National Diabetes Month – Resources
Ramadan & Fasting Considerations for People Living with Diabetes
Ramadan Mubarak… Happy Ramadan.
This evening, Ramadan begins. It is the most important spiritual time for the 1.8 billion Muslims around the world.
In Islam, Ramadan is the month in which the first verses of the Quran, were revealed to the Prophet Muhammad. In observance, many Muslims fast by abstaining from food, drink, smoking, and sex, from pre-sunrise to sunset. This fasting achieves greater “taqwa” or “consciousness to God.”
As Diabetes Care and Education specialists, we have the chance to provide tools for those who fast while keeping diabetes in mind.
The Association for Diabetes Care and Education Specialists (ADCES) put together some helpful handouts to better support people who are fasting and living with diabetes.
Below is the list of resources shared by ADCES
- Fasting and Diabetes web hub
- Fasting with Diabetes Healthcare professionals handout – This handout includes information for potential interventions, potential complications to look out for, nutritional recommendations, and more.
- Ramadan and Diabetes Handout for People Living with Diabetes – English
- Ramadan and Diabetes Handout for People Living with Diabetes – Arabic
To read more about Ramadan, click here.
To take our Question of the Week that considers Type 1 and fasting during Ramadan.
Rationale of the Week | How long are these insulin pens good for?

