Impacts of Healthcare Inequities & How We Can Change Them
As Diabetes Education Specialists and advocates, we see first-hand how healthcare inequalities impact the health of under-resourced communities.
Just as diabetes is systemic, affecting the entire body, so are the disparities in our public and private healthcare systems.
This is not only a result of public policies, healthcare education, medical racism, and medical classism, but also access to nutritious whole foods, stable housing, insurance coverage, and even enough time in the day to focus on one’s health.
Under the COVID-19 pandemic, these disparities have become even more apparent.
“Black and Latino patients are two to three times as likely as white patients to be diagnosed with COVID-19, and more than four times as likely to be hospitalized for it. Black patients are more than twice as likely to die from the virus. They also die from it at younger ages“ wrote Ezekiel J. Emanuel, Oncologist, bioethicist, and vice provost of the University of Pennsylvania and Risa Lavizzo-Mourey, Professor at the University of Pennsylvania for The Atlantic.
Acknowledging these perforations of care is an important first step towards a more inclusive healthcare system. This reparative practice can result in more positive outcomes and improve the quality of life for many.
Insurance Coverage & Reimbursement Rates
Equal access to healthcare coverage is key.
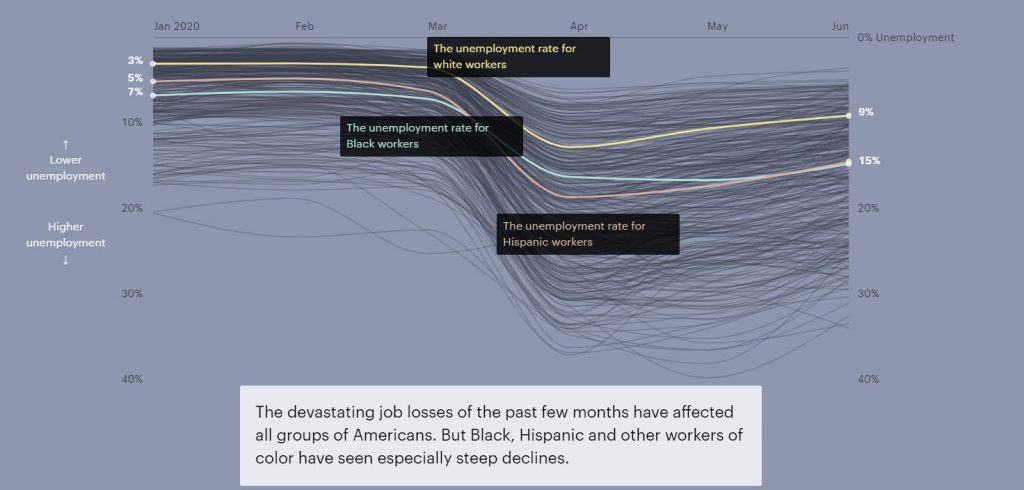
The economic impacts of the pandemic have widened the gap in insurance coverage. Around 12 million people living in the U.S. lost employer insurance due to the pandemic, with higher unemployment rates for Black and Latino workers (see above graph).
Since the implementation of the Affordable Care Act (ACA) the number of uninsured individuals and families was reduced. However, 15 states opted out of the widening of programs like Medi-Caid under ACA.
For those insured under Medi-Caid, there is still the hurdle of finding a provider that accepts their insurance. This is because many healthcare professionals do not accept Medi-Caid due to low reimbursement rates.
Initially, the ACA increased rates for providers who accepted Medicare and Medi-caid. But they have decreased over time and with that decrease, the number of doctors accepting or even scheduling individuals with Medi-Caid decreased, as well.
“A 2014–15 survey showed that only 68 percent of family-practice physicians accepted new Medicaid patients, while 91 percent accepted those with private insurance,” Ezekiel J. Emanuel and Risa Lavizzo-Mourey.
In addition to raising overall fees for service, implementing a system in which healthcare providers are reimbursed based on health outcomes can be a way to hold us accountable to provide a high level of care, despite factors such as race, gender, sexuality, or class.
Unlearning Medical Biases & Increasing Representation
Medical discrimination is pervasive.
A study conducted earlier in the pandemic found “that doctors were less likely to refer symptomatic Black patients for testing than they were to refer white ones.”
