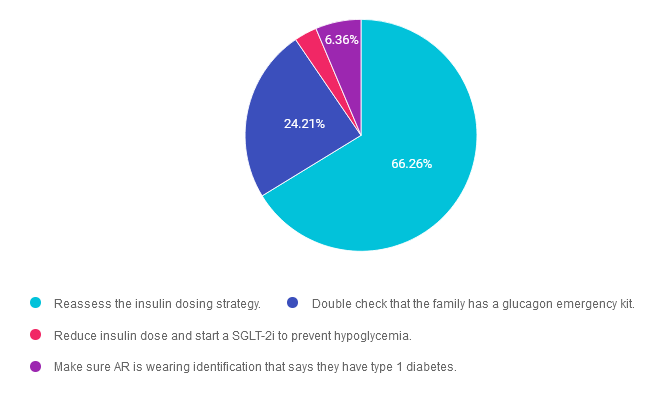
For last week’s practice question, we quizzed participants on type 1 and food insecurity. About two thirds of respondents chose the best answer. We want to clarify and share this important information, so you can pass it on to people living with diabetes and your colleagues, plus prepare for exam success!
Before we start though, if you don’t want any spoilers and haven’t tried the question yet, you can answer it below: Answer Question

Question:
AR is an 8 year old with type 1 diabetes who has a CGM but still uses insulin injections due to lack of insurance coverage. AR’s parents struggle with food insecurity and some days AR only has school provided breakfast and lunch. You notice he is experiencing level 1 hypoglycemia frequently around 6pm.
What is the best first intervention?
Answer Choices:
- Reassess the insulin dosing strategy.
- Double check that the family has a glucagon emergency kit.
- Reduce insulin dose and start a SGLT-2i to prevent hypoglycemia.
- Make sure AR is wearing identification that says they have type 1 diabetes.
Getting to the Best Answer
Answer 1 is correct. 66.26% chose this answer. “Reassess the insulin dosing strategy.” YES, this is the BEST answer. GREAT JOB! It appears that JR may not have adequate food intake on some days in the early evening hours. To compensate for this decreased food intake, the insulin dose will most likely need to be lowered to prevent dinnertime hypoglycemia. Of course, we would also need to connect AR and their family with social services and other resources.
Answer 2 is incorrect. 24.21% of you chose this answer. “Double check that the family has a glucagon emergency kit.” Although it is important for all people living with type 1 diabetes to have a glucagon rescue medication, the first goal is to prevent severe hypoglycemia. In this situation, the first action is to adjust the insulin dose to prevent dinnertime hypoglycemia. Of course, we would also need to connect AR and their family with social services and other resources.
Answer 3 is incorrect. About 3.18% of respondents chose this. “Reduce insulin dose and start a SGLT-2i to prevent hypoglycemia.” In this situation, the first action is to adjust the insulin dose to prevent dinnertime hypoglycemia. SGLT-2’s are off label for people living with type 1 diabetes and since AR is not in a stable situation, this would not be a good time to evaluate the effectiveness of adding on an SGLT. Of course, we would also need to connect AR and their family with social services and other resources.
Finally, Answer 4 is incorrect. 6.36% chose this answer. “Make sure AR is wearing identification that says they have type 1 diabetes.” Yes, wearing identification is recommended for people living with type 1 diabetes, but more importantly, we want to prevent hypoglycemia. In this situation, the first action is to adjust the insulin dose to prevent dinnertime hypoglycemia. Of course, we would also need to connect AR and their family with social services and other resources.
We hope you appreciate this week’s rationale! Thank you so much for taking the time to answer our Question of the Week and participate in this fun learning activity!
Want to learn more about this question?
Join us live on November 13, 11:30 am PST for our
FREE Prep for CDCES Exam Webinar
Join us to get ready to succeed a the CDCES Exam. This course will transform your test anxiety into calm self-confidence and test taking readiness. Topics covered include:
- Changes in requirements for 2024
- Exam eligibility and the updated test format
- Strategies to succeed
- Review of study tips and test taking tactics.
We will review sample test questions, and the reasoning behind choosing the right answers.
After registering, you will receive a confirmation email containing information about joining the webinar.
Intended Audience: This FREE webinar is designed for individual or groups of diabetes educators, including RNs, RDs, Pharmacists, Nurse Practitioners, Clinical Nurse Specialists, Physician Assistants and other health care providers interested in achieving excellence in diabetes care and becoming Certified Diabetes Care and Education Specialists®.
Instructor: Beverly Thomassian RN, MPH, CDCES, BC-ADM is a working educator who has passed her CDCES Exam 7 times. She is a nationally recognized diabetes expert for over 25 years.
Sign up for Diabetes Blog Bytes – we post weekly Blog Bytes that are informative and FREE! Every week we post one exam practice Question of the Week and Rationale of the Week. Sign up below!
Recent Blog Bytes
- Rationale of the Week | What Does J.C.’s Family History & Lab Work Reveal?
- Red Flags for Low Digital Literacy in Diabetes Care
- Question of the Week | Best Response for Facilitating Positive Health Behavior Change?
- Rationale of the Week | What to Assess When Looking for PAD?
- Grief and the Role of the Diabetes Educator
The use of DES products does not guarantee the successful passage of the certification exam. CBDCE and ADCES do not endorse any preparatory or review materials for the CDCES or BC-ADM exams, except for those published by CBDCE & ADCES.