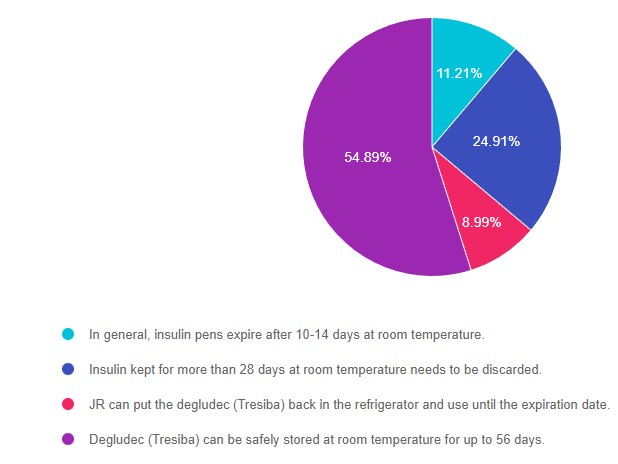
For last week’s practice question, we quizzed participants on insulin storage guidelines. 55% of respondents chose the best answer. We want to clarify and share this important information, so you can pass it on to people living with diabetes and your colleagues, plus prepare for exam success!
Before we start though, if you don’t want any spoilers and haven’t tried the question yet, you can answer it below: Answer Question
Question:
JR has a bunch of insulin pens at home and is wondering if they are still good to use. Most of the unopened insulin pens are stored in the fridge, but JR has 2 degludec (Tresiba) pens that they left out of the refrigerator by accident. They ask you if they are still good. What is the most accurate response for the shelf life of degludec (Tresiba) pens stored at room temperature of up to 86 degrees Fahrenheit?
Answer Choices:
- In general, insulin pens expire after 10-14 days at room temperature.
- Insulin kept for more than 28 days at room temperature needs to be discarded.
- JR can put the degludec (Tresiba) back in the refrigerator and use it until the expiration date.
- Degludec (Tresiba) can be safely stored at room temperature for up to 56 days.
Getting to the Best Answer
- In general, insulin pens expire after 10-14 days at room temperature. (incorrect) 11% of respondents chose this juicy answer. However, degludec has one of the longest shelf lives at room temperature due to its pharmacokinetics. NPH and premixed insulin like 70/30 insulins have a shorter shelf life of 10-14 days. You can refer to our Insulin Storage Guidelines or package inserts for more information.
- Insulin kept for more than 28 days at room temperature needs to be discarded. (incorrect) About 25% of respondents chose this answer. Most bolus insulins have a shelf life of about 28 days whether they are stored in an insulin pen or vial. But many basal and concentrated insulins have a longer shelf life. NPH and premixed insulin like 70/30 insulins have a shorter shelf life of 10-14 days. Given the cost of insulin, this is important information to share with people living with diabetes, so they are aware of accurate insulin storage guidelines. You can refer to our Insulin Storage Guidelines or package inserts for more information.
- JR can put the degludec (Tresiba) back in the refrigerator and use it until the expiration date. (incorrect) 9% of respondents chose this answer, however, it is not an accurate answer. Once insulin is left out at room temperature, the clock starts ticking and with time, the potency of the insulin diminishes. For insulin degludec, the shelf life is 56 days outside of the refrigerator. If JR isn’t sure how long the insulin has been sitting out, they can look at the box Rx label or contact their pharmacy and find out what day the insulin was dispensed. You can refer to our Insulin Storage Guidelines or package inserts for more information.
- Degludec (Tresiba) can be safely stored at room temperature for up to 56 days. (correct). YES, this is the BEST answer and 55% of you chose this answer. Degludec along with Toujeo (Lantus U-300) can both be stored at room temperature for up to 56 days. You can refer to our Insulin Storage Guidelines or package inserts for more information.
Practical Clinical Pointers: Of course, these are general storage guidelines and if people using insulin notice blood sugars climbing despite adequate insulin dosing, it can be a sign the insulin has lost its potency. Sometimes, people on a budget might decide to keep using insulin past the expiration date. In either case, we can advise individuals to switch to a new insulin vial or pen right away if they notice blood sugars unexplainably trending up.
Thank you so much for reading this “Rationale of the Week”.
Please refer to our Insulin Storage Guidelines or package inserts for more information. We also invite you to join our Online Courses for more information (see info below)
Hope you can join our ADA Standards of Care Webinar Update in February.
See below for info.
Want to learn more about this question? Join us for our
Level 2 | ADA Standards of Care CE Course | 2.0 CEs
Update airs live Feb. 2, 2023, at 11:30 am PST
This course, updated annually, is an essential review for anyone in the field of diabetes. Join Coach Beverly as she summarizes the 2023 updates to the American Diabetes Association’s Standards of Medical Care in Diabetes and provides critical teaching points and content for healthcare professionals involved in diabetes care and education.
Objectives:
- List significant changes and updates to the 2023 ADA Standards of Medical Care.
- State 3 updates on new blood pressure and lipid goals.
- Identify 5 key elements of the position statement.
- Discuss how to apply the Standards in the clinical setting and in preparation for exam success.
Intended Audience: This course is a knowledge-based activity designed for individuals or groups of diabetes professionals, including RNs, RDs, Pharmacists, Nurse Practitioners, Clinical Nurse Specialists, Physician Assistants, and other health care providers interested in staying up to date on current practices of care for people with prediabetes, diabetes and other related conditions.
Don’t worry if you can’t make it live. Your registration guarantees access to the recorded version in the Online University.
All hours earned count toward your CDCES Accreditation Information
Studying for the CDCES Exam? Enroll in our
CDCES Deluxe Prep Bundle | 30+ Online Courses + Bonus Items | 47 CEs
This bundle includes our CDCES Online Prep Bundle (featured above) plus the ADCES Review Guide – 5th Edition-Revised. The online bundle includes Level 1, Level 2, and Level 3 (Boot Camp), plus two bonus courses. The ADCES Review Guide offers over 480+ practice questions and is a fantastic independent study tool and comprehensive resource for the Diabetes Care and Education Specialist Exam.
Included in this bundle
- Level 1 focuses on the fundamentals and introduces each topic area for the exam.
- Level 2 deep dives into the ADA Standards of Care,
- Level 3 AKA Boot Camp is a more accelerated level that focuses on test simulation for finding the best answer to get you to the finish line of your study path.
- Technology Toolkit which gives information on pumps, sensors, and calculations,
- Test Taking Toolkit includes over 220 practice questions for test simulation plus a webinar where Coach Beverly provides test-taking tips based on her experience taking the certification exam six times.
- ADCES Review Guide for the Diabetes Care and Education Specialist Exam – 5th Edition – Revised – The ADCES Review Guide is a fantastic independent study tool and comprehensive resource for the Diabetes Care and Education Specialist Exam. This book includes 480 + multiple-choice questions and strategies for preparing for and taking the exam with an answer key with rationales for all questions!
- Medication PocketCard – Our four-sided medication accordion Pocketcards were designed by Coach Beverly Thomassian to assist in clinical practice and exam preparation.
- Tote Bag
Sign up for Diabetes Blog Bytes – we post one daily Blog Byte from Monday to Friday. And of course, Tuesday is our Question of the Week. It’s Informative and FREE! Sign up below!
The use of DES products does not guarantee the successful passage of the CDCES exam. CBDCE does not endorse any preparatory or review materials for the CDCES exam, except for those published by CBDCE.
Happy World Diabetes Day
I love November because we get to celebrate National Diabetes Month and World Diabetes Day on November 14th, which is Dr. Banting’s Birthday.
One hundred and one years ago, two researchers kick-started the production of insulin, making it available for worldwide use and saving millions of lives. Now, that’s a real cause for celebration. The discovery of insulin by Banting, Best, and team was no easy feat. They encountered resistance, setbacks, and failures.

