COVID-19 & Diabetes Resource Page | Free Resource Friday

For this week’s Free Resource Friday, we want to share with you our new COVID-19 & Diabetes Resource Page!
Over the past weeks, we have been collecting resources to learn more about COVID-19 and how it affects people living with diabetes.
We have decided to gather all of these resources together into one page to share with you.
This page includes webinars, ADA & ADCES COVID-19 resource hubs, handouts, mental wellness resources, and much more!
Sign up for Diabetes Blog Bytes – we post one daily Blog Byte from Monday to Friday. And of course, Tuesday is our Question of the Week. It’s Informative and FREE! Sign up below!
[yikes-mailchimp form=”1″]COVID-19 and Diabetes: CGMs in Hospital Improve Care | Tech Thursday
What does it feel like to be ill with COVID-19 as a person with diabetes? Much of the novel virus COVID-19 is still a mystery that we learn more about every day.

Through the stories of those who have contracted COVID-19, we know that the impacts vary. Symptoms can appear mild with a slight fever and some coughing, like Andrew O’Dwyer from the UK experienced.
While for others symptoms can be more severe, like how a secondary-school teacher living with diabetes had. She had a much longer list of symptoms including difficulty breathing, dizziness, dehydration, and vomiting.
Though even with her more severe symptoms, she struggled with whether she should go to the hospital or not.
“I’m unsure whether to go to the hospital. I feel as though I’ll be wasting valuable resources and I may be an infection risk to vulnerable patients.
As many medical systems are overwhelmed and resources continue to be limited, it’s important to think of ways to reduce the risk of transmission so individuals can get the care they need. Because despite this wide range of impact, COVID-19 continues to emerge with very severe complications for people with or without diabetes.
Reduce the Risk: Glucose control is key!
For people with diabetes who are treating COVID-19, glucose control is key! Keeping BG levels as close to the target range as possible can help reduce the inflammatory response, caused by hyperglycemia. Following the basic guidelines of sick day management will assist the type 1 person who might be diagnosed with COVID-19.
To minimize the risk of transmission, hospitals are starting to use CGM’s for glucose checks in ICUs and in COVID-19 units.
“We knew we needed to get creative” states Carol Levy, MD, Clinical Director of the Mount Sinai Diabetes Center, while discussing “a new initiative to utilize CGM for critically ill patients with COVID-19 to reduce patient-provider contact, conserve PPE, and reduce risks for virus transmission.”
For more information, please see our Emergency Preparedness Blog Post.
There is an incredible amount of information regarding COVID-19 and diabetes. These articles show a glimmer of hope for all people with diabetes that might develop COVID-19.
Written by Catherine Cullinane RN, CDCES, our resident Tech Thursday Content Writer
To read more Mount Sinai’s efforts click here. Click here for For Arthur’s full story, or for the secondary school’s story click here.
*From ADA Treatment & Care Fact Sheet, “People with diabetes are not more likely to get COVID-19 than the general population. The problem people with diabetes face is primarily a problem of worse outcomes, not a greater chance of contracting the virus. In China, where most cases have occurred so far, people with diabetes had much higher rates of serious complications than people without diabetes.” To help friends and family keep safe, here is an excellent handout on Keeping Safe and Home and in the Workplace by the World Health Organization.
COVID-19 & Diabetes| What Health Care Professionals Need to Know – FREE Webinar
As health care professionals and Diabetes Specialists, how do we prepare people with diabetes for the possibility of a COVID-19 infection and hospitalization?
What are best practices to care for people with diabetes and COVID-19 in the outpatient and hospital setting?
Updates:
The Telehealth guidelines for providing DSMT have been updated since the streaming of this webinar. Please see this blog, Telehealth and DSMT | Latest Updates from CMS, for updated information.
Webinar Viewing Options:
Coach Beverly Thomassian, RN, MPH, CDCES, BC-ADM, has summarized key information including critical teaching points and management strategies for people with diabetes who develop a COVID-19 infection.
In addition to the webinar, we will provide attendees with useful resources to provide care and education to colleagues and community members alike.
