
Subscribe
eNewsletter

Ready to get certified?
Free CDCES Coach App
Download
Free Med Pocket Cards
JR is 64 years old, in hospital with type 2 diabetes and COVID. JR normally manages their diabetes with metformin, but during this inpatient stay, JR is on prednisone therapy which has spiked sugar levels into the 250 mg/dl to 350 range. JR is receiving bolus insulin sliding scale with meals and bedtime glargine, but blood sugars are persistently elevated. To improve outcomes for JR, it is important to keep blood glucose levels less than 180 mg/dl, but what should we recommend to get glucose to goal?
What are some strategies to get blood sugar to target while on steroids?
There is no consensus on the best approach to manage this situation. Up until this point in history, steroid-induced hyperglycemia was mostly found in people with diabetes in COPD, those undergoing chemotherapy or in post-transplant situations.

With the COVID pandemic, many people with diabetes in hospitals and at home, are on steroids. Health care professionals are trying to figure out how to lower glucose levels.
For people with type 2 diabetes and COVID, the latest research indicates that sitagliptin (Januvia) not only helps maintain blood glucose but also decreases the inflammatory response associated with COVID infections. If not contraindicated, sitagliptin can be used in conjunction with insulin, to treat the extreme insulin resistance and hyperglycemia caused by steroid therapy.
To treat steroid induced hyperglycemia, we are going to call on our old insulin friend, NPH. Neutral Protamine Hagedorn (NPH) is an intermediate acting basal insulin. NPH insulin is made by mixing regular insulin and protamine in exact proportions with zinc and phenol such that a neutral-pH is maintained and crystals form.
NPH insulin is cloudy and has an onset of 1–4 hours. Its peak is 6–10 hours and its duration is about 10–16 hours.
Steroids have their highest potency at 4-12 hours, with the exception of the very potent dexamethasone, which has a half life of 1-2 days.
However, with all steroids, including dexamethasone, people will experience elevated glucose values after breakfast, lunch, dinner, and at bedtime but will have a significant drop toward normal glucose overnight.
Therefore, hyperglycemia is greatest 1–2 hours after a meal, with persistent elevation until the following meal, followed by a return to normal overnight.

NPH Insulin Dosing Strategies
There are several articles (see below) that recommend a variety of NPH dosing strategies. Generally, insulin dosing is based on a combination of steroid dose and body weight. For those on lower dose steroid (ie less than 40 mg prednisone daily) a starting NPH insulin dose of 0.1 – 0.2 units per kg is reasonable. If JR weighs 100 kg, that means 10 to 20 units of NPH daily.
If JR is on a higher steroid dose, or blood sugars are extremely elevated, JR may need 0.3 units/kg or 30 units of NPH daily. Of course, we also need to keep nutritional status in mind as we determine best dose. People who are not eating or NPO, will require less insulin, even in the presence of steroids.
The timing of NPH administration matches the timing of the steroid therapy.
In addition, coverage for carbohydrates at meals and correction insulin bolus for hyperglycemia can help prevent post-prandial hyperglycemia.
A simple getting started strategy – 70/30 Insulin
A simple strategy I have used over many years, that I find safe and effective, is giving the basal-bolus premixed 70/30 insulin with the morning dose of steroid. A safe starting range is around 10 units in the morning and gradually increases 10-20% daily to get glucose to target. In addition, bolus coverage for carbs and hyperglycemia can be given at lunch and dinner.
Since blood sugars trend down overnight, nighttime NPH insulin is not usually needed.
Keeping it flexible
As the person starts recovering and steroid doses are gradually tapered down, it is important to also decrease the NPH insulin dose and bolus insulins to prevent hypoglycemia.
In conclusion:
Keeping blood sugars on target improves outcomes. For people with diabetes, steroids can cause a hyperglycemic crisis. Thoughtful and progressive management using NPH and bolus insulins can turn the tide and help get blood glucose levels to goal.
Join Coach Beverly at our Virtual Conference for more information on COVID and Diabetes Management Strategies.
Glycemic Control in Hospitalized Patients with Diabetes Receiving Corticosteroids Using a Neutral Protamine Hagedorn Insulin Protocol: A Randomized Clinical Trial. Khowaja A, Alkhaddo JB, Rana Z, Fish L. Diabetes Ther. 2018 Aug;9(4):1647-1655.
How to Manage Steroid Diabetes in the Patient With Cancer
David S. Oyer, MD, FACE, Ajul Shah, BS, and Susan Bettenhausen, APRN, CDE, 2006
Whether you are new to diabetes or a seasoned expert, you’ll benefit from this virtual conference with the latest research plus critical content that you can immediately apply to your clinical practice.
Prepare for CDCES or BC-ADM certification or earn hours for renewal.
If you are interested in taking the CDCES or BC-ADM exam or are seeking a state of the art review of current diabetes care, this course is for you. Our team has been fine-tuning this course for over fifteen years, and we know what you need.
Team of expert faculty includes:
In addition to informative lectures, we also use group activities and case studies to highlight the essential knowledge, skills, and strategies needed to succeed in diabetes education today!
Your registrations include access to all the Online Sessions plus Bonus Courses through December 31st, 2021.
Virtual DiabetesEd Specialist Conference | April 15-17, 2021