It has also been studied that white medical students and residents rate pain lower for Black people who are experiencing similar symptoms to white people. This bias impacts their care recommendations and the study found lower accuracy of treatment plans for the Black person’s case example.
Educating ourselves on the history of medical racism and classism while engaging in implicit bias training can help us unlearn these inaccurate assumptions.
Representation matters for Healthcare Providers.
Lack of representation often stems from a multitude of factors, such as discriminatory admissions or hiring practices.
An experiment conducted in Oakland found that involving Black doctors in treatment plans reduced the cardiovascular mortality gap by 19% for Black and white men.
Another example of why representation matters are reflected in how commonly medical texts only show white skin tones. Because of this, Malone Mukwende, a 20-year-old medical student is working on a book to show what symptoms look like on darker skin.
Systemic changes begin with each of us.
Educating ourselves on discriminatory medical practices both for healthcare professionals and the people living with diabetes with whom we work with is a great first step to moving towards a more inclusive medical system.
Written by Bryanna, our Director of Operations & Customer Happiness
Read more from The Atlantic article by clicking here. For more information on racial disparities in the treatment of pain click here. For Malone Mukwende’s story click here.
Sign up for Diabetes Blog Bytes – we post one daily Blog Byte from Monday to Friday. And of course, Tuesday is our Question of the Week. It’s Informative and FREE! Sign up below!
[yikes-mailchimp form=”1″]
Accreditation: Diabetes Education Services is an approved provider by the California Board of Registered Nursing, Provider 12640, and Commission on Dietetic Registration (CDR), Provider DI002. Since these programs are approved by the CDR it satisfies the CE requirements for the CDCES regardless of your profession.*
The use of DES products does not guarantee the successful passage of the CDCES exam. CBDCE does not endorse any preparatory or review materials for the CDCES exam, except for those published by CBDCE.
Question of the Week | Sept 29, 2020

LT, a 59-year old with type 2 diabetes presents to the hospital in a hyperglycemic crisis. LT has a history of hypertension, peripheral vascular disease and smokes a pack per day. LT states they have been taking 1000mg metformin BID and 10 units basaglar every night as usual. LT tells you they are stressed out and concerned about a foot sore that doesn’t seem to be getting better. LT is trying to stay home and avoid other people, to prevent getting COVID. LT’s A1C is 8.8%.
What is the most likely cause of this sudden hyperglycemia?
- Stress eating due to isolation
- Untreated infection
- Rationing medications due to financial hardship
- Insulin resistance secondary to cigarette smoking
Click here to test your knowledge!
The New Art and Science of Diabetes Care and Education Desk Reference – 5th Edition| $249
We are so excited that the 5th edition The Art and Science of Diabetes Care and Education is finally here!
This specialist’s one-volume, go-to resource for the core knowledge and skills for providing person-centered care and education to persons with diabetes and related chronic conditions. This is a core resource for those who are studying for the Certified Diabetes Care and Education Specialist® (CDCES) exam.
Updates:
- Two new chapters addressing multiple daily injections (MDI), continuous subcutaneous insulin infusion (CSII), pump therapy, continuous glucose monitoring (CGM) and intensifying therapy, pattern management, and data analysis.
- Revised AADE7 Self-Care Behaviors®, with its recognition of the impact the emotional burden of diabetes on metabolic and quality of life outcomes.
- Highlights obesity management, including the 3-step algorithm for care of overweight and obese people with diabetes.
- Expanded coverage of motivational interviewing (MI).
- Major rewrites of the kidney disease and diabetic neuropathies chapters.
2020 Boot Camp Live Stream Webinar Schedule with Coach Beverly
All courses air at 11:30 a.m. (PST)
- Diabetes – Not Just Hyperglycemia | Recorded & Ready for Viewing.
- ADA Standards of Care | Recorded & Ready for Viewing.
- Insulin Therapy – From Basal/Bolus to Pattern Management | Sept 30
- Insulin Intensive – Monitoring, Sick Days, Lower Extremities | Oct 7
- Meds for Type 2 | Oct 14
- Exercise and Preventing Microvascular Complications | Oct 21
- Coping & Behavior Change | Oct 28
- “The Big Finish” Test Taking Boot Camp | Nov 4
Sign up for Diabetes Blog Bytes – we post one daily Blog Byte from Monday to Friday. And of course, Tuesday is our Question of the Week. It’s Informative and FREE! Sign up below!
