
For our May 18th Question of the Week, 76% of respondents chose the best answer, which is awesome! We still want to “take a closer look” at this question.
Before we start though, if you don’t want any spoilers and haven’t tried the question yet, you can answer below: Answer Question
Question: CT was diagnosed with type 2 diabetes three years ago. The current medication regimen includes 1000 mg of metformin twice daily and 70 units of glargine at night. CT wears an intermittent sensor, and you look at the glucose trends together on CT’s phone app. You both agree that there are consistent postmeal spikes up to 250 almost every day after lunch and dinner. The lowest blood sugar readings are in the 100s. BMI is 33.8 and CT says, “I never feel full”. The most recent A1C is 8.2%, urinary albumin creatinine ratio less than 30.
Based on this information, what intervention would be most likely help CT get to recommended ADA targets?
Answer Choices:
- Add on low-dose sulfonylurea to prevent hypoglycemia.
- Suggest adding a GLP-1 Receptor Agonist.
- Hold metformin, and switch to basal-bolus therapy.
- Encourage CT to get more active, especially after meals.
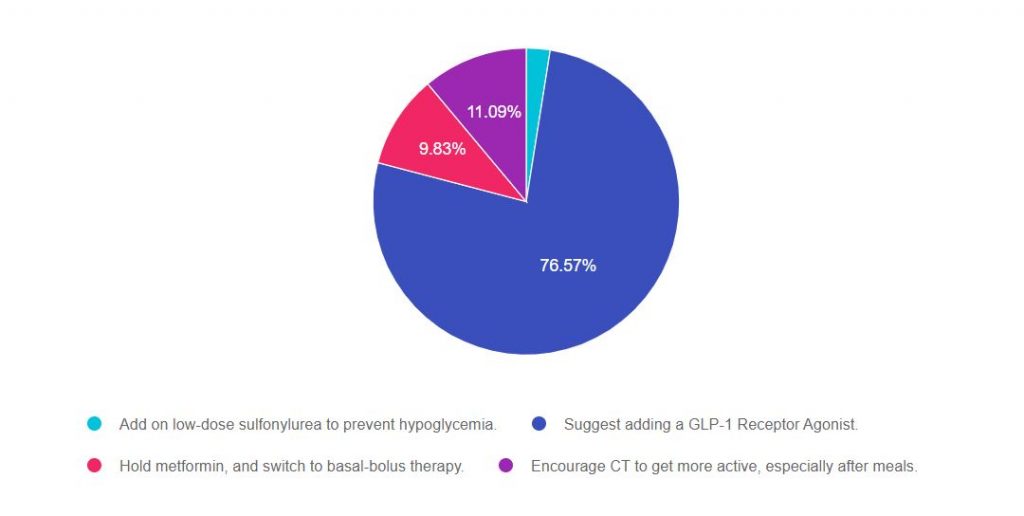
As shown above, the most common choice was option 2, the second most common answer was option 4, then option 3, and finally option 1.
Getting to the Best Answer
If you are thinking about taking the certification exam, the content of this practice test question will set you up for success. The exam will present questions that require test takers to be familiar with the stepwise approach to type 2 diabetes management in a variety of settings and situations.
For a complete listing of diabetes medications, please Download our Medication PocketCards.
Answers & Rationale
Answer 1 is incorrect, 2.51% chose this answer, “Add on low-dose sulfonylurea to prevent hypoglycemia.” Although we might consider this option, we can quickly identify a “tacked on” second half of the answer that makes it a wrong choice. One of the major side effects of sulfonylureas is hypoglycemia, so adding this class of medication wouldn’t prevent hypoglycemia, it would actually increase the risk of low blood sugars.
Answer 2 is correct, 76.57% of you chose this answer, “Suggest adding a GLP-1 Receptor Agonist.” GREAT JOB! Given the fact that CT is on 70 units of basal plus metformin and is experiencing postmeal spikes up to 250 almost every day after lunch and dinner and “never feels full”, adding a GLP-1 is the best choice. Adding a GLP-1 will decrease post meal hyperglycemia and postprandial glucose. In addition, GLP-1s can decrease appetite and increase feelings of satiation. Before suggesting addition of this medication class, it is important to consider insurance coverage and out of pocket cost, since cost could be a barrier.
Answer 3 is incorrect, 9.83% of you chose this answer, “Hold metformin, and switch to basal-bolus therapy.” According to the ADA, when initiating basal bolus insulin therapy for people with type 2 diabetes, they recommend continuing metformin to decrease insulin resistance. The ADA also suggests considering adding a GLP-1 RA or SGLT-2 Inhibitor before switching to basal bolus therapy.
Answer 4 is incorrect, 11.09% of you chose this answer, “Encourage CT to get more active, especially after meals.” While activity is important, this goal is very vague and not really actionable. In addition, “getting active after meals” will certainly improve health and is a great recommendation, but is not likely to drop the A1c to less than the goal of 7% or help with appetite.
We hope you appreciate this week’s rationale! Thank you so much for taking the time to answer our Question of the Week and participate in this fun learning activity!
Want to learn more about this topic? Join us for our upcoming
Level 4 | Solving Glucose Mysteries for Type 2 | 1.5 CEs | Ready to Watch!

Why are glucose levels elevated in the morning? When should insulin be started? What is the next step to get A1c to target?
During this course Coach Beverly addresses each of these glucose mysteries and more, using a person-centered approach. She describes a stepwise approach to evaluate glucose patterns and correct common issues encountered by people living with type 2 diabetes.
By attending this webinar, you will gain confidence in evaluating glucose patterns and making recommendations for improvement.
Objectives
- Describe common glucose mysteries encountered by people with type 2 diabetes.
- Using a stepwise approach, evaluate factors affecting glucose patterns.
- State interventions to increase time-in-range and improve quality of life.
Join us for our Live Webinars
Sign up for Diabetes Blog Bytes – we post one daily Blog Byte from Monday to Friday. And of course, Tuesday is our Question of the Week. It’s Informative and FREE! Sign up below!
[yikes-mailchimp form=”1″]Accreditation: Diabetes Education Services is an approved provider by the California Board of Registered Nursing, Provider 12640, and Commission on Dietetic Registration (CDR), Provider DI002. Since these programs are approved by the CDR it satisfies the CE requirements for the CDCES regardless of your profession.*
The use of DES products does not guarantee the successful passage of the CDCES exam. CBDCE does not endorse any preparatory or review materials for the CDCES exam, except for those published by CBDCE.