Whether you are new to diabetes or a seasoned expert, you’ll benefit from this virtual conference with the latest research plus critical content that you can immediately apply to your clinical practice.
Entire Program Fee: $399
Dates: April 15-17, 2021
Live Webinar Schedule: All webinars start and end times are in Pacific Standard Time
Coach Beverly Thomassian, RN, MPH, BC-ADM, CDCES

Author, Nurse, Educator, Clinician and Innovator, Beverly has specialized in diabetes management for over twenty years. As president and founder of Diabetes Educational Services, Beverly is dedicated to optimizing diabetes care and improving the lives of those with diabetes.
Diana Isaacs, PharmD, BCPS, BC-ADM, BCACP, CDCES

We are thrilled to welcome our newest speaker, Diana Isaacs, who will be joining our Virtual and Live Courses!
Dr. Isaacs was named 2020 AADE Diabetes Educator of the Year for her educational platform promoting the use of CGM for people with diabetes and other innovations. Dr. Isaacs was awarded the Ohio Pharmacists Association Under 40 Award in 2019. Dr. Isaacs has served in leadership roles for several pharmacies and diabetes organizations. She has numerous diabetes publications and research projects with a focus on medications, CGM and diabetes technology.
As the CGM Program Coordinator and clinical pharmacist specialist in the Cleveland Clinic Diabetes Center, Dr. Isaacs brings a wealth of clinical knowledge combined with extensive research experience to this program.
Diabetes Meds and Insulin Toolkit – with Dr. Diana Isaacs | 4.0 CEs
April 15 10:30 am – 12:30 BREAK and 1:15 – 3:15 PST
*Topics include:
Technology Toolkit with CV Management Update – Dr. Diana Isaacs | 4.0 CEs –
April 16 with 8:30—12:30 am
Ashley LaBrier, MS, RD, CDCES