Topics:
- Discuss the relationship between social determinants of health, diabetes, and COVID-19.
- List how people with type 1 and type 2 diabetes can prevent and prepare for a COVID-19 infection.
- Describe how the COVID-19 virus can cause serious illness in people with diabetes and underlying health conditions
- State management strategies for people with diabetes and COVID in the inpatient and outpatient settings.
- Discuss the latest regulations regarding DSMT and Telehealth
Updates:
The Telehealth guidelines for providing DSMT have been updated since the streaming of this webinar. Please see this blog, Telehealth and DSMT | Latest Updates from CMS, for updated information.
Instructor: Beverly Thomassian RN, MPH, CDCES, has been Board Certified in Advanced Diabetes Management for over 20 years. She is an Associate Clinical Professor at UCSF, a working educator and a nationally recognized diabetes expert.
Can’t make it live? Your webinar registration means you receive a link to the recorded version within hours of airing.
Other FREE Resources we offer
See a complete listing of our upcoming FREE Webinars
Sign up for Diabetes Blog Bytes – we post one daily Blog Byte from Monday to Friday. And of course, Tuesday is our Question of the Week. It’s Informative and FREE! Sign up below!
[yikes-mailchimp form=”1″]DIY Cloth Face-Masks | Mindful Monday
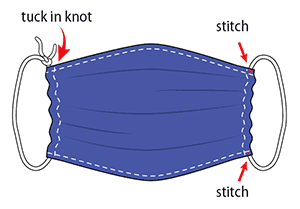
To help prevent the spread of COVID-19, the CDC recommends everyone wears a cloth face-mask when in public.
In addition to washing our hands frequently and maintaining a 6ft. distance from others, cloth masks can help in situations where social distancing is more difficult, such as the grocery store.
Cloth face-masks can easily be made at home with a scarf, bandana, hand towel, or t-shirt, just be sure to wash them frequently. Here are a few tips for making your mask:
Click here to read more.
Sign up for Diabetes Blog Bytes – we post one daily Blog Byte from Monday to Friday. Tuesday is our Question of the Week. It’s Informative and FREE! Sign up below!
[yikes-mailchimp form=”1″]April Newsletter | COVID-19 & Best Diabetes Care
Click here to read our entire April Newsletter

At a local hospital, a person in their mid-40s, with type 2 diabetes was admitted for treatment of COVID-19 and Diabetes Ketoacidosis (DKA). An insulin drip was started and their SGLT-2 Inhibitor was stopped. Why are people with type 2 and COVID-19 going into DKA and how is this impacting outcomes?
A person with type 1 diabetes calls into a rural health clinic and says they are running a temperature, having difficulty breathing and can’t get their blood sugars below 300. The diabetes specialist instructs them to go to the hospital. What supplies should they take in case they are admitted to the hospital?
How do we help prepare people with diabetes for the possibility of hospitalization and what are best practices to care for people with diabetes and COVID-19 in the hospital setting?
What instruction do we provide for people with diabetes if they get sick and are wondering if they need to go to the hospital?
In this newsletter, our goal is to answer these questions based on the opinions of experts in the field and the best information to date.
In addition, we are excited to share information on drone delivery of insulin, mask making and the opportunity to celebrate the AADE (ADCES) Educator of the Year, Dr. Diana Isaacs.
Lastly, please let CMS (Medicare) know that RNs and Pharmacists need to be considered as providers of DSME telehealth services. Now, more than ever, we need all hands on deck.
Thank you everyone. Take extra good care of yourselves.
Beverly
Click here to read our entire April Newsletter
Can DPP-4 Inhibitors Help Treat COVID-19 in People with Diabetes?
Hopeful news.

DPP-4 inhibitors may contribute to a lowered risk and progression of acute respiratory complications for people with type 2 diabetes and COVID-19.
According to commentary in Diabetes Research and Clinical Practice, Endocrinologist Gianluca Iacobellis, MD, Ph.D. suggests that DPP-4 inhibitors could help decrease COVID-19-related immune overreaction in people with diabetes. This immune system calming is due to DPP-IVs anti-inflammatory effects.
