
Subscribe
eNewsletter

Ready to get certified?
Free CDCES Coach App
Download
Free Med Pocket Cards
We received dozens of applications for our Making a Difference Scholarship. Even better, an anonymous donor generously contributed two additional scholarships, so we able to award four scholarships in total. Each scholar winner is awarded CDCES Deluxe Online Prep Bundle | 44+ CEs plus additional study tools (a value of over $450) to acknowledge their service.
It was a great personal joy for our team to read these scholarship applications. Each applicant is serving communities with a great need and going “above and beyond” to promote and provide accessible diabetes care and education. It is always a very difficult decision for all of the judges, and we read each application in careful detail considering the financial need, impact, volunteerism, and readiness to take the CDCES exam.
We greatly appreciate the good work of all the applicants and thank them for their service!
Making a Difference Scholarships

We are excited to recognize and reward diabetes advocates who are making a difference in their community while working toward certification (CDCES). In recognition of health disparities, this award considers health care professionals whose daily actions, volunteer activities and advocacy work is making a significant difference in improving the health of their people.
We are excited to announce our “Making a Difference” scholarship winners, Rachel Patton and Mercy Edziah.
Diabetes Educator Flower Scholarships awarded by a generous donor, this new annual Flower Scholarship awards two health care professionals who are taking a leadership role in making significant contributions to under-served communities through their work and volunteer activities. Two of our applicants are living examples of giving back to their communities and are recognized for their hard work, grit, and hope.
We are pleased to announce our Flower Diabetes Educator Scholarship winners, Alexa Guzman and Chinethia Johnson. Learn about the Flower Scholarship here.

Rachel Patton is a trailblazer and fierce advocate for those in need
Rachel works in a non-profit community health center where she serves primarily with people who are un/underinsured, have Medicaid, or Medicare. In her work, she supports people living with diabetes who have barriers in glucose control due to houselessness or depression.
?She has advocated for the accessibility of continuous glucose monitors and other supplies at no or reduced cost for those she works with, even taking the time to call pharmacies to find ways to make supplies more affordable. At community events and health fairs, she has offered her time and expertise to raise awareness about diabetes. She has also created recipe booklets with those in mind who have limited cooking utensils, for example, heart-healthy crockpot recipes that uses items like mugs or spoons to measure ingredients.

Mercy Edziah combines culture, food and cooking classes
Mercy volunteers at a local hospital where she is passionate about increasing her cultural intelligence while working with people living with diabetes from diverse backgrounds. There she leads group classes, peer-to-peer support groups, along with individual sessions.
?Mercy also brings her experience with agriculture and food service to support the hospital’s greenhouse that provides fresh produce for the hospital’s weekly farmer’s market and cooking classes offered in the hospital’s wellness center. In her practice, she individualizes her care plans that match each individual’s access and needs. She is an advocate and pillar of support for people living with diabetes within her community.
Alexa Guzman uses Food Pharmacy Prescriptions to promote health.
Alexa volunteers with her local church and other local health centers to empower her community through education on diabetes management and prevention. In her practice, she works with people who have poor social determinants of health, and little to no access to care.
She is passionate about food accessibility and has adopted the concept of a “Food Pharmacy.” In this practice philosophy, she prescribes food plans that anchor on individual access and that are culturally sensitive. She believes her recommendations should not be confined to only an ”American diet.” Her goal of becoming a CDCES will allow her to expand her impact of providing a high level of care that is realistic and obtainable to those within her community.
Chinethia Johnson is a volunteer extraordinaire.
For Chinethia, diabetes is a disease that holds a personal significance in her heart. Because of her experience with the first-hand impacts of diabetes, she is driven to provide education and support the those she holds dear.
Each month she spends over 40 hours volunteering her time and knowledge either in person, over Zoom or the phone, to people living with diabetes or those who want to learn more about prevention. Outside of the inspiring number of hours she spends each month volunteering, she also juggles being a case manager, a mother, and a grandmother, all while being in school working to obtain her masters in nursing.

