
Fasting has been practiced for centuries, rooted in spiritual, religious, and medical traditions. Religious fasting can be found throughout cultures and faith-based traditions, such as Islam, Judaism, Christianity, Buddhism, and Hinduism, as well as in Native American tribal ceremonies. During Ramadan, an Islam holy month, fasting occurs from dawn to dusk from February 28 through March 29th.
Christians may observe daily fasting, alternate-day fasting, or an abstinence during the 40 days of Lent. While many religions have exceptions for individuals with chronic conditions, including diabetes, many may choose to participate in fasting.
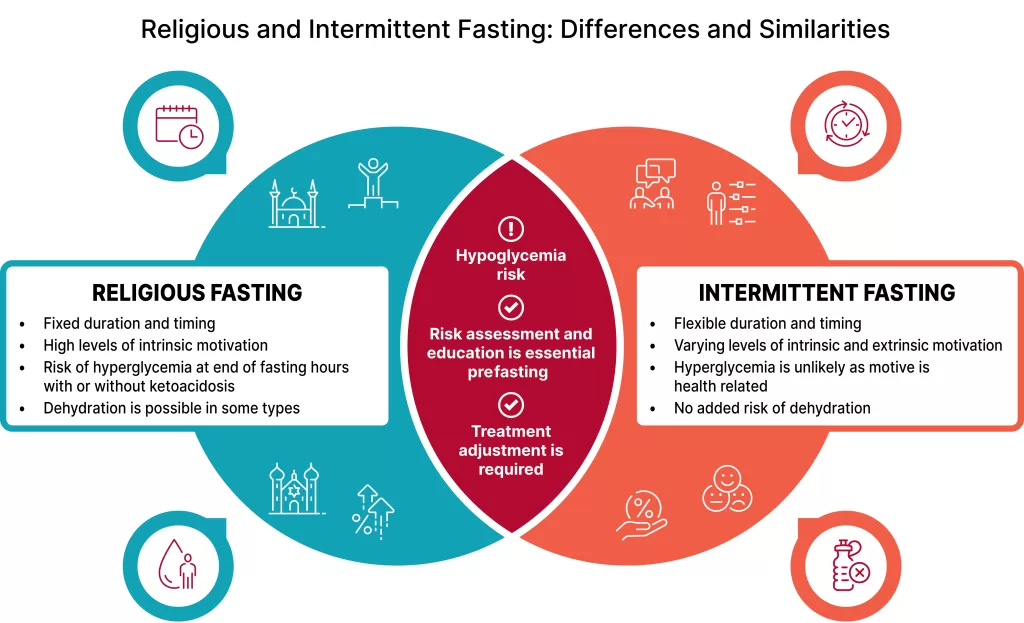
Religious fasting has distinct differences from dietary fasting.
The intention, motivation, duration, frequency, of these approaches differ significantly. Fasting for health and longevity practices can be found in early ancient Ayurvedic medicine and modern intermittent fasting trends. Therapeutically, 5th-century Greek physician Hippocrates recommended fasting for symptoms of certain illnesses. In recent years, researchers have explored the metabolic effects of fasting, particularly its role in insulin sensitivity and glucose control, sparking interest in its potential benefits and risks for individuals with diabetes.
The American Diabetes Association (ADA) has recognized the importance of understanding how fasting may play a role in the lives of individuals with diabetes. The 2025 Standards of Care have been updated to provide more structured guidance (see infographic below).
The new recommendations highlight individualized care plans, focusing on pre-fasting risk assessments, medication adjustments, and glucose monitoring strategies to ensure safety during fasting.1 To assess risk, clinicians are encouraged to consider the duration of fast, type of diabetes, daily activity, and individual diabetes risk factors while using standardized tools, such as the International Diabetes Federation-Diabetes and Ramadan International Alliance (IDF-DAR) risk tool.2
While the type and duration of fasting may differ, this risk calculator may also provide assessment of risk for varying religious fasting and may guide fasting-focused education to minimize risks of hypoglycemia, hyperglycemia, and dehydration.
