
Subscribe
eNewsletter

Ready to get certified?
Free CDCES Coach App
Download
Free Med Pocket Cards
We are excited to announce the new Diabetes Flower Scholarship. We are awarding one of these scholarship this year, valued at $1000. This scholarship is available due to the generous contribution of an anonymous colleague, friend, co-instructor, and mentor.
Our donor worked as a Nurse Practitioner and Diabetes Specialist, serving her community, plus mentoring health care professionals about diabetes for over 30 years.
With the Flower Diabetes Educator Scholarship, she wants to keep investing in the health of our future by supporting future diabetes educators.
Her vision is to increase diversity in the diabetes education workforce by supporting diabetes nurse educators who come from under-served communities. By increasing the number of diabetes educators who represent the population demographics of those living with diabetes, we can make more meaningful connections on an individual and community level while promoting best care.
To be eligible for these scholarships, the U.S. health care professional is a diabetes nurse educator who comes from an under-served community and is providing care and education to communities that lack access to Diabetes Specialists and health care resources. Applicants will also be working toward certification (CDCES) within the next year and preference is given to those facing financial hardships that are interfering with their ability to pursue this dream.
The Flower Scholarship is valued at $1000 and includes:

The Flower Scholarship is a tribute to our donor’s last name, which translates to flower. The flower is a perfect symbol for this scholarship that aims to support the growth of novice diabetes educators into Certified Diabetes Care and Education Specialists.
Flowers are a symbol of hope and can be found growing in the most unexpected places, including harsh cities and forgotten spaces. With just a little sunlight and water, they have the ability to thrive in even the most difficult situations and shine their fierce beauty. Given a chance, as these flowers are tended to and nurtured, they grow stronger and brighter, spreading their beauty to new places to give people hope. These resilient flowering seeds perpetuate the opportunity for a future generation of diabetes specialists.
We know that a great resource page full of accurate and helpful cheat sheets can save busy diabetes specialists time and energy.
That’s why we have put together our entire list of cheat sheets so you can access them with ease.
These sheets and cards include information to study for certification exams and to use in your clinical setting. Plus, we have included teaching sheets for people with diabetes.

In each webinar, either Coach Beverly, Dr. Isaacs, or Ms. Armstrong, highlight the critical content of each topic area, so you can focus your study time most efficiently. They also launch multiple poll questions to help participants focus on key concepts and assess their knowledge while learning the best test-taking strategies.
2020 Boot Camp Live Stream Webinar Schedule with Coach Beverly
All courses air at 11:30 a.m. (PST)
Can’t make it live?
No worries! All video presentations and podcasts will be available now on-demand.
Sign up for Diabetes Blog Bytes – we post one daily Blog Byte from Monday to Friday. And of course, Tuesday is our Question of the Week. It’s Informative and FREE! Sign up below!
[yikes-mailchimp form=”1″]Accreditation: Diabetes Education Services is an approved provider by the California Board of Registered Nursing, Provider 12640, and Commission on Dietetic Registration (CDR), Provider DI002. Since these programs are approved by the CDR it satisfies the CE requirements for the CDCES regardless of your profession.*
The use of DES products does not guarantee the successful passage of the CDCES exam. CBDCE does not endorse any preparatory or review materials for the CDCES exam, except for those published by CBDCE.
[yikes-mailchimp form=”1″]
Unsure about updates for the 2020 exam?
Coach Beverly offers this FREE webinar to help get you to prepare for the CDCES Exam. All her tips and tricks are meant to ease your mind and reflect the updates to the CDCES content outline.
Instructor: Beverly Thomassian RN, MPH, CDCES, BC-ADM is a working educator who has passed her CDCES Exam 6 times. She is a nationally recognized diabetes expert for over 25 years.
See our Preparing for CDCES Resource Page >>
Test Taking Toolkit (220+ practice questions)
Whether you are preparing for the updated CDCES or BC-ADM exam, this test-taking toolkit is designed to prepare you for success.
