Like millions of adults worldwide, our close family friend lived with undetected steatosis.
Up to 70% of people with diabetes have steatosis, which increases the risk for progressive liver disease. Unfortunately, much of the time, it is not discovered early enough.
Over 15 years ago, our friends’ steatosis progressed and quickly led to hepatocellular carcinoma. A cursory evaluation of his health history quickly highlights his risk of steatosis. He lived with diabetes for over ten years and had insulin resistance, as evidenced by his dark neck tan (acanthosis nigricans), hypertension, and a BMI well over 30. Even without any access to his lab data or complete medical history, we can easily assume that he was at risk for liver disease. Yet, he did not receive any diagnostic testing or nutrition counseling to address the silent inflammation that was wreaking havoc on his liver.
At 67, his steatohepatitis became evident as his confusion increased. His skin had a faint yellow tinge, and he “just wasn’t himself.” Months later, we were saying an early goodbye to a big-hearted, fearless man who loved his family and community and made a lasting impression on anyone he met.
We are not alone in this tragic story. The statistics are startling. About 70% of people with diabetes have steatosis, and of those, 50% are living with the more serious steatohepatitis, which can lead to severe liver fibrosis and scarring. Over time, these individuals are at risk of developing cirrhosis, liver cancer, and cardiovascular disease. Yet, we are only now catching up with this under-detected and often overlooked condition and its impact on individual and public health outcomes.
We can all become more actively involved in screening for liver disease and advocating for prompt action when it is detected. Together, we can save lives and share a message of hope!
Diabetes care and education specialists can Take Action!

According to the American Diabetes Association Standards of Care, here is a list of actions we can take to identify and prevent progression of liver disease.
- Lab Check: Encourage yearly evaluation of liver health and risk factors. Review annual ALT and AST levels and alert providers for values greater than 30 and evaluate Fib-4 Score.
- Calculate Fib-4 yearly to determine the risk of fibrosis and liver disease (you need the person’s age, ALT, AST, and platelet count). Encourage further imaging for those with elevated FIB-4.
- Take Action: For people with diabetes at higher risk of steatosis based on elevated insulin resistance (BMI 30+, cardiometabolic factors, age 50+), in addition to screening for liver disease, encourage immediate lifestyle changes that decrease steatosis risk and improve health – even before an official diagnosis!
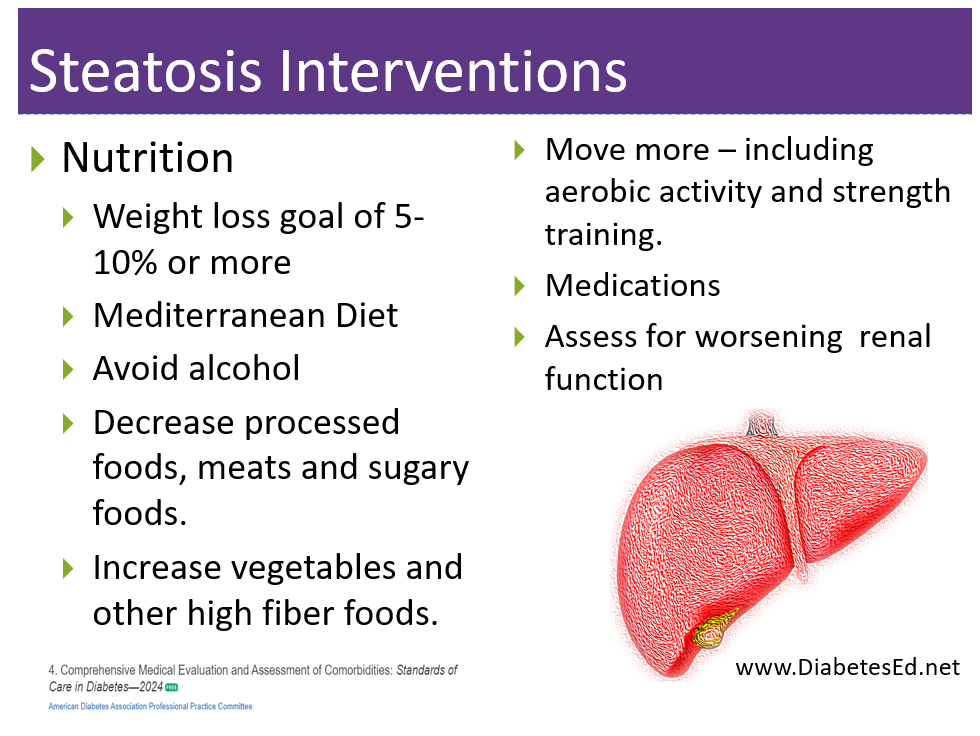
- Lifestyle changes:
- Refer to an RD/RDN for MNT therapy. In the meantime, encourage movement toward the Mediterranean Diet and a 5-10% weight reduction.
- Strength training at least twice weekly and increased activity (150 minutes a week) to improve insulin sensitivity.
- Even small changes in waist circumference indicate decreased visceral adiposity. These critical lifestyle changes decrease hepatic lipotoxicity and promote healing.
More than lifestyle change is often needed. Medications to Treat and Address Steatosis
The following medication is the first FDA-approved treatment for NASH and fibrosis.