Although religious and non-religious fasting may have differences in intention and motivation for the individual living with diabetes, risk assessment, education, and treatment adjustment are recommended for all.
Medication modifications are typically required for individuals on high-risk therapies such as insulin or sulfonylureas.
The Standards of Care guidelines emphasize pre-fasting education on the frequency of glucose monitoring, encouraging continuous glucose monitoring (CGM) to optimize safety during fasting periods. Current knowledge reports that SGLT2 inhibitors do not need to be adjusted during fasting but should be withheld from initiation close to the start of fasting.1
For individuals with type 1 diabetes, insulin pump therapy helps reduce the risk of hypoglycemia during fasting by allowing for setting temporary basal rates or, in the case of Automated Insulin Delivery systems, modifying insulin delivery based on sensor glucose feedback.
A referral to a Registered Dietitian with expertise in religious fasting can provide personalized and culturally sensitive meal and fluid planning to prevent dehydration and minimize post-prandial hyperglycemia when breaking a fast, or hypoglycemia due to change in typical meal patterns. A comprehensive medication plan tailored to the individual’s risk factors, dietary intake, and medication regimen is crucial to ensuring safety during fasting.
Non-religious fasting typically has motivations in weight loss, improving metabolic risk factors, or longevity.
Intermittent fasting can comprise alternate-day fasting, or a 5:2 dietary plan, each involving low calorie (500-600 kcals) intake either every other day or two of seven days of the week. Time-restrictive eating is a daily practice in which the focus is on fasting and eating hours. The most common is the 16:8 method, in which an individual focuses on fasting for 16 hours, and eating is restricted to a planned 8 hours.
While evidence suggests that time-restricted eating and intermittent fasting results in 3-8% weight loss over 12 weeks and improved metabolic markers, the outcomes are comparable to consistent calorie reduction plans.1 Just as with all nutrition therapy approaches, interventions need to be individualized, ensuring dietary patterns are sustainable and align with cultural, religious, and personal preferences while maintaining glucose stability and overall well-being.
For diabetes educators, these updated guidelines reinforce the necessity of proactive counseling and culturally sensitive care.
By staying informed on best practices for fasting, diabetes care and education specialists can guide individuals in making informed decisions that support their faith and their health.
Education includes discussing medication modifications, meal planning strategies, safe exercise recommendations, and the importance of fluid balance during fasting periods. Providing clear, evidence-based recommendations ensures that individuals with diabetes feel supported in their tradition or dietary choice while also minimize health risks.
References:
- American Diabetes Association Professional Practice Committee; 5. Facilitating Positive Health Behaviors and Well-being to Improve Health Outcomes: Standards of Care in Diabetes—2024. Diabetes Care 1 January 2024; 47 (Supplement_1): S77–S110. https://doi.org/10.2337/dc24-S005
- International Diabetes Federation-Diabetes and Ramadan Alliance (IDF-DAR) Fasting Risk Assessment. Downloaded from https://www.mdcalc.com/calc/10522/international-diabetes-federation-diabetes-ramadan-alliance-idf-dar-fasting-risk-assessment on February 19th, 2024.
Want to hear more from this expert?

Gain fresh insights, practical tools, and a deeper understanding of the latest in person-centered diabetes care. Our expert team brings the ADA Standards of Care to life—covering medications, behavior change, technology, and more! If you’re preparing for the CDCES or BC-ADM exam, this conference—paired with free bonus courses—serves as the ideal study companion!
With interactive co-teaching, we keep sessions engaging, relevant, and fun. Let’s learn and grow together!

Our expert team transforms complex diabetes science into clear, practical insights—keeping it real, engaging, and fun! The faculty includes:
- Diana Isaacs, PharmD, BCPS, BC-ADM, BCACP, CDCES
- Coach Beverly Thomassian, RN, MPH, CDCES, BC-ADM
- Christine Craig, MS, RD, CDCES
- 3 Days: of critical information delivered by passionate speakers in an engaging and fun format!
- 11 Bonus Online Courses: As a course attendee, you automatically receive a bonus online course bundle of 11 online courses valued at over