Dr. Banting secured space to test out his theory at the University of Toronto during a hot summer in 1921. Along with his colleague, Charles Best, and a bare-bones lab, they conducted dozens of experiments on dogs. Marjorie (dog 408) lived for 70 days without a pancreas due to receiving life-saving insulin injections.
This success was replicated in other experimental dogs and ultimately provided the first step toward producing insulin from pig and cow pancreases.
In 1922, children with type 1 diabetes started receiving early doses of this newly available life-saving hormone. Leonard Thompson, was the first recipient in January 1922, followed by many thereafter. Here is a heartbreaking then uplifting photo of J.L., who after 2 months of receiving insulin, transformed into a healthy young boy.
To learn more about the Discovery of Insulin and download historical slides Click here!

We are Celebrating Diabetes Month with Giveaways and 30% Sale on Nov 28th
For the month of November:
- Join or View our 3 FREE webinars
- FREE Tote Bag + Pocket Card with Book or Teaching Tool Purchase
- Cyber Monday Sale – 30% off Online Courses on November 28th.
Sign up for Diabetes Blog Bytes – we post one daily Blog Byte from Monday to Friday. And of course, Tuesday is our Question of the Week. It’s Informative and FREE! Sign up below!
[yikes-mailchimp form=”1″]Accreditation: Diabetes Education Services is an approved provider by the California Board of Registered Nursing, Provider 12640, and Commission on Dietetic Registration (CDR), Provider DI002. Since these programs are approved by the CDR it satisfies the CE requirements for the CDCES regardless of your profession.*
The use of DES products does not guarantee the successful passage of the CDCES exam. CBDCE does not endorse any preparatory or review materials for the CDCES exam, except for those published by CBDCE.
Finding Gratitude During a Pandemic
As we all prepare for the holidays this year we may be having a difficult time feeling thankful.