This toolkit includes two courses with over 220 practice questions to help you prepare and simulate the exam.
Sign up for Diabetes Blog Bytes – we post one daily Blog Byte from Monday to Friday. And of course, Tuesday is our Question of the Week. It’s Informative and FREE! Sign up below!
[yikes-mailchimp form=”1″]Accreditation: Diabetes Education Services is an approved provider by the California Board of Registered Nursing, Provider 12640, and Commission on Dietetic Registration (CDR), Provider DI002. Since these programs are approved by the CDR it satisfies the CE requirements for the CDCES regardless of your profession.*
The use of DES products does not guarantee the successful passage of the CDCES exam. CBDCE does not endorse any preparatory or review materials for the CDCES exam, except for those published by CBDCE.
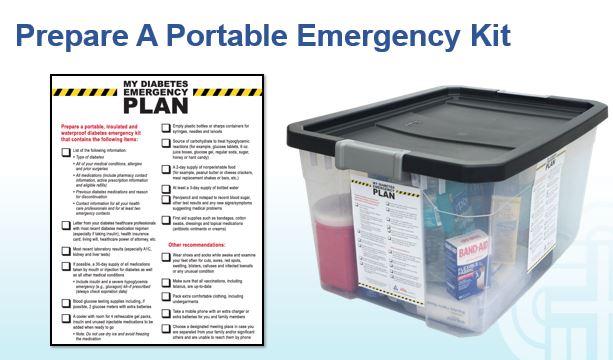
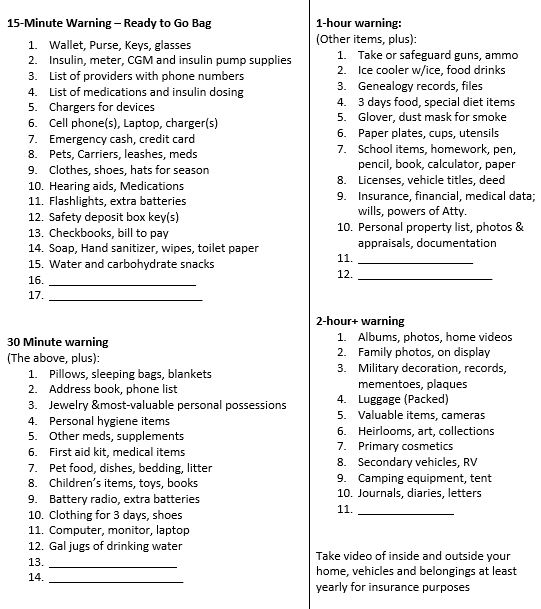
As we enter fire and storm season, it’s always a good idea to think ahead and be prepared for disaster. In addition to the items listed below, make sure to pack hand sanitizer, wipes, and masks due to the current pandemic. Also, bring your own pillow and bedding in case you need to spend time in a shelter.
For any emergency scenario, it’s important to have an emergency preparedness plan. For people living with diabetes, a “diabetes kit” is an important part of emergency preparedness. Diabetes Disaster Response Coalition (DDRC) has put together great resources to help people with diabetes be prepared so that no one is caught unaware without medication.
DDRC’s Diabetes Kit checklist includes needed supplies, but more importantly, information that should be written down and kept in a waterproof container for emergency situations where a health care provider could find it and make informed emergency treatment decisions.
Emergency Evacuation-Items to Gather for People with Diabetes
We thought this list was a helpful way to prioritize what items to grab given different time frame limitations. We found it online, and customized it for people with diabetes. It is available in Word or PDF. Thank you for sharing with your colleagues and community.
1-800-DIABETES (800-342-2383) is an excellent referral resource for people with diabetes to call toll free for updates on accessing medical support during an emergency.
Sign up for Diabetes Blog Bytes – we post one daily Blog Byte from Monday to Friday. And of course, Tuesday is our Question of the Week. It’s Informative and FREE! Sign up below!