[yikes-mailchimp form=”1″]Accreditation: Diabetes Education Services is an approved provider by the California Board of Registered Nursing, Provider 12640, and Commission on Dietetic Registration (CDR), Provider DI002. Since these programs are approved by the CDR it satisfies the CE requirements for the CDCES regardless of your profession.*
The use of DES products does not guarantee the successful passage of the CDCES exam. CBDCE does not endorse any preparatory or review materials for the CDCES exam, except for those published by CBDCE.
Coach Bev’s Diabetes Cheat Sheets
We know that a great resource page full of accurate and helpful cheat sheets can save busy diabetes specialists time and energy.
That’s why we have put together our entire list of cheat sheets so you can access them with ease.
These sheets and cards include information to study for certification exams and to use in your clinical setting. Plus, we have included teaching sheets for people with diabetes.
Our Summer 2020 Boot Camp begins September 16th!

In each webinar, either Coach Beverly, Dr. Isaacs, or Ms. Armstrong, highlight the critical content of each topic area, so you can focus your study time most efficiently. They also launch multiple poll questions to help participants focus on key concepts and assess their knowledge while learning the best test-taking strategies.
2020 Boot Camp Live Stream Webinar Schedule with Coach Beverly
All courses air at 11:30 a.m. (PST)
- Diabetes – Not Just Hyperglycemia | Sept 16
- ADA Standards of Care | Sept 23
- Insulin Therapy – From Basal/Bolus to Pattern Management | Sept 30
- Insulin Intensive – Monitoring, Sick Days, Lower Extremities | Oct 7
- Meds for Type 2 | Oct 14
- Exercise and Preventing Microvascular Complications | Oct 21
- Coping & Behavior Change | Oct 28
- “The Big Finish” Test Taking Boot Camp | Nov 4
Can’t make it live?
No worries! All video presentations and podcasts will be available now on-demand.
Sign up for Diabetes Blog Bytes – we post one daily Blog Byte from Monday to Friday. And of course, Tuesday is our Question of the Week. It’s Informative and FREE! Sign up below!
[yikes-mailchimp form=”1″]Accreditation: Diabetes Education Services is an approved provider by the California Board of Registered Nursing, Provider 12640, and Commission on Dietetic Registration (CDR), Provider DI002. Since these programs are approved by the CDR it satisfies the CE requirements for the CDCES regardless of your profession.*
The use of DES products does not guarantee the successful passage of the CDCES exam. CBDCE does not endorse any preparatory or review materials for the CDCES exam, except for those published by CBDCE.
[yikes-mailchimp form=”1″]Vitamin D, Diabetes, & COVID-19 | Tech Thursday

Interesting findings that explore the relationship between Vitamin D levels and COVID-19 outcomes are being released.
In an article by WedMD, there have been several international studies that evaluate Vitamin D levels in people infected with COVID-19.
None of these studies indicate definitively if higher levels of Vitamin D reduce the risk of contracting or becoming severely ill with COVID-19. Though, they’ve noticed that the “sickest” people with COVID-19 had low levels of Vitamin D.
Several studies conducted across different countries indicate that a healthy level of Vitamin D might strengthen our immune system and reduce our vulnerability to disease.
Vitamin D is so important for our bones, muscles, and a nutrient our immune systems need for optimal health. An adequate blood level of Vitamin D is between 20 nanograms/milliliter to 50 mg/ml. A simple but slightly costly blood test can measure one’s level of this vitamin.
People living with diabetes (type 1 & type 2) often have lower levels of Vitamin D. Vitamin D deficiency can manifest as fatigue, depression, muscle and bone pain, and decreased overall health.
Boosting Vitamin D Levels
Lifestyle changes can be used to treat low Vitamin D levels; eating healthy foods like eggs, mushrooms, fresh fish, and getting outside in sunlight, can increase our Vitamin D levels. As a supplement, Vitamin D3 or cholecalciferol is recommended at a dose of 400-1000 IU /day.