Ashley is an educator, dietitian, and the Diabetes Education Program Coordinator at the Salinas Valley Medical Clinic’s Diabetes & Endocrine Center. Her work with people living with diabetes focuses on the value of healthy nutrition and movement to improve well-being.
Ashley is passionate about providing person-centered education to empower those who live with diabetes. Having been diagnosed with type 1 diabetes herself nearly 20 years ago, she combines her professional knowledge with personal experience and understanding.
April 17 with Ashley LaBrier, MS, RD, CDCES
8:30 am — 12:30 pm PST
*Dates and times subject to change. Course start and end time are for Pacific Standard Timezone.
Bonus Courses – Course registration includes FREE enrollment into our Level 2 Standard of Care Course Series including:
Team of expert faculty includes:
In addition to informative lectures, we also use group activities and case studies to highlight the essential knowledge, skills, and strategies needed to succeed in diabetes education today!
Prepare for CDCES or BC-ADM certification or earn hours for renewal.
Your registrations include access to all the Online Sessions plus Bonus Courses through December 31st, 2021.
This virtual program includes:
3 day live webinar courses from April 15th-17th (20 CEs) + enrollment in our Bonus Bundle (14.0+ CEs) from now through December 2021.
View full Conference Schedule and Faculty.
Sign up for Diabetes Blog Bytes – we post one daily Blog Byte from Monday to Friday. And of course, Tuesday is our Question of the Week. It’s Informative and FREE! Sign up below!
[yikes-mailchimp form=”1″]Accreditation: Diabetes Education Services is an approved provider by the California Board of Registered Nursing, Provider 12640, and Commission on Dietetic Registration (CDR), Provider DI002. Since these programs are approved by the CDR it satisfies the CE requirements for the CDCES regardless of your profession.*
The use of DES products does not guarantee the successful passage of the CDCES exam. CBDCE does not endorse any preparatory or review materials for the CDCES exam, except for those published by CBDCE.
What are the treatment options for people with type 1 diabetes with a COVID infection hospitalized for Diabetes KetoAcidosis (DKA)?
The typical treatment for DKA is fluids coupled with an IV insulin drip. Given the frequent monitoring and ICU bed required for treatment of DKA with an insulin drip, there has been a renewed interest in treating DKA with subcutaneous or sub-q insulin.
But after doing some research, I discovered an excellent 2004 paper co-authored by Dr. Guillermo Umpierrez et al. on using Sub-Q Insulin to Treat DKA. After completing a study comparing treatment of DKA using sub-q insulin vs. insulin drip, the author’s conclude that sub-Q insulin treatment is a safe and effective alternative treatment to IV insulin in the management of people with mild or moderate DKA.
With a little more digging, I found 2 more recent papers that suggest considering Sub-Q insulin treatment as an option for mild or moderate DKA.
It is important to note that sub-Q insulin treatment for DKA is NOT recommended for patients with arterial hypotension, severe and complicated DKA, or with HHS.
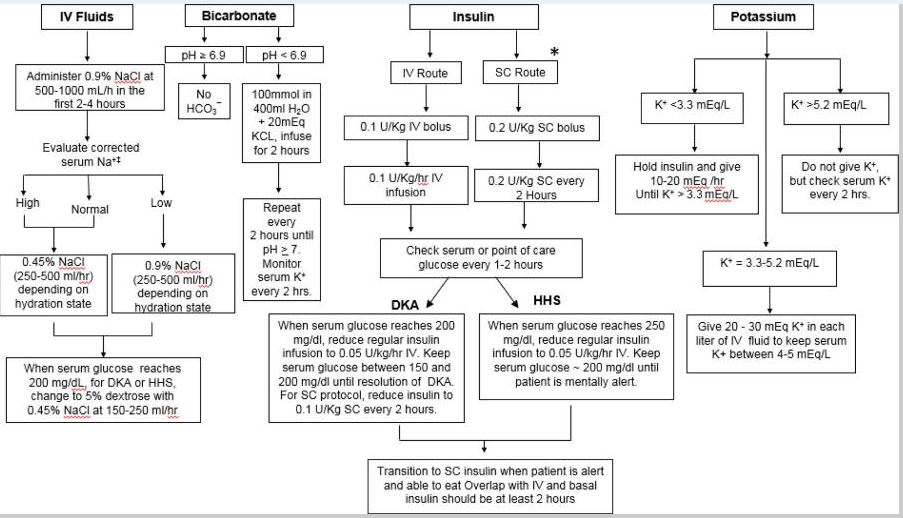
Insulins: Use either rapid acting lispro or aspart insulin.
1st Bolus: Starting dose is 0.1 or 0.2 or 0.3 units/kg of insulin (depending on initial blood glucose and clinical presentation)
Example: Pt weighs 100 kg, give 100kg x 0.1 – 0.2 – 0.3 units/kg of insulin = 10 or 20 or 30 units insulin sub-q bolus respectively.
Next Step – Sub-q insulin every 2 hours | Give 0.1 – 0.2 units of insulin /kg every 2 hours until blood glucose is less than 250.
Example: Pt weighs 100 kg, give 100kg x 0.1 – 0.2 units/kg of insulin = 10 or 20 units insulin sub-q bolus respectively every 2 hours.
Blood glucose less than 250 | Now give 1/2 the sub-q insulin dose every 2 hours. Calculate 0.05 to 0.1 units/kg every 2 hours until glucose at target and ketosis is resolved.
Example: Pt weighs 100 kg, give 100kg x 0.05 – 0.1 units/kg of insulin = 5 or 10 units insulin sub-q bolus respectively every 2 hours.
Using scheduled subcutaneous insulin allows for safe and effective treatment in the emergency room and step-down units without the need for ICU care. Umpierrez et al
Please see reference chart and articles below for more detailed information.
Of course, fluid and electrolyte status needs to be assessed before starting insulin.
If the K+ is less than 3.3, hold insulin and start with IV fluids (NS or LR) first with potassium replacement. Once the K is stable, start the insulin injection every 2 hours (see article and flow chart below).
Thank you for reading this article. Please share any feedback or your experiences using sub-q insulin for DKA. We always love to hear from you. You can email us at [email protected]
Eledrisi MS, Elzouki AN. Management of Diabetic Ketoacidosis in Adults: A Narrative Review. Saudi J Med Med Sci. 2020;8(3):165-173. doi:10.4103/sjmms.sjmms_478_19
Fayfman M, Pasquel FJ, Umpierrez GE. Management of Hyperglycemic Crises: Diabetic Ketoacidosis and Hyperglycemic Hyperosmolar State. Med Clin North Am. 2017;101(3):587-606. doi:10.1016/j.mcna.2016.12.011
Join Coach Beverly to learn more about causes and treatment of hyperglycemic crisis. (opens in a new tab)”>Find out more here>>