[yikes-mailchimp form=”1″]
Join us Aug 20, 2020 @ 11:30 – 12:40 p.m. PST
Many of you are curious about the steps involved in becoming a BC-ADM. Thank you for reaching out to us with your questions about eligibility and study strategies. Coach Beverly will be providing answers to your questions interwoven with her own journey to achieve her Board Certification in Advanced Diabetes Management (BC-ADM).
Becoming Board Certified in Advanced Diabetes Management (BC-ADM) is an excellent professional goal for diabetes specialists with an advanced degree in their field and a professional license as an advanced practice nurse, registered dietitian, or registered pharmacist or provider.
The person holding the BC-ADM credential skillfully manages complex patient needs and assists patients with their therapeutic problem-solving. Within their scope of practice, healthcare professionals who hold the BC-ADM certification:
The scope of advanced diabetes practice includes clinical management skills such as medication adjustment, medical nutrition therapy, exercise planning, counseling for behavior management, and psycho-social issues. There is a focus on research, national standards, medical management of diabetes, and co-conditions, with a person-centered care approach.

This free webinar will review BC-ADM requirements for the current year.
Coach Beverly will discuss:
She will also review sample test questions and reasoning behind choosing the right answers. We hope you can join us.
Aug 20, 2020 @ 11:30 – 12:40 p.m. PST
The use of DES products does not guarantee the successful passage of the CDCES exam. CBDCE does not endorse any preparatory or review materials for the CDCES exam, except for those published by CBDCE.
**To satisfy the requirement for renewal of certification by continuing education for the Certification Board for Diabetes Care & Education (CBDCE), continuing education activities must be applicable to diabetes and approved by a provider on the CBDCE List of Recognized Providers (www.ncbde.org). CBDCE does not approve of continuing education. Diabetes Education Services is accredited/approved by the Commission of Dietetic Registration which is on the list of CBDCE Recognized Providers.”
Sign up for Diabetes Blog Bytes – we post one daily Blog Byte from Monday to Friday. And of course, Tuesday is our Question of the Week. It’s Informative and FREE! Sign up below!
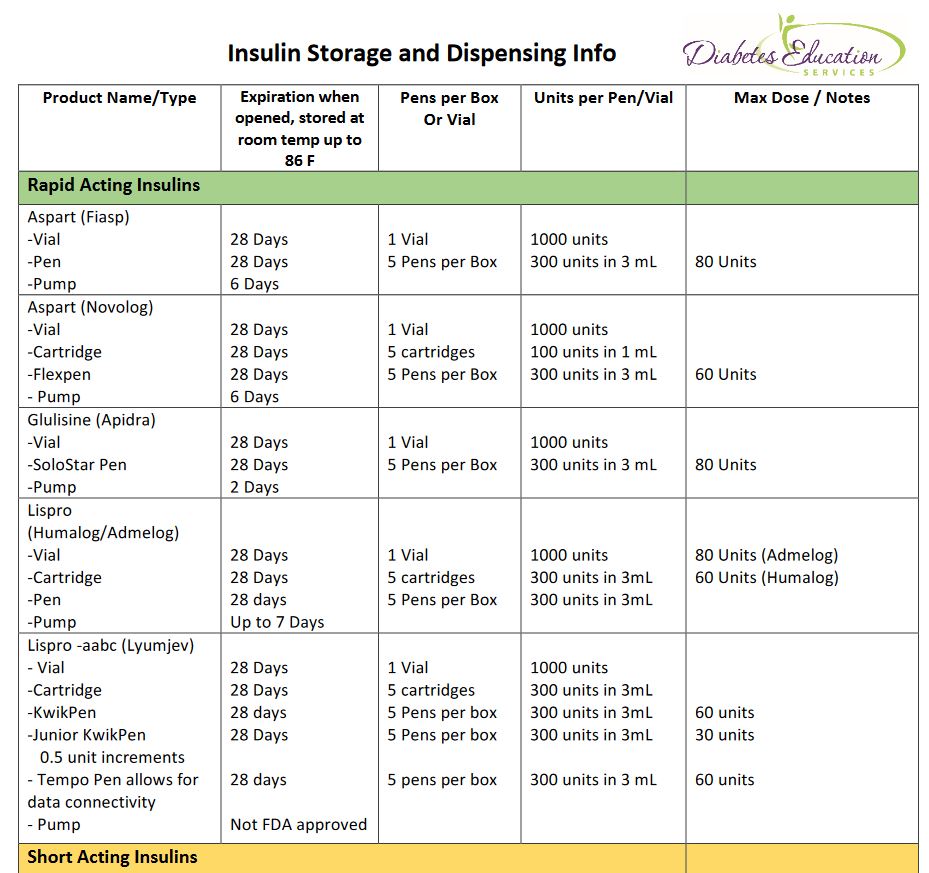
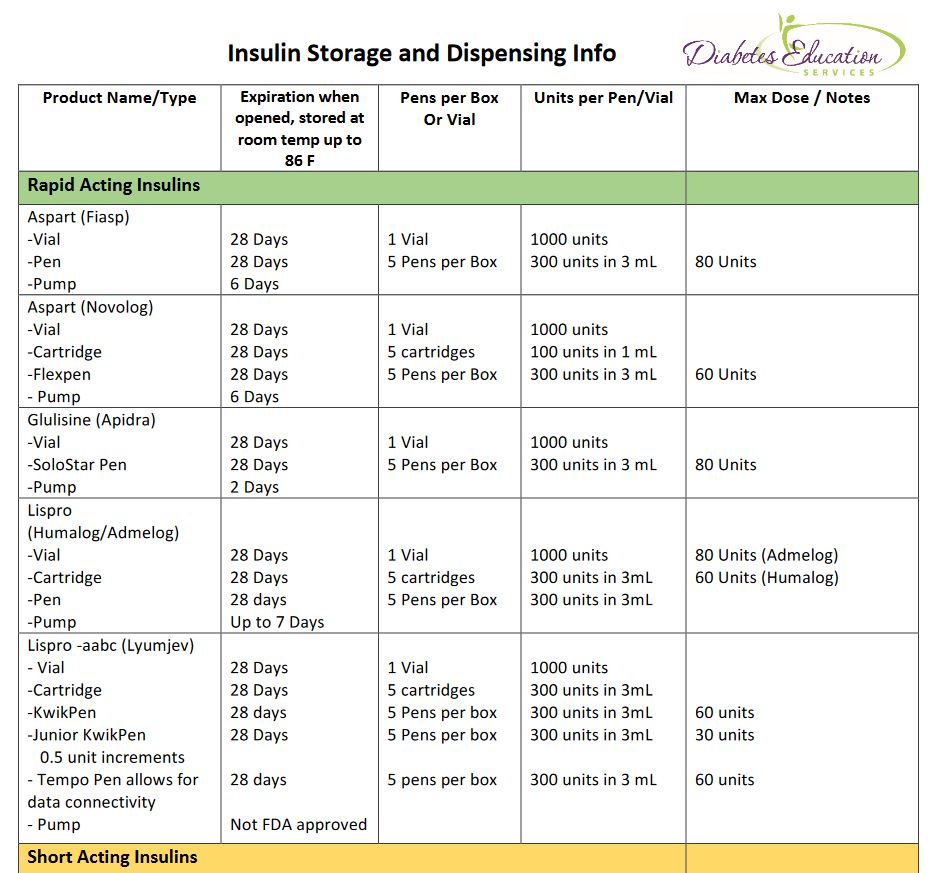
[yikes-mailchimp form=”1″]How long does glulisine last in pumps? What insulins can people buy without a prescription? What is the longest lasting insulin? If you want to learn the answers to these questions an more, we are here to help!