Vitamin D is made by the body when the skin is exposed to sunlight. Often people in the Northern Hemisphere with less sun exposure have lower levels of Vitamin D. Regular sun exposure can help increase Vitamin D levels, although supplementation seems to be more effective.
In addition, improving access to healthy foods needs to be a priority for all people, but especially vulnerable populations and those with diabetes.
For more information, read the WebMD article here. We also recommend you read Vitamin D and Type 1 Diabetes: What the Research Says & Higher vitamin D levels linked to lower risk for diabetes. Click here for NIH Vita D Info page.
Update
Healio has released more information on this topic that you can find on their recent article, “Researchers caution against ‘misinformation’ on vitamin D during COVID-19 pandemic.”
Written by Catherine Cullinane RN, CDCES, our resident Tech Thursday Content Writer
Sign up for Diabetes Blog Bytes – we post one daily Blog Byte from Monday to Friday. And of course, Tuesday is our Question of the Week. It’s Informative and FREE! Sign up below!
[yikes-mailchimp form=”1″]Accreditation: Diabetes Education Services is an approved provider by the California Board of Registered Nursing, Provider 12640, and Commission on Dietetic Registration (CDR), Provider DI002. Since these programs are approved by the CDR it satisfies the CE requirements for the CDCES regardless of your profession.*
The use of DES products does not guarantee the successful passage of the CDCES exam. CBDCE does not endorse any preparatory or review materials for the CDCES exam, except for those published by CBDCE.
Update: DPP-4 Inhibitor Not Associated with Improved Outcomes in COVID-19

In a recent post, we shared endocrinologist Gianluca Iacobellis’, MD, Ph.D. suggesting that DPP-4 inhibitors could help decrease COVID-19-related immune overreaction in people with diabetes.
However, according to Daniel Drucker, MD, Ph.D., there is “insufficient evidence” that DPP-IVs decrease the immune response during COVID-19 infections.
Daniel Drucker, MD, Ph.D., professor of medicine at the Lunenfeld Tanenbaum Research Institute of Mount Sinai Hospital and the University of Toronto and expert in the field, summarized that DPP-4 inhibitors and GLP-1 receptor agonists have not been associated with improved outcomes in critically ill individuals with diabetes and a COVID- 19 infection.
Insulin is the glucose-lowering therapy of choice for acute coronavirus-related illness in hospital.
Daniel Drucker, MD, Ph.D
Dr. Drucker states that available evidence does not currently support clinically meaningful alterations in markers of immune function after administration of DPP-IV inhibitors in humans with or without type 2 diabetes.
This is important news as it clears up medication misconceptions and further highlights the importance of administering insulin for people with type 2 diabetes and active COVID-19 infection.
Considering the fact that people with type 2 diabetes have a higher chance of developing complications from COVID-19 than people without diabetes, it is critical to use the most effective method of treatment.
Read More
- For more information on DPP4-Inhibitors, click here.
- To read our previous article about DPP-4 Inhibitors, click here.
Update for CMS Guidelines for CGM Coverage | Tech Thursday

Last week we posted a blog titled “CMS Updates For CGM Coverage,” which on the surface seemed like very exciting, impactful changes on CMS regulations for CGM coverage during the COVID-19 pandemic.
After sharing this post, members of our community let us know that although CMS guidelines have been relaxed in writing, this hasn’t translated into better access on the ground.
What do these changes actually mean?
To learn more we dove into the interim final rule with comment period (IFC) that was released by the Department of Health & Human Services – Centers for Medicare & Medicaid Services.
In the March 31st COVID-19 IFC, we finalized on an interim basis that we will not enforce the clinical indications for coverage across respiratory, home anticoagulation management, and infusion pump NCDs (Nation Coverage Determinations) and LCDs (Local Coverage Determinations) (including articles) allowing for more flexibility for practitioners to care for their patients. This enforcement discretion will only apply during the PHE for the COVID-19 pandemic.
The language in the IFC is vague and ambiguous regarding what it means to have less stringent and “more flexible” requirements of obtaining a CGM in the time of the COVID-19 for people with diabetes. Though we have found a few highlights from the document based on feedback by our community on what is unclear.
The Highlights
- These changes are only applicable to those who are COVID-19 positive and living with diabetes.