All told, DPP-4 “may represent a potential target for preventing and reducing the risk and the progression of the acute respiratory complications that Type 2 diabetes may add to the COVID-19 infection,” Iacobellis wrote in his article.
Based on data from the Chinese city of Wuhan and Italy, people with type 2 diabetes are at higher risk of serious disease in the current pandemic. The data indicates that people with diabetes have accounted for a large proportion of intensive care admission and deaths related to COVID-19.
“The body is overreacting with this inflammatory response to the virus,” Dr. Iacobellis said in a statement. “This could be partially mediated by DPP-4. The virus binds to the enzyme and the enzymatic activity of DPP4 overexpresses inflammatory cytokines, exaggerating the inflammatory response.”
Read more FierceBiotech
Diabetes 2020 – Virtual Conference!
Now with COVID-19 Update
7.5 CEs | $89 | Starts April 23
The COVID Pandemic is taking a toll on people with diabetes. What is the critical information Diabetes Care and Education Specialists need as we navigate this pandemic? How can take a leadership role in providing sound recommendations while helping to manage the full range of diabetes issues, including hypertension, hyperlipidemia, and cardiovascular risk reduction?

Coach Beverly has created this four-session virtual course so that participants can delve deep into the topics that are most pressing for diabetes care now and in the future. We will focus on improving population health and then drill down to individual intervention through case studies. We will discuss implementing cardiovascular risk screening and treatment in the clinical setting and more!
Course Schedule
Session 1 – Getting to the Heart of Care – 1.5 CEs – Airs April 23rd
- Our role as Diabetes Care and Education Specialists
- Diabetes and the COVID Pandemic
- ADA and 2020 Medication Management Algorithm –
Session 2 – Cardiovascular Risk Reduction Strategies – 1.5 CEs – Airs April 24th
- ADA and AACE Guidelines for CV Risk Reduction
- Implement Risk Reduction Strategies
- Addressing Hypertension, Lipids and Weight – A Case Study Approach
Session 3 – Lower Extremity Assessment and Intervention – 1.5 CEs – Airs April 28th
- Peripheral Arterial Disease vs Vascular Disease
- Lower extremity assessment techniques
- Prevention strategies and education
Session 4 – Making meaningful Connections and a Vision for the Future – 1.5 CEs – Airs April 30th
- Adverse Child Experiences – ACE and Impact of Diabetes and other Health Outcomes
- Improving health- From individuals to populations
Sign up for Diabetes Blog Bytes – we post one daily Blog Byte from Monday to Friday. Tuesday is our Question of the Week. It’s Informative and FREE! Sign up below!
[yikes-mailchimp form=”1″]Insulin Drone Delivery? | Tech Thursday

The world’s first drone delivery of insulin may be a useful model in response to the COVID-19 pandemic.
For people in rural, remote and isolated urban areas, using a drone to deliver much-needed insulin supplies is an option under consideration. A test flight in Ireland used a drone to deliver insulin as a response to people who were stranded without insulin during Hurricane Ophelia and the post-winter storm Emma when people were snowed in.
“Drone delivery has endless possibilities and can help us connect with our patient communities even in the most remote areas during sentinel events such as hurricanes, earthquakes, and pandemics, which have unfortunately become more common,” Spyridoula Maraka, MD, MS told Healio/Endo.
Though drone delivery has endless possibilities, there are also significant regulatory challenges with “aviation, medication dispensing, pharmaceutical dispensing, and cold chain protocols,” that had to be accounted for during this test run. Markara explains that through each phase of the mission, they had to have backup procedures in place.
Even with the obstacles for drone delivery of insulin or life-saving medications, this is an innovative and exciting prospect for people living in remote or isolated areas.
During the current pandemic, endocrinologists and care providers encourage people that use insulin to have enough stores at home for prolonged “Stay At Home” orders. As stated in our recent Question of the Week people with diabetes are not necessarily at increased risk for contracting COVID-19, but are at risk for experiencing worse outcomes and series complications from the virus (click here to review ADA’s Treatment & Care Factsheet). People living with diabetes may also experience a compromised immune system if blood glucose levels are running above target for a prolonged amount of time.