Please enjoy these FREE resources that we have put together for you:
See Full Free Resource Catalog
We are excited to announce the new Diabetes Flower Scholarship. We are awarding one of these scholarship this year, valued at $1000. This scholarship is available due to the generous contribution of an anonymous colleague, friend, co-instructor, and mentor.
Our donor worked as a Nurse Practitioner and Diabetes Specialist, serving her community, plus mentoring health care professionals about diabetes for over 30 years.
With the Flower Diabetes Educator Scholarship, she wants to keep investing in the health of our future by supporting future diabetes educators.
Her vision is to increase diversity in the diabetes education workforce by supporting diabetes nurse educators who come from under-served communities. By increasing the number of diabetes educators who represent the population demographics of those living with diabetes, we can make more meaningful connections on an individual and community level while promoting best care.
To be eligible for these scholarships, the U.S. health care professional is a diabetes nurse educator who comes from an under-served community and is providing care and education to communities that lack access to Diabetes Specialists and health care resources. Applicants will also be working toward certification (CDCES) within the next year and preference is given to those facing financial hardships that are interfering with their ability to pursue this dream.
The Flower Scholarship is valued at $1000 and includes:

The Flower Scholarship is a tribute to our donor’s last name, which translates to flower. The flower is a perfect symbol for this scholarship that aims to support the growth of novice diabetes educators into Certified Diabetes Care and Education Specialists.
Flowers are a symbol of hope and can be found growing in the most unexpected places, including harsh cities and forgotten spaces. With just a little sunlight and water, they have the ability to thrive in even the most difficult situations and shine their fierce beauty. Given a chance, as these flowers are tended to and nurtured, they grow stronger and brighter, spreading their beauty to new places to give people hope. These resilient flowering seeds perpetuate the opportunity for a future generation of diabetes specialists.
We know that a great resource page full of accurate and helpful cheat sheets can save busy diabetes specialists time and energy.
That’s why we have put together our entire list of cheat sheets so you can access them with ease.
These sheets and cards include information to study for certification exams and to use in your clinical setting. Plus, we have included teaching sheets for people with diabetes.