This course is included in: Level 2 – Standards of Care. Purchase this course individually for $19 or the entire bundle and save 70%.
This 60-minute course discusses common causes of hyperglycemia crises. Topics include hyperglycemia secondary to medications and insulin deprivation. The difference and similarities between Diabetes Ketoacidosis and Hyperosmolar Hyperglycemic Syndrome are also covered. Treatment strategies for all situations are included.
Topics include:
Sign up for Diabetes Blog Bytes – we post one daily Blog Byte from Monday to Friday. And of course, Tuesday is our Question of the Week. It’s Informative and FREE! Sign up below!
[yikes-mailchimp form=”1″]
Accreditation: Diabetes Education Services is an approved provider by the California Board of Registered Nursing, Provider 12640, and Commission on Dietetic Registration (CDR), Provider DI002. Since these programs are approved by the CDR it satisfies the CE requirements for the CDCES regardless of your profession.*
The use of DES products does not guarantee the successful passage of the CDCES exam. CBDCE does not endorse any preparatory or review materials for the CDCES exam, except for those published by CBDCE.

As health care professionals and Diabetes Specialists, how do we keep up to date with all the latest information on diabetes and COVID-19?
How do we prepare people with diabetes for the possibility of a COVID-19 infection and hospitalization?
To help, we have put together a list of free resources by category so you can easily access important and relevant information about COVID-19.
Plus, we have updated our Sick Days / COVID-19 and Diabetes Handout that we invite you to share with colleagues and people living with diabetes.
COVID-19, Sick days & Diabetes: Handout
Updated to reflect the latest CDC guidelines. Reviews sick day instruction for people with diabetes, plus COVID-19 specific information.
Article Library Sections