With the pandemic and ongoing insulin pricing issues, many people are struggling to pay for their insulin. Armed with information, we can help people maximize their insulin use and optimize their choices.
By knowing how long different insulin formulations last when kept at room temperature (temps up to 86 degrees), we can help people use their insulin as long as it is safe and recommended.
We usually say insulin is good for about 28 days. This is correct for many insulins, but not all.
For example, a vial of Human Regular insulin is good at room temp for 42 days. Degludec (Tresiba) is good for 56 days and Novolin 70/30 vial is good for 42 days. Glulisine (Apidra) expires after 2 days in an insulin pump, but lasts for 28 days in a vial.
See our new and exciting Insulin Storage Cheat Sheet for all kinds of important details on storage and more!
In addition, did you know that there are 3 insulins that do not require a prescription in most states? Regular, NPH and Regular/NPH combo insulins require no prescription.
A recent client ran out of their aspart insulin, was low on cash and out of town. They walked into a local Walmart, without a prescription, and paid $25 cash for a vial of regular insulin. This is incredibly important information to share with clients as a back up in case of emergency.
How many times have you launched into a google search or scoured insulin package inserts to find out the following questions or something like it?
Our Insulin Storage Cheat Sheet answers these questions and more!
Special thanks to Jackson Thomassian for compiling the first drafts of these sheets and to Diana Isaacs, PharmD for her inspiration.
Even though Coach Beverly has reviewed and edited these sheets dozens of times, she knows there is always room for improvement. Please let us know if you see content that needs updating. In appreciation, Beverly


AR is 16 years old and is struggling with weight. AR was diagnosed with type 2 diabetes and has met with the dietitian and diabetes specialist. In spite of eating healthier and a 3% weight loss, AR’s A1c is increasing and is currently 7.6%. The provider decides to start AR on medication.
Which of the following FDA approved medications should the provider prescribe?
Click here to test your knowledge!
Click here to view our Top 3 Blogs Newsletter

Happy Wednesday Diabetes Community!
We are excited to announce our new feature; Top 3 blog posts of the Month.
Coach Beverly and team are committed to keeping you apprised of the latest findings in diabetes.
We promise to keep this end-of-the-month wrap-up announcement short and sweet while providing links to references so you can dig deeper.
As part of our commitment to sharing information, we are offering FREE webinar viewing of our Level 2 Standards Intensive Series. See upcoming topics and dates below.
Our top 3 blogs this month include the recall of some long-acting metformin brands, Medicare’s $35 monthly cap on insulin starting in 2021, and the rationale for this month’s most popular question of the week.
Happy early July 4th weekend. Please stay safe and take good care.
Coach Beverly
Click here to view our Top 3 Blogs Newsletter
Check out our new bundle!
Level 3 | Boot Camp + Expert Team Bundle
Join us live starting September 16th!
When you join our DiabetesEd Certification Boot Camp, it’s like having your own online coaching staff.
?In each webinar, either Coach Beverly, Dr. Isaacs, or Ms. Armstrong, highlight the critical content of each topic area, so you can focus your study time most efficiently. They also launch multiple poll questions to help participants focus on key concepts and assess their knowledge while learning the best test-taking strategies.
Mastery of this content is critical to ensure certification exam success and to improve clinical outcomes.
Click here to download Level 3 + Expert Bundle flyer
Sign up for Diabetes Blog Bytes – we post one daily Blog Byte from Monday to Friday. And of course, Tuesday is our Question of the Week. It’s Informative and FREE! Sign up below!
[yikes-mailchimp form=”1″]Accreditation: Diabetes Education Services is an approved provider by the California Board of Registered Nursing, Provider 12640, and Commission on Dietetic Registration (CDR), Provider DI002. Since these programs are approved by the CDR it satisfies the CE requirements for the CDCES regardless of your profession.*
The use of DES products does not guarantee the successful passage of the CDCES exam. CBDCE does not endorse any preparatory or review materials for the CDCES exam, except for those published by CBDCE.