In each webinar, either Coach Beverly, Dr. Isaacs, or Ms. Armstrong, highlight the critical content of each topic area, so you can focus your study time most efficiently. They also launch multiple poll questions to help participants focus on key concepts and assess their knowledge while learning the best test-taking strategies.
2020 Boot Camp Live Stream Webinar Schedule with Coach Beverly
All courses air at 11:30 a.m. (PST)
Can’t make it live?
No worries! All video presentations and podcasts will be available now on-demand.
Sign up for Diabetes Blog Bytes – we post one daily Blog Byte from Monday to Friday. And of course, Tuesday is our Question of the Week. It’s Informative and FREE! Sign up below!
[yikes-mailchimp form=”1″]Accreditation: Diabetes Education Services is an approved provider by the California Board of Registered Nursing, Provider 12640, and Commission on Dietetic Registration (CDR), Provider DI002. Since these programs are approved by the CDR it satisfies the CE requirements for the CDCES regardless of your profession.*
The use of DES products does not guarantee the successful passage of the CDCES exam. CBDCE does not endorse any preparatory or review materials for the CDCES exam, except for those published by CBDCE.
[yikes-mailchimp form=”1″]
Unsure about updates for the 2020 exam?
Coach Beverly offers this FREE webinar to help get you to prepare for the CDCES Exam. All her tips and tricks are meant to ease your mind and reflect the updates to the CDCES content outline.
Instructor: Beverly Thomassian RN, MPH, CDCES, BC-ADM is a working educator who has passed her CDCES Exam 6 times. She is a nationally recognized diabetes expert for over 25 years.
See our Preparing for CDCES Resource Page >>
Test Taking Toolkit (220+ practice questions)
Whether you are preparing for the updated CDCES or BC-ADM exam, this test-taking toolkit is designed to prepare you for success.
This toolkit includes two courses with over 220 practice questions to help you prepare and simulate the exam.
Sign up for Diabetes Blog Bytes – we post one daily Blog Byte from Monday to Friday. And of course, Tuesday is our Question of the Week. It’s Informative and FREE! Sign up below!
[yikes-mailchimp form=”1″]Accreditation: Diabetes Education Services is an approved provider by the California Board of Registered Nursing, Provider 12640, and Commission on Dietetic Registration (CDR), Provider DI002. Since these programs are approved by the CDR it satisfies the CE requirements for the CDCES regardless of your profession.*
The use of DES products does not guarantee the successful passage of the CDCES exam. CBDCE does not endorse any preparatory or review materials for the CDCES exam, except for those published by CBDCE.
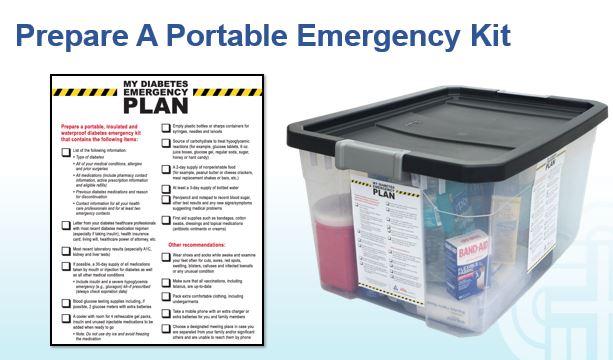
As we enter fire and storm season, it’s always a good idea to think ahead and be prepared for disaster. In addition to the items listed below, make sure to pack hand sanitizer, wipes, and masks due to the current pandemic. Also, bring your own pillow and bedding in case you need to spend time in a shelter.
For any emergency scenario, it’s important to have an emergency preparedness plan. For people living with diabetes, a “diabetes kit” is an important part of emergency preparedness. Diabetes Disaster Response Coalition (DDRC) has put together great resources to help people with diabetes be prepared so that no one is caught unaware without medication.
DDRC’s Diabetes Kit checklist includes needed supplies, but more importantly, information that should be written down and kept in a waterproof container for emergency situations where a health care provider could find it and make informed emergency treatment decisions.
Emergency Evacuation-Items to Gather for People with Diabetes
We thought this list was a helpful way to prioritize what items to grab given different time frame limitations. We found it online, and customized it for people with diabetes. It is available in Word or PDF. Thank you for sharing with your colleagues and community.
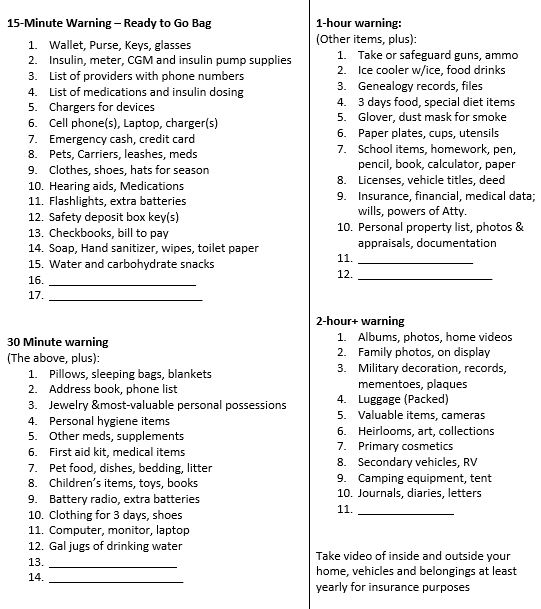
1-800-DIABETES (800-342-2383) is an excellent referral resource for people with diabetes to call toll free for updates on accessing medical support during an emergency.
Sign up for Diabetes Blog Bytes – we post one daily Blog Byte from Monday to Friday. And of course, Tuesday is our Question of the Week. It’s Informative and FREE! Sign up below!
[yikes-mailchimp form=”1″]
Join us Aug 20, 2020 @ 11:30 – 12:40 p.m. PST
Many of you are curious about the steps involved in becoming a BC-ADM. Thank you for reaching out to us with your questions about eligibility and study strategies. Coach Beverly will be providing answers to your questions interwoven with her own journey to achieve her Board Certification in Advanced Diabetes Management (BC-ADM).
Becoming Board Certified in Advanced Diabetes Management (BC-ADM) is an excellent professional goal for diabetes specialists with an advanced degree in their field and a professional license as an advanced practice nurse, registered dietitian, or registered pharmacist or provider.
The person holding the BC-ADM credential skillfully manages complex patient needs and assists patients with their therapeutic problem-solving. Within their scope of practice, healthcare professionals who hold the BC-ADM certification:
The scope of advanced diabetes practice includes clinical management skills such as medication adjustment, medical nutrition therapy, exercise planning, counseling for behavior management, and psycho-social issues. There is a focus on research, national standards, medical management of diabetes, and co-conditions, with a person-centered care approach.