We have updated this content based on the ADA 2021 Standards of Care.
We are living longer and more people are getting diabetes. The American Diabetes Association has updated the Older Adults Standards, with special attention to considering a reduction of medication and insulin therapy intensity. The older population has unique issues and special needs that require consideration as we provide diabetes self-management education. This online course highlights key areas of assessment, intervention, and advocacy for older clients living with diabetes.
Topics include:
Join us live on December 23rd at 11:30 am (PST)
This course is included in: Level 2 – Standards of Care Intensive. Purchase this course individually for $29 or the entire bundle and save 70%.
Enroll in our entire Level 2 – Standards of Care Intensive to join us for the below for Live Webinar Updates. All courses air at 11:30 a.m. (PST)
All hours earned count toward your CDCES Accreditation Information
Sign up for Diabetes Blog Bytes – we post one daily Blog Byte from Monday to Friday. And of course, Tuesday is our Question of the Week. It’s Informative and FREE! Sign up below!
[yikes-mailchimp form=”1″]Accreditation: Diabetes Education Services is an approved provider by the California Board of Registered Nursing, Provider 12640, and Commission on Dietetic Registration (CDR), Provider DI002. Since these programs are approved by the CDR it satisfies the CE requirements for the CDCES regardless of your profession.*
The use of DES products does not guarantee the successful passage of the CDCES exam. CBDCE does not endorse any preparatory or review materials for the CDCES exam, except for those published by CBDCE.
Blood glucose levels provide an immediate snapshot of a person’s state of inflammation, with or without diabetes.
According to recent research findings, admission glucose is also an excellent predictor of COVID-19 related deaths and severity of illness.
Researchers in Spain retrospectively evaluated over 11,000 patients positive with COVID on admission in 109 hospitals throughout Spain. They also evaluated admission blood glucose levels and their findings were startling.
The researchers were also able to stratify the risk of death based on admissions glucose levels.
For all 11, 000 patients admitted with COVID in this study, the mortality rate was 20%.
For patients with admission glucose of 140 – 180, the mortality rate increased to 33%.
The mortality rate skyrocketed to 41% if admission glucose was 180 mg/dL or greater.
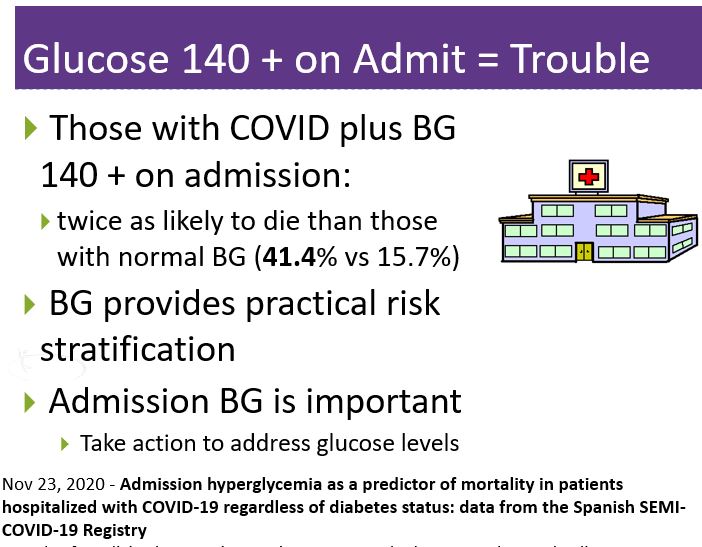
Read More Here Admission hyperglycemia as a predictor of mortality in patients hospitalized with COVID-19 regardless of diabetes status: data from the Spanish SEMI-COVID-19 Registry. November 2020
Annals of Medicine by Francisco Javier Carrasco-Sánchez, MD, PhD, and colleagues. Nov 23, 2020
Recorded & Ready for Viewing
Coach Beverly Thomassian, RN, MPH, CDCES, BC-ADM, has completely updated this critical presentation, to bring health care professionals up-to-date on the current state of COVID and its impact on diabetes care. She summarizes key information including critical teaching points and management strategies for people with diabetes who develop a COVID-19 infection.
Topics Include:
Join us to learn critical information about Diabetes and COVID Management