For these reasons, it is of utmost importance to have the necessary supplies and insulin one needs for optimal glucose levels during periods of crisis, like a pandemic.
To read more, click here and here for more valuable information regarding staying prepared in the pandemic with your insulin and diabetes supplies.
Written by Catherine Cullinane RN, CDCES, our resident Tech Thursday Content Writer
Sign up for Diabetes Blog Bytes – we post one daily Blog Byte from Monday to Friday. And of course, Tuesday is our Question of the Week. It’s Informative and FREE! Sign up below!
[yikes-mailchimp form=”1″]COVID-19, Sick Days & Diabetes | QoW Rationale

Our March 31st Question of the week was a question about COVID-19, sick days and diabetes. Although 40% of respondents chose the correct answer, 60% did not. We thought that this was an important topic to discuss further, so we can pass on correct info to people living with diabetes.
Before we start though, if you don’t want any spoilers and haven’t tried the question yet, you can answer below: Answer Question
JR is 27 with Type 1 diabetes and is very worried about getting COVID-19 since they work in a local grocery store. They ask you what they should do if they get COVID-19?
Which of the following statements is accurate regarding sick day management with COVID-19?
Answer Choices:
- Seek immediate medical attention if lips or face become bluish.
- Report to the emergency room if the temperature is 101 degrees or greater.
- Reduce insulin intake by 10-20% if experiencing diarrhea.
- Use glucose fingersticks instead of continuous glucose monitoring (CGM) when febrile to improve accuracy.
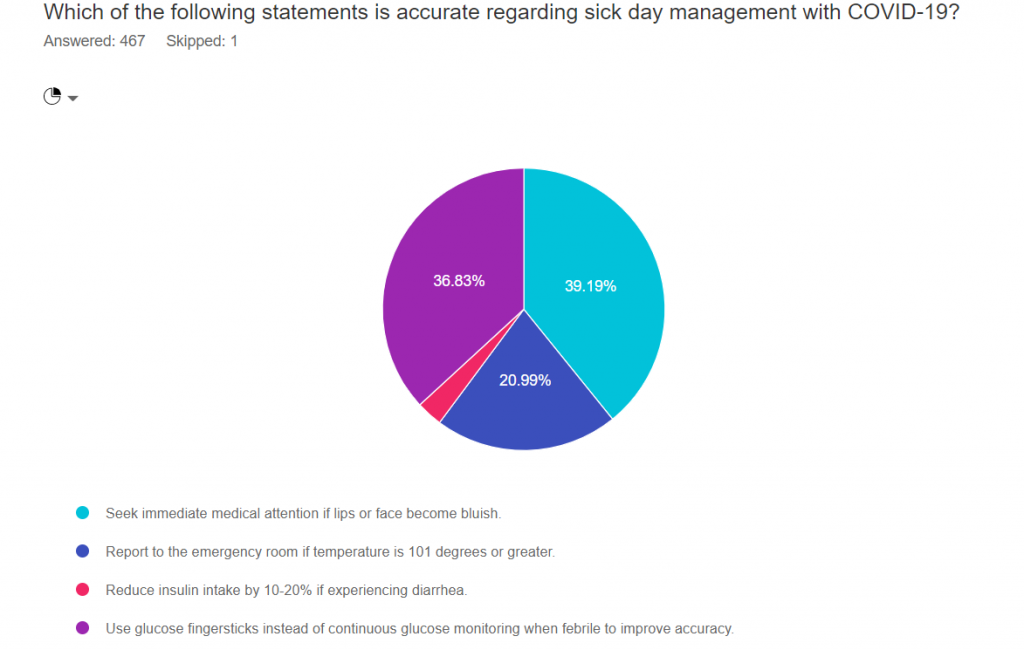
As shown above, the most common choice was option 1, the second most common answer was option 4, then option 2, and finally option 3.
Only 39% of participants chose the correct answer number 3, which means there is a learning opportunity!
