycemia in the inpatient setting. It also addresses the use of CGM and insulin pumps in hospitals.
For this blog, I want to discuss some changes in approaches to hospital management, that I think is long overdue!
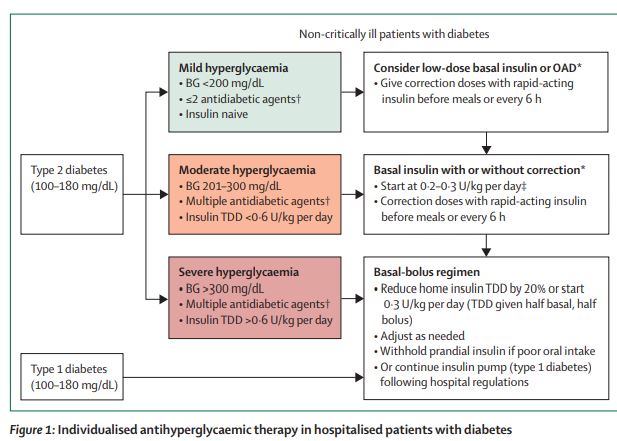
Take a look at the algorithm below and see if you agree with my takeaways below.
Coach Bev’s Takeaways
- For those with type 2 diabetes who have blood sugars under 200 mg/dl and who have never been on insulin (insulin naïve), instead of starting basal/bolus therapy, consider managing glucose with:
- low dose basal plus bolus correction with meals
- consider trying oral agents.
- In my opinion, this updated approach will help prevent hypoglycemia for those at the highest risk. Instead of a one-size-fits-all approach and starting everyone on basal/bolus insulin therapy, we can tailor our management strategies based on the person’s glucose treatment history.
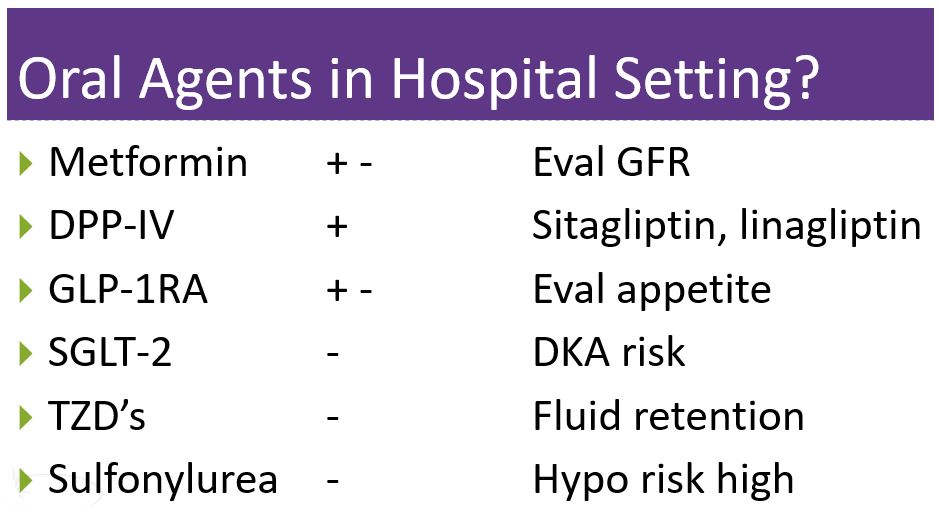
- Oral agents in the hospital? For the past several years, the ADA Standards have encouraged stopping non-insulin medications on hospital admission. However, the door seems to be reopening to allow for oral medications in combination with basal insulin, based on an individual assessment of benefit vs. risk.
- Based on the article, I created a list of medications and their appropriateness to treat hyperglycemia in the hospital. The DPP-IV inhibitors offer the benefit of no hypoglycemia, decreasing inflammation, and limited side effects. The other medications require careful consideration including length of hospital stay, patient acuity, renal function, eating status, and more.
As a hospital-based diabetes nurse for a few decades, I have watched the evolution of inpatient diabetes management. With this new article, it feels like we have reached a more thoughtful middle ground, based on evidence and clinical experience.
Certainly, the insulin sliding scale alone is not effective to manage glucose levels. But this nuanced approach of considering orals with low dose basal insulin for those at risk of hypoglycemia and using basal/bolus for those who are more insulin resistant makes good sense to me.
What do you think?
Learn more
I have more takeaways to share! Join Coach Beverly for her Basal Bolus Therapy in the Hospital Setting Webinar on May 6th at 11:30. And don’t worry if you can’t join us live, you will have access to the recorded version for a year after purchase.
Level 4 | Solving Glucose Mysteries for Type 2 | 1.5 CEs

Why are glucose levels elevated in the morning? When should insulin be started? What is the next step to get A1c to target?
During this 60-minute course Coach Beverly addresses each of these glucose mysteries and more, using a person-centered approach. She describes a stepwise approach to evaluate glucose patterns and correct common issues encountered by people living with type 2 diabetes.
By attending this webinar, you will gain confidence in evaluating glucose patterns and making recommendations for improvement.
Objectives
- Describe common glucose mysteries encountered by people with type 2 diabetes.
- Using a stepwise approach, evaluate factors affecting glucose patterns.
- State interventions to increase time-in-range and improve quality of life.
Sign up for Diabetes Blog Bytes – we post one daily Blog Byte from Monday to Friday. And of course, Tuesday is our Question of the Week. It’s Informative and FREE! Sign up below!
[yikes-mailchimp form=”1″]Accreditation: Diabetes Education Services is an approved provider by the California Board of Registered Nursing, Provider 12640, and Commission on Dietetic Registration (CDR), Provider DI002. Since these programs are approved by the CDR it satisfies the CE requirements for the CDCES regardless of your profession.*
The use of DES products does not guarantee the successful passage of the CDCES exam. CBDCE does not endorse any preparatory or review materials for the CDCES exam, except for those published by CBDCE.