Instructor: Beverly Thomassian RN, MPH, CDCES, has been Board Certified in Advanced Diabetes Management for over 20 years. She is an Associate Clinical Professor at UCSF and Touro University and a nationally recognized diabetes expert.
Sign up for Diabetes Blog Bytes – we post one daily Blog Byte from Monday to Friday. And of course, Tuesday is our Question of the Week. It’s Informative and FREE! Sign up below!
[yikes-mailchimp form=”1″]
Accreditation: Diabetes Education Services is an approved provider by the California Board of Registered Nursing, Provider 12640, and Commission on Dietetic Registration (CDR), Provider DI002. Since these programs are approved by the CDR it satisfies the CE requirements for the CDCES regardless of your profession.*
The use of DES products does not guarantee the successful passage of the CDCES exam. CBDCE does not endorse any preparatory or review materials for the CDCES exam, except for those published by CBDCE.

Our November 17th Question of the week quizzed test takers on COVID-19 and diabetes. Less than half, 48% of respondents, chose the best answer, We thought that this was an important topic to discuss further, so we can pass on correct info to people living with diabetes.
Before we start though, if you don’t want any spoilers and haven’t tried the question yet, you can answer below: Answer Question
Question: COVID cases are surging throughout the United States. Providing the best care for people with diabetes is especially important during this crisis. Which of the following statements regarding diabetes and COVID is most accurate?
Answer Choices:
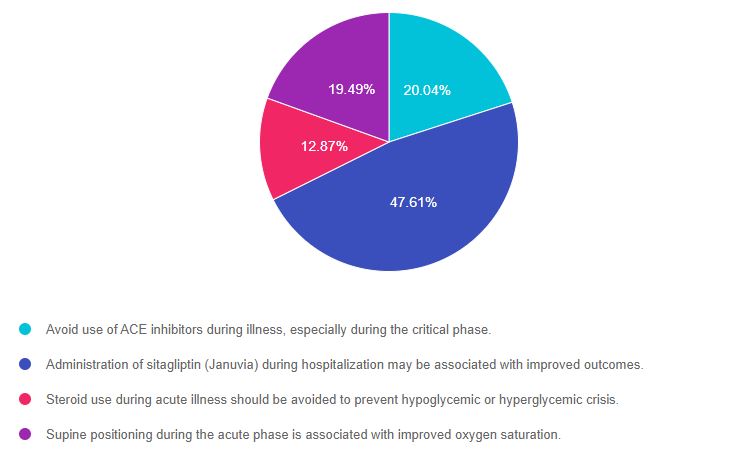
As shown above, the most common choice was option 2, the second most common answer was option 1, then option 4, and finally option 3.
If you are thinking about taking the certification exam, this practice test question will set you up for success. Test writers anticipate possible answers based on the details in the question. They will wave those “juicy answers” right under your nose. Your job is to weed through the particulars, pluck out the most important elements and choose the BEST answer.
Answer 1 is incorrect. 20.04% chose this answer. “Avoid use of ACE inhibitors during illness, especially during the critical phase.” Since the corona virus enters the body via ACE2 receptors, some early recommendations included stopping ACE inhibitors in those with COVID-19. However, scientists quickly discovered that stopping ACE inhibitors did NOT improve outcomes and that ACE inhibitors should be continued.
Answer 2 is correct. 47.61% of you chose this answer. “Administration of sitagliptin (Januvia) during hospitalization may be associated with improved outcomes.” YES. New research demonstrates that people with diabetes and COVID-19 started sitagliptin (Januvia) on hospital admission, experience dramatic decreases mortality and improved outcomes.
See our Blog Post – Sitagliptin Improves Outcomes here
Answer 3 is incorrect. About 12.87% of respondents chose this. “Steroid use during acute illness should be avoided to prevent hypoglycemic or hyperglycemic crisis.” It is true that steroids can contribute to hyperglycemia in people with diabetes. However, since steroids have been shown to be lifesaving for very ill people with COVID, with or without diabetes, research supports administering the steroid while managing resultant hyperglycemia with insulin therapy.
Finally, Answer 4 is incorrect. 19.49% chose this answer. “Supine positioning during the acute phase is associated with improved oxygen saturation.” Research has shown that “prone” positioning (laying on belly) can improve alveolar oxygenation and outcomes. More info here.
We hope you appreciate this week’s rationale! Thank you so much for taking the time to answer our Question of the Week and participate in this fun learning activity!