As we continue to navigate this long-lasting pandemic there has been so much loss and heartache.
Years ago I went to a conference on preventing burnout in healthcare providers with Dr. J. Bryan Sexton, associate professor in psychiatry and behavioral sciences at Duke’s School of Medicine and an expert in the idea of resilience. He impressed me and I have talked about his conference to many colleagues over the years.
I loved sharing his wisdom with my clients, because of studies that link resilience to better diabetes self management. (1)
Lately, as I have been struggling with overwhelming feelings of sadness, I have remembered to practice some of his tools to cultivate resilience. Cultivating resiliency is something that takes daily focus. To cultivate means to nurture, grow, and encourage resilient behaviors.
Dr. Sexton suggests these three ways to increase resilience.
Three Good Things
Humans are hard-wired to remember the negative aspects of our day, but flipping around the natural inclination is simple.
Building resilience is possible by focusing on positive emotions – joy, serenity, hope gratitude, inspiration, pride, love, awe, and amusement.
Promoting positive thoughts and building resilience can be as easy as taking notes each night before bed. Think of three things that happened during the day that went well and your role in the positive outcome, then jot down those three things. Best results for this exercise come after 14 consecutive days. Empirical evidence shows that this elevates brain serotonin with positive effects on our mood that last for months. (2)
Show Gratitude
Grab a pen and paper and write a letter of appreciation to someone- anyone. Take five minutes to explain something they did, how it impacted you and the benefits you received. Whether you share the letter or not, Dr. Sexton said it can have lasting impacts, increasing happiness while lowering depressing thoughts because focusing on benefits forces us to linger on positive thoughts.
Rediscover Awe
Through an “awe intervention,” you can create a sense of slowed down time, which offers a calming sensation and a feeling of having more time available.
Awe also helps us to feel inspired. I call awe intervention, “joyful thanksgiving”. It is a practice that I am doing in which I acknowledge and give a little extra gratitude for the many amazing sights, sounds, tastes, relationships, information, and emotions that excite me and create awe right from the moment when I wake up.
Today as I was practicing my joyful thanksgiving I paid special attention to my breakfast of oatmeal, blueberries, banana, walnuts and cinnamon. I love oatmeal in the fall and winter months.
I began to feel grateful for this medicinal food. Oats, blueberries, banana, and nuts contain water soluble fiber which slow the absorption of sugar and fat from food, and therefore help prevent spikes in blood sugar and blood fat, possibly reducing the inflammatory response to food. (3)(4)
Fiber is a super food which provides important nutrition for our intestinal bacteria to live and prosper, that’s why fiber is called a pre-biotic. Vegetables, fruit, whole grains, nuts and legumes remain the single best sources of fiber in the diet. High-fiber vegetables include many of the green leafy vegetables like kale, collard greens, chard, arugula, and even lettuces. Whole-grain sources of fiber include oats, quinoa, barley and rye. Legumes include beans like peas, soy, black, pinto and lentils.
Encouraging our clients to consider adding more fiber rich dishes to the holiday meals this season and perhaps telling them about Dr. Sexton’s tools for cultivating resilience may help them to feel happier and more hopeful and contribute to better blood sugar control.
Blueberry-Banana Overnight Oats
½ cup unsweetened coconut milk beverage
½ cup old-fashioned oats
½ TB chia seeds
½ banana
1 tsp maple syrup
½ cup blueberries
2 TB chopped walnuts
1/8 tsp cinnamon
Combine coconut milk, oats, chia, banana, maple syrup in a pint-sized jar and stir. Top with blueberries and coconut. Cover and refrigerate overnight. Heat up and sprinkle with walnuts and cinnamon in the morning.
285 calories, 6 gm protein, 57 gms carbohydrate, 7 gms fiber 6 gm fat
- Understanding the links between resilience and type-2 diabetes self-management: a qualitative study in South Australia . Arch Public Health. 2017; 75: 56.
- Seligman, Steen, Park & Petersen (July-August 2005). Positive Psychology Progress: Empirical Validation of Intervention. American Psychologist
- The Metabolic Effects of Oats Intake in Patients with Type 2 Diabetes: A Systematic Review and
Meta-Analysis. Nutrients. 2015 Dec; 7(12): 10369-10387p. 1392:8
- Chandalia, M., et al., Beneficial effects of high dietary fiber intake in patients with type 2 diabetes mellitus. N Engl J Med, 2000. 342(19):
Sign up for Diabetes Blog Bytes – we post one daily Blog Byte from Monday to Friday. And of course, Tuesday is our Question of the Week. It’s Informative and FREE! Sign up below!
[yikes-mailchimp form=”1″]
Forest Bathing | Oxygen Cocktails can Boost Your Killer T Cells
The winter and holiday seasons can be stressful and wear us down, especially during the pandemic. We tend to spend more time indoors. To help out, we have some suggestions that will not only help with stress management but can also boost your immunity.
Walking outside in nature and drinking in an “oxygen cocktail” feels good, but does it benefit our immunity?
You might be familiar with the term “Forest bathing” or shinrin-yoku. In Japanese, Shinrin means “forest,” and yoku means “bath.” Shinrin-yoku means bathing in a forest atmosphere or taking in the forest through our senses.
Research has demonstrated that trips to the forest can not only make us feel better by lowering muscle tension, boosting sleep, and reducing blood pressure. It turns out being in nature also enhances our immune systems by increasing the number and activity of our lympocytes and killer T cells.
Phytoncides are Natures Immune Boosters
When we walk among trees and plants, we breathe in airborne chemicals from plants called phytoncides.
Plants produce these chemicals to protect themselves from insects, bacterial and fungal infections. Phytoncides help plants fight disease.
When people breathe in these phytoncides, our bodies respond by increasing the number and activity of a type of white blood cell called natural killer cells or NK.
These cells kill tumor and virus-infected cells in our bodies. In one study, increased NK activity from a 3-day, 2-night forest bathing trip lasted for more than 30 days.
Boost your immune system and state of mind.