This free webinar will review BC-ADM requirements for the current year.
Coach Beverly will discuss:
She will also review sample test questions and reasoning behind choosing the right answers. We hope you can join us.
Aug 20, 2020 @ 11:30 – 12:40 p.m. PST
The use of DES products does not guarantee the successful passage of the CDCES exam. CBDCE does not endorse any preparatory or review materials for the CDCES exam, except for those published by CBDCE.
**To satisfy the requirement for renewal of certification by continuing education for the Certification Board for Diabetes Care & Education (CBDCE), continuing education activities must be applicable to diabetes and approved by a provider on the CBDCE List of Recognized Providers (www.ncbde.org). CBDCE does not approve of continuing education. Diabetes Education Services is accredited/approved by the Commission of Dietetic Registration which is on the list of CBDCE Recognized Providers.”
Sign up for Diabetes Blog Bytes – we post one daily Blog Byte from Monday to Friday. And of course, Tuesday is our Question of the Week. It’s Informative and FREE! Sign up below!
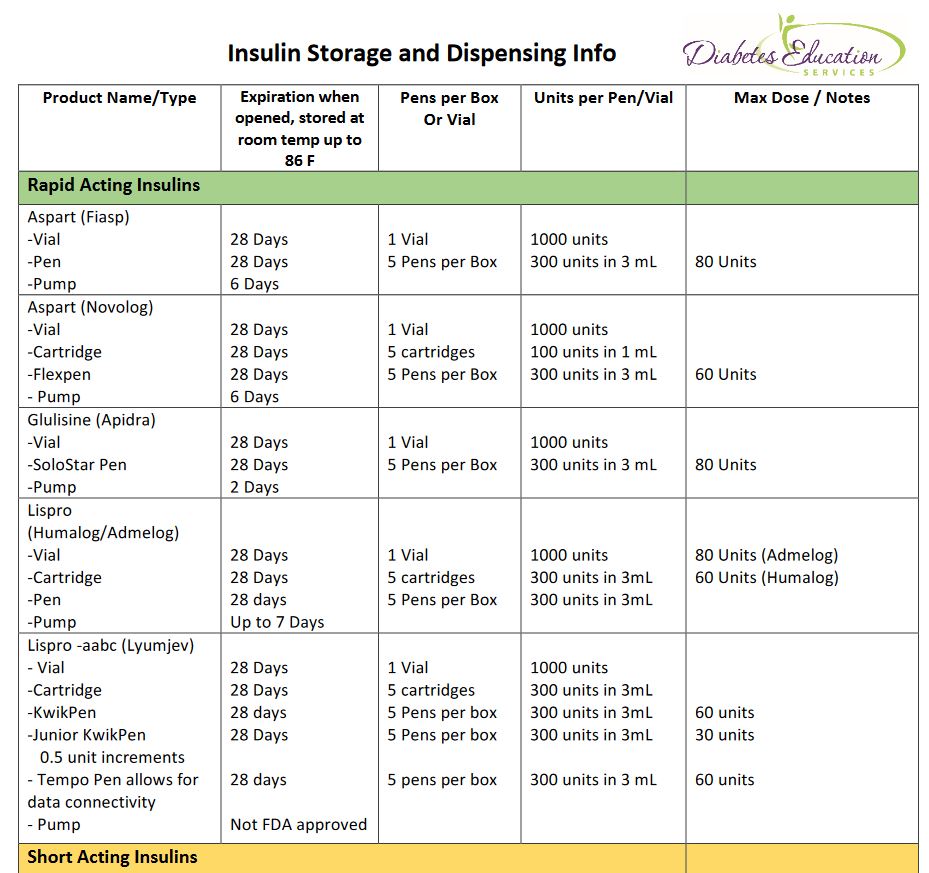
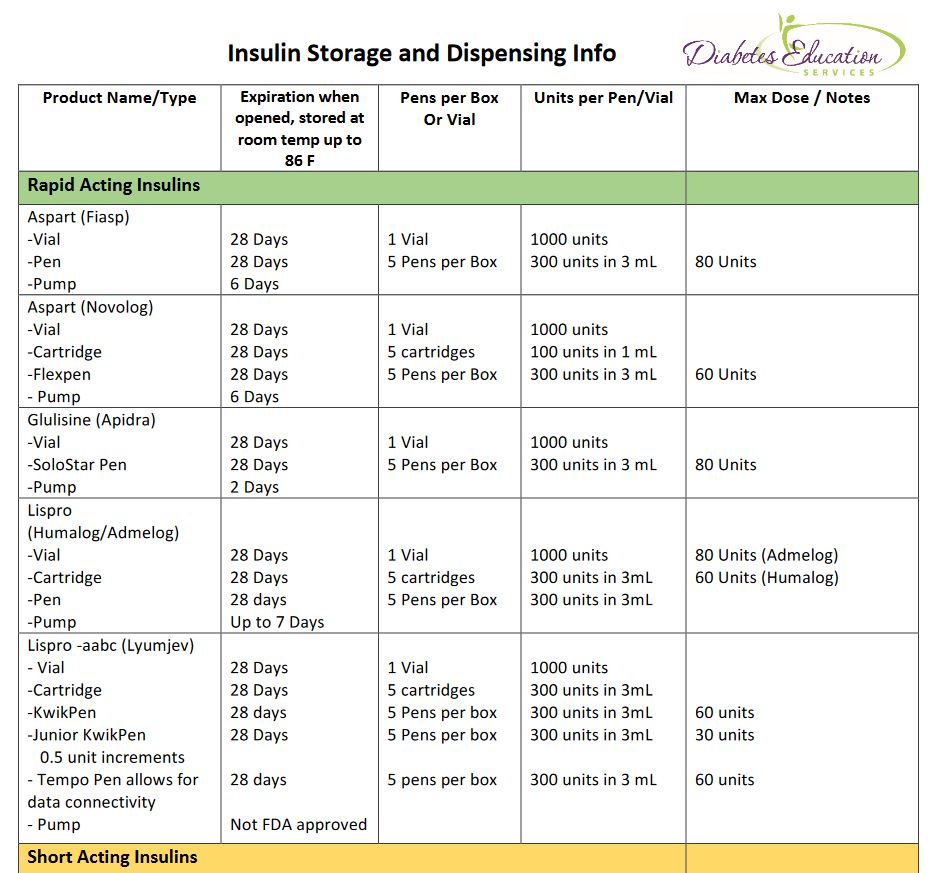
[yikes-mailchimp form=”1″]How long does glulisine last in pumps? What insulins can people buy without a prescription? What is the longest lasting insulin? If you want to learn the answers to these questions an more, we are here to help!
With the pandemic and ongoing insulin pricing issues, many people are struggling to pay for their insulin. Armed with information, we can help people maximize their insulin use and optimize their choices.
By knowing how long different insulin formulations last when kept at room temperature (temps up to 86 degrees), we can help people use their insulin as long as it is safe and recommended.