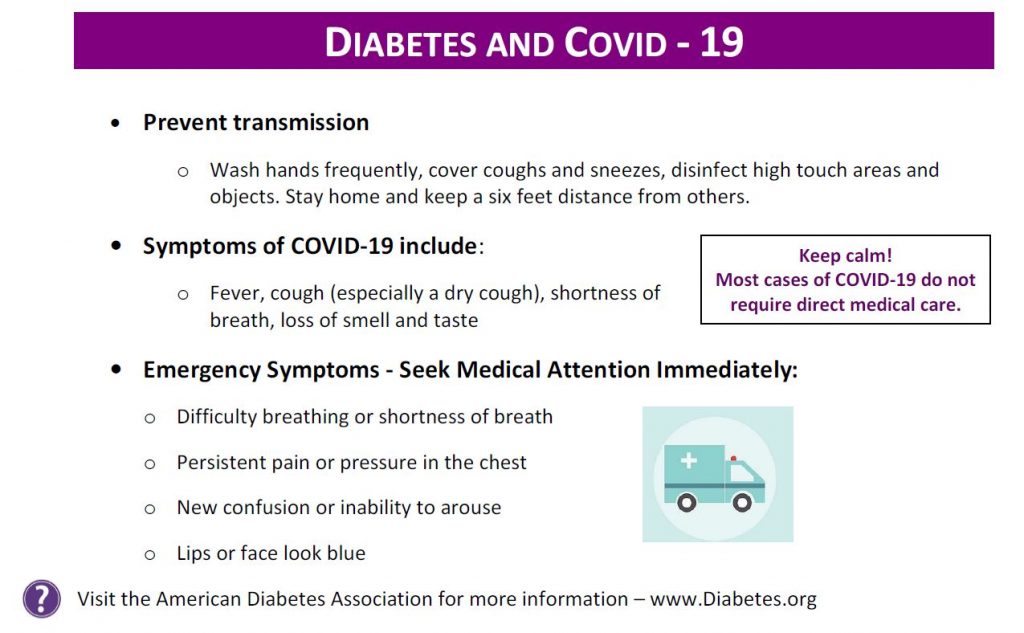
Answer 1 is Correct! Seek immediate medical attention if lips or face become bluish. Bluish lips or face indicates hypoxia and signals urgent medical care is needed.
From ADA Sick Day Information. If develop emergency warning signs for COVID-19 get medical attention immediately.
In adults, emergency warning signs include:
- Difficulty breathing or shortness of breath
- Persistent pain or pressure in the chest
- New confusion or inability to arouse
- Bluish lips or face
Option 2 is incorrect. One-fifth of respondents chose ” Report to the emergency room if the temperature is 101 degrees or greater.” In the case of fever, the next step would to be to contact your provider to evaluate presence of cough, shortness of breath and other symptoms to determine if urgent care is required.
Option 3 is also incorrect. “Reduce insulin intake by 10-20% if experiencing diarrhea.” During periods of illness, inflammation leads to insulin resistance and hyperglycemia. Most people will need to increase insulin dose during illness, including GI distress.
Finally, Option 4 is incorrect. “Use glucose fingersticks instead of continuous glucose monitoring when febrile to improve accuracy.”
Fever by itself does not interfere with CGM accuracy. If a person is taking Tylenol, it can interfere with the accuracy certain CGMs. And, CGM use is not recommended in the Intensive Care setting. But, having a temperature by itself, does not interfere with CGM accuracy.
Here is a COVID and Sick Day Handout that you can share with your community. Thank you for helping us get the word out.
For more information on sick day management and when to seek medical care, please see this ADA Sick Day Information.
We hope you appreciate this week’s rationale and keep studying hard! Thank you so much for taking the time to answer our Question of the Week and participate in this fun learning activity!
Sign up for Diabetes Blog Bytes – we post one daily Blog Byte from Monday to Friday. And of course, Tuesday is our Question of the Week. It’s Informative and FREE! Sign up below!
[yikes-mailchimp form=”1″]