According to Dr. Qing Li, author of the book, Forest Bathing, the key to unlocking the power of the forest is in the five senses:
- Let nature enter through your ears, eyes, nose, mouth, hands, and feet.
- Listen to the birds singing and the breeze rustling in the leaves of the trees.
- Look at the different greens of the trees and the sunlight filtering through the branches.
- Smell the fragrance of the forest and breathe in the natural aromatherapy of phytoncides.
- Taste the freshness of the air as you take deep breaths. Place your hands on the trunk of a tree.
- Dip your fingers or toes in a stream. Lie on the ground. Drink in the flavor of the forest and release your sense of joy and calm.
- This is your sixth sense, a state of mind. Now you have connected with nature. You have crossed the bridge to happiness.
To read more, click here.
Surviving the Holidays – 10 Steps to Success

The holiday season can also be stressful and throw us off our normal routine. This can compromise our sleep and our overall eating habits.
To help everyone feel their best during this holiday season, we have ten strategies for you and your patients. And even if you can’t do all ten, just pick one or a few that you feel you can commit to and succeed with most of the time.
We have created a 10 Steps to Survive the Holidays PDF – a handout that includes the info below to print and share with your friends, patients, and colleagues!
COVID & Diabetes Update – Navigating a Crisis
COVID & Diabetes Update
Navigating a Crisis
Recorded & Ready for Viewing
Coach Beverly Thomassian, RN, MPH, CDCES, BC-ADM, has completely updated this critical presentation, to bring health care professionals up-to-date on the current state of COVID and its impact on diabetes care. She summarizes key information including critical teaching points and management strategies for people with diabetes who develop a COVID-19 infection.
Topics Include:
- Discuss the current state of diabetes in the United States.
- Describe the relationship between COVID and health care disparities
- Explore the impact of COVID infection on those with pre-existing diabetes.
- Discuss treatment strategies for COVID and diabetes, including new vaccines.
- List critical teaching points for people with diabetes and COVID.
Join us to learn critical information about Diabetes and COVID Management

Instructor: Beverly Thomassian RN, MPH, CDCES, has been Board Certified in Advanced Diabetes Management for over 20 years. She is an Associate Clinical Professor at UCSF and Touro University and a nationally recognized diabetes expert.
FREE Resource Catalog

- Diabetes Cheat Sheets
- Diabetes Blog Bytes
- Medication PocketCards
- Start Your Certification Journey
- CDCES Coach App
- Free Webinars hosted by Coach Beverly
- Question of the Week
See Full Free Resource Catalog
Sign up for Diabetes Blog Bytes – we post one daily Blog Byte from Monday to Friday. And of course, Tuesday is our Question of the Week. It’s Informative and FREE! Sign up below!
[yikes-mailchimp form=”1″]Accreditation: Diabetes Education Services is an approved provider by the California Board of Registered Nursing, Provider 12640, and Commission on Dietetic Registration (CDR), Provider DI002. Since these programs are approved by the CDR it satisfies the CE requirements for the CDCES regardless of your profession.*
The use of DES products does not guarantee the successful passage of the CDCES exam. CBDCE does not endorse any preparatory or review materials for the CDCES exam, except for those published by CBDCE.
Happy World Diabetes Day
Today, November 14, is Dr. Banting’s Birthday
World Diabetes Day is celebrated in honor of Dr. Fredrick Banting, whose leadership, tenacity and belief led to the discovery of insulin.
The discovery of insulin has saved the lives of countless millions of people over the past hundred years and will continue to save millions of lives in the near future and beyond.
During a hot summer in 1921, Dr.Banting secured space to test out his theory at the University of Toronto. Along with his colleague, Charles Best, and a bare-bones lab, they conducted dozens of experiments on dogs, which ultimately led to the discovery of insulin.


Dr. Banting and Charles Best began their experiments ligating the pancreases of dogs, thinking this would prevent destruction by the digestive pancreatic juices, and then isolating the extract from the islet cells. They then processed the extract from the islet cells and injected this extract they called “insulin” into diabetic dogs. According to an audio interview with Dr. Best, by July 1921, they had 75 positive examples of insulin lowering blood glucose levels in dogs.