We usually say insulin is good for about 28 days. This is correct for many insulins, but not all.
For example, a vial of Human Regular insulin is good at room temp for 42 days. Degludec (Tresiba) is good for 56 days and Novolin 70/30 vial is good for 42 days. Glulisine (Apidra) expires after 2 days in an insulin pump, but lasts for 28 days in a vial.
See our new and exciting Insulin Storage Cheat Sheet for all kinds of important details on storage and more!
In addition, did you know that there are 3 insulins that do not require a prescription in most states? Regular, NPH and Regular/NPH combo insulins require no prescription.
A recent client ran out of their aspart insulin, was low on cash and out of town. They walked into a local Walmart, without a prescription, and paid $25 cash for a vial of regular insulin. This is incredibly important information to share with clients as a back up in case of emergency.
How many times have you launched into a google search or scoured insulin package inserts to find out the following questions or something like it?
Our Insulin Storage Cheat Sheet answers these questions and more!
Special thanks to Jackson Thomassian for compiling the first drafts of these sheets and to Diana Isaacs, PharmD for her inspiration.
Even though Coach Beverly has reviewed and edited these sheets dozens of times, she knows there is always room for improvement. Please let us know if you see content that needs updating. In appreciation, Beverly


AR is 16 years old and is struggling with weight. AR was diagnosed with type 2 diabetes and has met with the dietitian and diabetes specialist. In spite of eating healthier and a 3% weight loss, AR’s A1c is increasing and is currently 7.6%. The provider decides to start AR on medication.
Which of the following FDA approved medications should the provider prescribe?
Click here to test your knowledge!