- The type of diabetes one has is no longer relevant in coverage determinations.
- These guidelines do not automatically expand to Medicaid coverage. For more details on Medicaid coverage, contact your local state.
In this IFC, we are finalizing on an interim basis that we will not enforce the clinical indications for therapeutic continuous glucose monitors in LCDs. For example, we will not enforce the current clinical indications restricting the type of diabetes that a beneficiary must have or relating to the demonstrated need for frequent blood glucose testing in order to permit COVID-19 infected patients with diabetes to receive a Medicare-covered therapeutic continuous glucose monitor.
Overall, there is still much to learn about these changes as they apply to real-life situations. This is an unprecedented time for all of us and there is a lot of unknowing. We hope as things develop to keep you informed.
To read the full IFC click here. For more information about Medicaid Guidelines, click here.
If you have any more information on these changes, please click here to visit our survey to update us.
Written by Catherine Cullinane RN, CDCES, our resident Tech Thursday Content Writer
Sign up for Diabetes Blog Bytes – we post one daily Blog Byte from Monday to Friday. And of course, Tuesday is our Question of the Week. It’s Informative and FREE! Sign up below!
[yikes-mailchimp form=”1″]Accreditation: Diabetes Education Services is an approved provider by the California Board of Registered Nursing, Provider 12640, and Commission on Dietetic Registration (CDR), Provider DI002. Since these programs are approved by the CDR it satisfies the CE requirements for the CDCES regardless of your profession.*
The use of DES products does not guarantee the successful passage of the CDCES exam. CBDCE does not endorse any preparatory or review materials for the CDCES exam, except for those published by CBDCE.
Telehealth and DSMT | Latest Updates from CMS
As Diabetes Specialists, we want to ensure the safety of patients and colleagues, while providing diabetes care to those who may be the most vulnerable and isolated during this pandemic.
According to the CARES Act, Diabetes Self-Management Training (DSMT) can be provided to patients via telehealth during the pandemic. Though the original regulations had many gaps.
Previously, the CARES Act required that telehealth visits must include both audio and video, while many hospital outpatient clinics were running into billing barriers. In addition, under the original guidelines, RNs and Pharmacists were not included in the approved list of telehealth DSMT Providers.
See: ADCES Summary Sheet of DSMT and Telehealth FAQ for more information.
Though as of April 23, 2020 the guidelines have been updated.
Good News – these updates to the CARES Act now expand blanket waivers under the 1135 waiver.
For any of the information below, please check with your compliance team for clarification and share the important resource links below with your billing department.
How do CMS Updates Affect Our Ability to Provide DSMT Training?
DSMT Can Now be Audio-Only
DSMT services may be billed for audio-only, but only if the video is not available or possible. Make sure to document the mode of instruction and the rationale if using audio-only.
See: COVID-19 Emergency Declaration Waiver for more information.
Can RNs & Pharmacists Now Provide Telehealth and Bill for DSMT?
The ADA and ADCES have been working hard to decipher the language and intent in the updated guidelines. It seems that RN and Pharmacists are now included based on an assessment of the wording in the new documents. CMS continues to expand the definition of providers eligible to furnish telehealth services during the COVID-19 public health emergency.
As DSMT programs bill as an entity, rather than at the individual provider level, the American Diabetes Association is seeking confirmation that DSMT programs that are eligible through Medicare Part B, are considered distant site practitioners approved to furnish telehealth services.
See: Blanket Waivers for HealthCare Providers Fact Sheet for more information.
Hospital-Based Programs Can Bill for Telehealth DSMT on the UB-04 (Medicare Claims) Form
Hospitals may now bill for education and management services (i.e. DSMT) as if they were furnished in the hospital and consistent with any specific requirements for billing Medicare in general, including any relevant modifications in effect during the COVID-19 PHE.
In summary:
- DSMT services can be provided in the hospital outpatient setting remotely to a patient in their home.
- The patient’s home can serve as a temporary provider-based department of the hospital (CMS’ Hospitals Without Walls initiative).
- If you previously billed using the UB-04, continue to bill the same way.
- The patient must be a registered outpatient of a hospital.
- DSMT and scope of practice requirements must be met.
See: CMS Hospitals Without Walls Initiative for more information.