Purchase recording of our Live Webinar on December 2 | Earn 1.5 CE | $19
With the surge in new COVID cases, what is the essential information health care professionals and Diabetes Specialists need to navigate this overwhelming crisis?
What are the best practices to care for people with diabetes and COVID-19 in the outpatient and hospital setting?
Coach Beverly Thomassian, RN, MPH, CDCES, BC-ADM, has completely updated this critical presentation, to bring health care professionals up-to-date on the current state of COVID and its impact on diabetes care. She summarizes key information including critical teaching points and management strategies for people with diabetes who develop a COVID-19 infection.
Topics Include:
If you miss the live version, your registration guarantees access to the recorded version.
Join us to learn critical information about Diabetes and COVID Management

Instructor: Beverly Thomassian RN, MPH, CDCES, has been Board Certified in Advanced Diabetes Management for over 20 years. She is an Associate Clinical Professor at UCSF and Touro University and a nationally recognized diabetes expert.
Sign up for Diabetes Blog Bytes – we post one daily Blog Byte from Monday to Friday. And of course, Tuesday is our Question of the Week. It’s Informative and FREE! Sign up below!
[yikes-mailchimp form=”1″]Accreditation: Diabetes Education Services is an approved provider by the California Board of Registered Nursing, Provider 12640, and Commission on Dietetic Registration (CDR), Provider DI002. Since these programs are approved by the CDR it satisfies the CE requirements for the CDCES regardless of your profession.*
The use of DES products does not guarantee the successful passage of the CDCES exam. CBDCE does not endorse any preparatory or review materials for the CDCES exam, except for those published by CBDCE.
The winter and holiday seasons can be stressful and wear us down, especially during the pandemic. We tend to spend more time indoors. To help out, we have some suggestions that will not only help with stress management but can also boost your immunity.
Walking outside in nature and drinking in an “oxygen cocktail” feels good, but does it benefit our immunity?
You might be familiar with the term “Forest bathing” or shinrin-yoku. In Japanese, Shinrin means “forest,” and yoku means “bath.” Shinrin-yoku means bathing in a forest atmosphere or taking in the forest through our senses.
Research has demonstrated that trips to the forest can not only make us feel better by lowering muscle tension, boosting sleep, and reducing blood pressure. It turns out being in nature also enhances our immune systems by increasing the number and activity of our lympocytes and killer T cells.
When we walk among trees and plants, we breathe in airborne chemicals from plants called phytoncides.
Plants produce these chemicals to protect themselves from insects, bacterial and fungal infections. Phytoncides help plants fight disease.
These cells kill tumor and virus-infected cells in our bodies. In one study, increased NK activity from a 3-day, 2-night forest bathing trip lasted for more than 30 days.

According to Dr. Qing Li, author of the book, Forest Bathing, the key to unlocking the power of the forest is in the five senses:
To read more, click here.

The holiday season can also be stressful and throw us off our normal routine. This can compromise our sleep and our overall eating habits.
To help everyone feel their best during this holiday season, we have ten strategies for you and your patients. And even if you can’t do all ten, just pick one or a few that you feel you can commit to and succeed with most of the time.
We have created a 10 Steps to Survive the Holidays PDF – a handout that includes the info below to print and share with your friends, patients, and colleagues!
Recorded & Ready for Viewing
Coach Beverly Thomassian, RN, MPH, CDCES, BC-ADM, has completely updated this critical presentation, to bring health care professionals up-to-date on the current state of COVID and its impact on diabetes care. She summarizes key information including critical teaching points and management strategies for people with diabetes who develop a COVID-19 infection.
Topics Include:
Join us to learn critical information about Diabetes and COVID Management

Instructor: Beverly Thomassian RN, MPH, CDCES, has been Board Certified in Advanced Diabetes Management for over 20 years. She is an Associate Clinical Professor at UCSF and Touro University and a nationally recognized diabetes expert.

