The content of this newly published guideline is thoughtful, person-centered, and offers a clear clinical path for the management of type 2 diabetes. I tip my hat to the authors in gratitude for their dedication and vision.
Besides having lots of attractive infographics and a fantastic summary of the research, this guideline offers evidence-based strategies to get glucose to the goal with an emphasis on taking a person-centered approach to pharmacologic and lifestyle interventions. We invite you to enjoy a detailed review by joining our webinar or reading this brief summary of the findings that impressed me most.
- Metformin doesn’t have to be the initial therapy.
This medication has enjoyed the number one seat in the ADA guidelines for over a decade. And for good reason. In addition to being low cost ($4 a month), it does not cause low blood sugar or weight gain and it lowers A1C by 1-2% points. Although it lowers LDL cholesterol, it is not officially recognized as a cardiovascular risk-lowering medication.
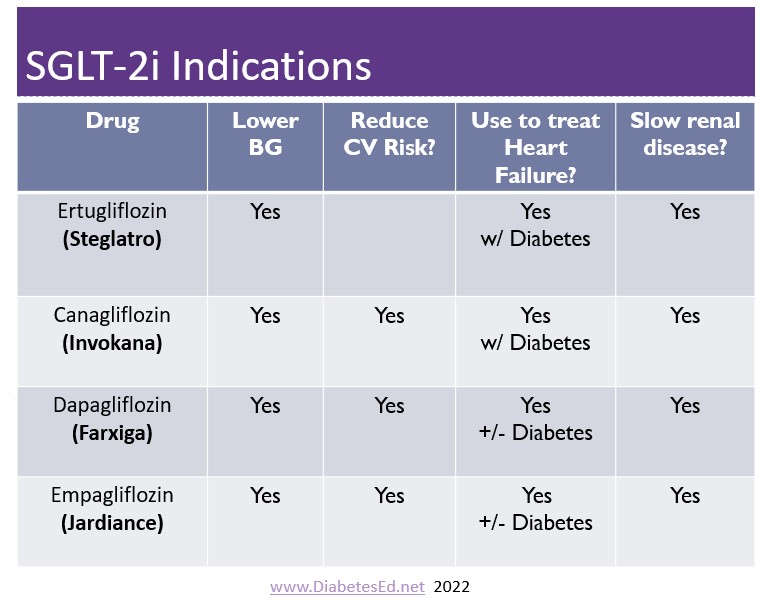
The guidelines state, that in addition to lifestyle interventions if there is a history of CV disease, heart failure, or kidney disease, we need to turn our gaze elsewhere and consider an SGLT-2 Inhibitor or a GLP-1 Receptor Agonist.
- Embrace Diabetes Self Management Education (DSMES) as being as important as other aspects of care, including pharmacotherapy.
This endorsement of the significance of DSMES in improving outcomes and quality of life in people living with diabetes is powerful. Research has demonstrated that people with diabetes who receive DSMES, including counseling by an RD/RDN, experience an A1C drop of 1-2%. In addition, they are less likely to be hospitalized, engage in more preventive behaviors, and know when to reach out for help. They go on to say that DSMES needs to offer on an ongoing basis, using a variety of delivery approaches, and should be accessible in all communities. - If GFR is 20 or greater and the UACR is 30mg/g or more, start SGLT-2 Inhibitors.
It doesn’t get much bolder than that statement. There is the fine print, that recognizes that clinicians can use their discretion and judgment, but the data is clear. The use of SGLT-2 slows the progression of kidney disease and can delay the need for dialysis. Even if glucose levels are at target, in the presence of renal failure, starting an SGLT-2 is indicated. Since the leading cause of death for those with kidney disease is CV events, if SGLT-2 can’t be tolerated for clinical reasons, using a GLP-1 with CV benefits would be the second choice. - In the presence of heart failure, start an SGLT-2 Inhibitor.
All four of the available SGLT-2 Inhibitors are effective “glucoretics” helping rid the body of excess sugar and fluid. This action has a significant impact on improving not only glucose levels but decreasing fluid overload thereby improving cardiac function. This class of medication is so effective at treating heart failure, that 2 of the 4 SGLT-2 meds are indicated to treat heart failure even in the absence of diabetes. - Weight loss Goals Intensified
Traditionally, in the recommendations, weight loss targets range from 5-7% for people with diabetes. However, these new guidelines suggest we aim for at least 5-10% weight loss with even better outcomes if people can lose 10-15% or more significant weight loss can lead to diabetes remission, improved metabolic profiles, and fewer complications. In the past, achieving these targets was usually linked to very low-calorie diets or metabolic surgery. However, with higher doses of the GLP-1 RA and the Dual GLP GIP Agonist, Tirzepatide, we have additional tools in our toolkit to get the job done.
6. The placement of Tirzepatide (Mounjaro)
In the new ADA/EASD Algorithm, there are 2 hierarchies of medication effectiveness, glucose, and weight impact. As its trade name suggests, tirzepatide is at the top of the mountain of both lists (along with semaglutide) for its glucose-lowering properties and weight loss efficacy. This medication was studied in people with diabetes (Surpass) and people without diabetes (Surmount).
In the diabetes group, at the highest dose, A1C dropped by over 2% and people experienced a 10% or greater weight loss. In the non—diabetes group, people experienced up to 20% weight loss. This medication is currently only approved for people with diabetes, but don’t be surprised if we see it on the market as a weight loss intervention for people without diabetes in the near future.
7. Keep it person-centered and Address Social Determinants of Health. The last version of the guidelines recognizes that we have to consider the needs, values, and goals of the individual PATIENT. In this newer version, they ditched the word “PATIENT” and finally replaced it with the term “PERSON”. This consensus statement also recognizes the importance of considering inequities in access to diabetes care and resources. They offer a comprehensive list of all of the social determinants of health to consider when providing care.
There is so much more to this article. I hope I have inspired you to read the complete ADA/EASD Consensus document or join our webinar on December 1st to learn more.
Meds for Type 2 Update; New ADA/EASD Consensus Statement
Level 2

Plan on joining this exciting webinar that walks participants through the newly released, “Management of Hyperglycemia in Type 2 Consensus Report by the ADA and EASD”. These updated guidelines will be incorporated into the 2023 ADA Standards of Care, but you can get a early sneak peak by joining Coach Beverly on December 1st, 2022. She will highlight the revised guidelines with a focus on new elements and exciting changes on how we approach medication management for type 2 diabetes. Together, we will explore clinical factors to consider when determining the best strategy to improve glucose management in people with type 2 diabetes and other co-conditions. There will be a special focus on cardiovascular risk reduction and renal protection and addressing clinical inertia.
Objectives:
- Describe the role of Diabetes Care and Education Specialists in advocating for optimal therapeutic approaches.
- Discuss the application of the new ADA/EASD Guidelines to improve glucose and reduce CV and renal risk.
- List strategies to initiate and adjust oral and injectable therapy using a person-centered approach
Intended Audience: A great course for health care professionals seeking evidence-based information that improves the quality of life and outcomes.
Don’t worry if you can’t make it live. Your registration guarantees access to the recorded version in the Online University.
All hours earned count toward your CDCES and BC-ADM Exam Accreditation Information