- Rezdiffra (resmetirom) – The U.S. Food and Drug Administration approved Rezdiffra (resmetirom) in March 2024, for the treatment of adults with noncirrhotic, non-alcoholic steatohepatitis (NASH) with moderate to advanced liver scarring (fibrosis), to be used along with diet and exercise. Rezdiffra is a partial activator of a thyroid hormone receptor; activating this receptor by Rezdiffra in the liver reduces liver fat accumulation. “Previously, patients with NASH who also have notable liver scarring did not have a medication that could directly address their liver damage,” said Nikolay Nikolov, M.D., acting director of the Office of Immunology and Inflammation in the FDA’s Center for Drug Evaluation and Research. “Today’s approval of Rezdiffra will, for the first time, provide a treatment option for these patients, in addition to diet and exercise.”
The following medications are not specifically FDA-approved to treat liver disease but are recommended in the setting of diabetes and metabolic-associated steatosis/steatohepatitis.
Since steatosis and type 2 diabetes share underlying alterations in pathophysiology, including insulin resistance, it is not surprising that agents used to treat type 2 diabetes have demonstrated benefit in treating metabolic-associated steatosis and steatohepatitis.
- Pioglitazone (Actos) reduces blood glucose, and several studies demonstrate it is an effective treatment for steatosis and steatohepatitis. It also reduces the progression of fibrosis and cardiovascular risk. Since pioglitazone can cause fluid retention and weight gain, avoid using it in those with heart failure.
- GLP-1 RAs—this class of medication not only lowers blood glucose but can also lead to significant weight loss and a reduction in visceral adiposity and hepatocellular lipid levels. Several studies demonstrate that it is an effective treatment for steatosis and steatohepatitis. It also reduces the progression of fibrosis and cardiovascular risk.
- SGLT-2 Inhibitors – Recent research published in JAMA reveals that in a retrospective study, SGLT-2 Inhibitors were associated with a higher likelihood of liver disease regression among those with metabolic dysfunction-associated steatotic liver disease and type 2 diabetes. According to Dr. Won Kim, the study’s lead researcher, “SGLT2 inhibitors were distinguished by their association with fatty liver improvement, surpassing other [oral antidiabetic drugs] known for their potential benefits in steatosis.” More research is needed, but since this class of medication lowers blood glucose plus decreases cardiovascular risk, it is already widely used for people with diabetes and insulin resistance.
- Statin Therapy – Lipid-lowering and antihypertensive meds need to be prescribed in people with steatosis as indicated. Statins are safe in individuals with steatohepatitis but avoid their use in those with decompensated cirrhosis.
 A Final Note
A Final Note
Even though we lost our close friend due to undetected liver disease, I am hoping that by telling our story, all of us can become more actively involved in screening for liver disease and advocating for prompt action when it is detected. Together we can save lives and share a message of hope.
Coach Beverly
Resources: In addition to the ADA Standards, I utilized this article below, published in the Winter 2024 Edition of Diabetes Spectrum: Nonalcoholic Fatty Liver Disease: A Call to Action.
ReViVE 5 Diabetes Training Program:
Unlocking Hidden Barriers to Diabetes Management
June 17th & 24th, 2024
“ReVive 5” breathes new life into our relationship with diabetes, bringing a fresh perspective to both the person with diabetes and the provider.
The ReVive 5 program is built on sound research from the Embark Trial and will revolutionize your approach to diabetes self-management education.
We have reassembled the Embark training team and created a resource binder of fantastic tools that we are excited to share with you in our ReVive 5 Diabetes Training Program. You are invited to join us to learn a step-wise, proven approach to addressing hidden barriers to diabetes self-management and glucose management.
You don’t need to be mental health expert or diabetes technology wiz to join this training or to integrate these new strategies into your daily practice.
ReVive 5 uses an integrated, evidence-based approach that provides health care professionals with a realistic 5-step approach to addressing the whole person, starting with emotional distress and incorporating a unique, but integrated approach to problem-solving glucose management difficulties.
Intended Audience: This library of critical information is designed for individuals or groups of diabetes specialists, including RNs, RDs, Pharmacists, Nurse Practitioners, Clinical Nurse Specialists, Physician Assistants, and other health care providers interested in staying up to date on current practices of care for people with diabetes and preparing for the CDCES or BC-ADM Certification Exams.
Can’t join live? That’s okay. Your registration guarantees you access to the recorded version of the series, along with podcasts and resources for one full year.
Accredited Training Program:
- 15+ CEs – Includes the 7-hour ReVive 5 Training Program, Certificate, and 5 FREE bonus courses to supplement content.
- A comprehensive set of assessment tools, educational materials, log sheets, and resources.
Join us to gain the confidence and learn the skills needed to support people with diabetes to move forward in their self-management and discover the expert within.
Team of Experts:
ReVive 5 is taught by a team of 3 Interdisciplinary Experts:
- Lawrence Fisher, Ph.D., ABPP, Professor Emeritus, UCSF
- Susan Guzman, PhD
- Beverly Thomassian, RN, MPH, CDCES, BC-ADM
Speakers Interviews – Learn more about the ReVive 5 Team
Sign up for Diabetes Blog Bytes – we post weekly Blog Bytes that are informative and FREE! Every week we post one exam practice Question of the Week and Rationale of the Week. Sign up below!
Recent Blog Bytes
Accreditation: Diabetes Education Services is an approved provider by the California Board of Registered Nursing, Provider 12640, and our CPEU courses have received Prior Approval* from the Commission of Dietetic Registration (CDR), Provider DI002. Since our CPEU courses received Prior approval* from the CDR, these CPEU courses satisfy the CE requirements for the CDCES /BC-ADM regardless of your profession!
The use of DES products does not guarantee the successful passage of the certification exam. CBDCE and ADCES do not endorse any preparatory or review materials for the CDCES or BC-ADM exams, except for those published by CBDCE & ADCES.