See Full Free Resource Catalog
Sign up for Diabetes Blog Bytes – we post one daily Blog Byte from Monday to Friday. And of course, Tuesday is our Question of the Week. It’s Informative and FREE! Sign up below!
[yikes-mailchimp form=”1″]Accreditation: Diabetes Education Services is an approved provider by the California Board of Registered Nursing, Provider 12640, and Commission on Dietetic Registration (CDR), Provider DI002. Since these programs are approved by the CDR it satisfies the CE requirements for the CDCES regardless of your profession.*
The use of DES products does not guarantee the successful passage of the CDCES exam. CBDCE does not endorse any preparatory or review materials for the CDCES exam, except for those published by CBDCE.
The COVID-19 Pandemic is taking a toll on people with diabetes.
Although people with diabetes are not more likely than the general population to be infected by COVID-19, they have much higher mortality rates than people without diabetes once infected with the virus.

The Corona Virus appears to have two portals of entry in humans.
In a recent study released in September in Diabetes Care, “Type 2 Diabetes and COVID-19: A Multicenter, Case-Control, Retrospective, Observational Study by Solerte et al”, the researchers demonstrated reduced mortality, improved clinical outcomes, and a greater number of hospital discharges for those started on sitagliptin on admission.
The COVID-19 virus seems to bind to the DPP-IV enzyme and the enzymatic activity of DPP4 causes overexpression of inflammatory cytokines, exaggerating the inflammatory response.
Since sitagliptin is a DPP-IV inhibitor, the researchers believe that the medication inhibited the virus’s ability to bind to DPP-IV. This had a net effect of decreasing the intense inflammatory response, often termed the “cytokine storm” associated with COVID-19 infections.
This Multicenter, Case-Control, Retrospective, Observational Study followed 338 consecutive patients with type 2 diabetes and COVID-19 admitted to Northern Italy hospitals.
Included in this study were 169 patients on sitagliptin and 169 on the standards of care. All patients had pneumonia and exhibited oxygen saturation <95% when breathing ambient air or when receiving oxygen support.
RESULTS: Treatment with sitagliptin at the time of hospitalization was associated with:
Sitagliptin contributed to a lowered risk and progression of acute respiratory complications for people with type 2 diabetes and COVID-19.
This research suggests that DPP-4 inhibitors can help decrease COVID-19-related immune overreaction in people with diabetes and dramatically improve outcomes.
Read article here >> Sitagliptin Treatment at the Time of Hospitalization was Associated with Reduced Mortality in Patients with Type 2 Diabetes and COVID-19: A Multicenter, Case-Control, Retrospective, Observational Study, Solerte et al. Diabetes Care 2020, Sept
Recorded & Ready for Viewing
Coach Beverly Thomassian, RN, MPH, CDCES, BC-ADM, has completely updated this critical presentation, to bring health care professionals up-to-date on the current state of COVID and its impact on diabetes care. She summarizes key information including critical teaching points and management strategies for people with diabetes who develop a COVID-19 infection.
Topics Include:
Join us to learn critical information about Diabetes and COVID Management

Instructor: Beverly Thomassian RN, MPH, CDCES, has been Board Certified in Advanced Diabetes Management for over 20 years. She is an Associate Clinical Professor at UCSF and Touro University and a nationally recognized diabetes expert.
Sign up for Diabetes Blog Bytes – we post one daily Blog Byte from Monday to Friday. And of course, Tuesday is our Question of the Week. It’s Informative and FREE! Sign up below!
[yikes-mailchimp form=”1″]
Accreditation: Diabetes Education Services is an approved provider by the California Board of Registered Nursing, Provider 12640, and Commission on Dietetic Registration (CDR), Provider DI002. Since these programs are approved by the CDR it satisfies the CE requirements for the CDCES regardless of your profession.*
The use of DES products does not guarantee the successful passage of the CDCES exam. CBDCE does not endorse any preparatory or review materials for the CDCES exam, except for those published by CBDCE.