Important to note: Please consult with your organization’s billing department and compliance team if you have questions.
Sources and Links
- CMS Press Release Summarizing April 30 Guidance.
- Hospitals CMS Flexibilities to Fight COVID Fact Sheet.
- Blanket Waivers for HealthCare Providers Fact Sheet
- Telehealth Information: List of billing codes are available here.
Sign up for Diabetes Blog Bytes – we post one daily Blog Byte from Monday to Friday. And of course, Tuesday is our Question of the Week. It’s Informative and FREE! Sign up below!
[yikes-mailchimp form=”1″]Accreditation: Diabetes Education Services is an approved provider by the California Board of Registered Nursing, Provider 12640, and Commission on Dietetic Registration (CDR), Provider DI002. Since these programs are approved by the CDR it satisfies the CE requirements for the CDCES regardless of your profession.*
The use of DES products does not guarantee the successful passage of the CDCES exam. CBDCE does not endorse any preparatory or review materials for the CDCES exam, except for those published by CBDCE.
May Newsletter | Insulin Savings, Telehealth Updates, and Salivary Glucose Testing
Click here to read our entire May Newsletter

As a Diabetes Nurse Specialist in a local clinic, I am providing telehealth once a week. During these visits, I am checking in with people about their food and medications.
Do you have enough food and insulin to last? Most of them answer, “yes, for now”.
Many of them may run out of insulin and supplies in the near future, some as a result of the costs that make essential medications in-affordable. If this is the case, what can we offer them?
We are excited to thank our guest contributor and Diabetes Educator of the Year, Dr. Diana Isaacs, who has provided us with helpful information and a multitude of resources for people in need of low-cost insulin.
In light of the COVID-19 emergency, the Centers for Medicare & Medicaid Services (CMS), has expanded opportunities to provide remote care to people with diabetes. We have highlighted some recent updates and provided links to helpful resources for your billing team.
Lastly, we are looking towards the future with salivary glucose testing and insights into a past Question of the Week.
I am grateful to be a part of this amazing community of diabetes specialists. Thank you for your care, concern and advocacy.
Be well! Coach Beverly
Click here to read our entire May Newsletter
Virtual Course Insulin Therapy, Pumps, & CGM + CV Risk Reduction Strategies
Earn 4.0 CEs | $69
Join Diana Isaacs, PharmD, BCPS, BC-ADM, BCACP, CDCES, and ADCES 2020 Diabetes Educator of the year as she reviews these important topics. As Diabetes Specialists, we are tasked with taking a leadership role in technology and cardiovascular risk reduction. Dr. Isaacs will address these topics with clinical insight and expert knowledge during these two virtual courses.
Session 1 | CV Risk Management with Pharmacology and Intensive Insulin Therapy | Recorded & Ready for Viewing!
Session 2 | Continuous Glucose Monitoring and Insulin Pump Therapy | Recorded & Ready for Viewing!
Objectives:
- Describe critical teaching content before starting insulin pump therapy.
- Describe appropriate candidates for insulin pump therapy.
- Discuss strategies to determine and fine-tune insulin pump basal rates.
- Discuss how to determine and fine-tune bolus rates including coverage for carbs and hyperglycemia.
- State important safety measures to prevent hyperglycemic crises.
- List inpatient considerations for insulin pump therapy and CGMs.
- Discuss features of available professional and personal CGMs and insulin pumps.
- Describe CV risk factors associated with diabetes and future event prediction.
- List different pharmacologic approaches to mitigate CV events.
$69 | Earn 4 CEs
These sessions are also included in our Virtual Conference.
Sign up for Diabetes Blog Bytes – we post one daily Blog Byte from Monday to Friday. And of course, Tuesday is our Question of the Week. It’s Informative and FREE! Sign up below!
[yikes-mailchimp form=”1″]Accreditation: Diabetes Education Services is an approved provider by the California Board of Registered Nursing, Provider 12640, and Commission on Dietetic Registration (CDR), Provider DI002. Since these programs are approved by the CDR it satisfies the CE requirements for the CDCES regardless of your profession.*
The use of DES products does not guarantee the successful passage of the CDCES exam. CBDCE does not endorse any preparatory or review materials for the CDCES exam, except for those published by CBDCE.