In February 1922, doctor Frederick Banting and biochemist John Macleod published their paper on the successful use of an alcohol-based pancreatic extract for normalizing blood glucose levels in a human patient.
Here are some photos of the first insulin bottles produced by the University of Toronto and Eli Lilly.
Soon, word of their discovery got out and the race was on to produce enough insulin to treat the flood of type 1 patients arriving in Toronto to receive this miracle injection.
But, as with any amazing discovery, there is always more to the story.
One of the biggest barriers to Banting was the simple fact that he was not involved in the field of diabetes research. The idea leading to the discovery of insulin came to him after preparing a lecture on the pancreas and diabetes, a subject he knew little about. He wasn’t a trained researcher and thus securing support for the project was initially difficult.
First Children to Receive Insulin
The first patient to receive insulin was a ‘welfare’ case at Toronto General Hospital – no clinical trial structure to say the least. People from Canada/US flooded into Toronto to receive treatment. Banting struggled with the lack of accessibility of insulin – volume needed issues of purification.
The earliest patients were “selected”, some youths from Canada/US, some soldiers with diabetes (probably because of Banting’s service in the First World War), and then later some select private patients. During this time they were working hard to increase the volume and continue to improve the purification process. Insulin was available for testing in the US, namely through Dr. Elliot Joslin in the late summer of 1922.
Takes a Team

While Best played a critical and important role, credit must also go to Professor Macleod, from the University of Toronto, who provided the lab space, showed Dr. Banting how to operate on dogs, provided his student Best and suggested they switch from saline to alcohol to purify the ‘extract’. Dr. Macleod also secured the support of JB Collip, the 4th man on the team, and the first person to purify insulin for human use. Best is also known for pushing Banting to return to the research during a particularly dark period of failure.
Dr. Banting – Fun and Interesting Facts
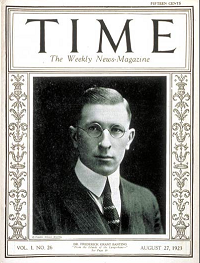
- Sold insulin patent for $1
- Was wounded during the First World War and received the Military Cross
- Youngest Nobel Laureate in Medicine
- First Canadian on the cover of Time Magazine
- Among the last Canadians to receive a knighthood and have the title, Sir Frederick Banting
- One of only two “non-Americans” to have a Second World War Liberty Ship named after him (USS Frederick Banting)
- Has as a crater on the Moon named after him (between Apollo 15 & 17 landing sites).
Want to Learn More About Dr. Banting?
Visit Banting House FaceBook Page
Sign up for Diabetes Blog Bytes – we post one daily Blog Byte from Monday to Friday. And of course, Tuesday is our Question of the Week. It’s Informative and FREE! Sign up below!
[yikes-mailchimp form=”1″]November Newsletter | You’re Invited to Celebrate Diabetes Month | 2 FREE Webinars

November is an exciting month. We celebrate National Diabetes Month and World Diabetes Day. Plus, we get to exercise our right to vote.
I love this quote by Sharon Salzberg, “Voting is the expression of our commitment to ourselves, one another, this country and this world.”
Ms. Salzberg’s expression is the perfect segue to this year’s Diabetes Month Celebration theme; Taking care of Youth with Diabetes. When we take care of children with diabetes, we are making a long-term commitment to our families, communities, and the future. Diabetes Specialists are natural advocates for children and families living with diabetes.
We are excited to share helpful resources to support you with ongoing advocacy, education, and emotional support for young people living with diabetes.
November also kicks off our holiday season extravaganza. Celebrating during a pandemic is going to present many challenging situations and awkward conversations around safety. To help out, we are sharing our Stress Management Strategies for the Holidays handout. Plus, our dietitian expert, Dawn DeSoto, bravely explores her personal story of stress and sugar overconsumption. She provides some delicious low sugar recipes to help ease us through the holidays.
Lastly, as part of our annual celebration, we are excited to invite you to two FREE Webinars. Diabetes Management in Tots to Teens and our Gut & Skin Microbiome Webinar. We will look into COVID and gut health plus explore some new science that might change our showering habits.
We are grateful for family and friends. We are thankful for each one of you and the message of hope you share with our diabetes community.
In health and gratitude,
Coach Beverly, Bryanna, and Jackson
Click here to read our full November newsletter.
Sign up for our newsletter
FREE Webinar – Getting to the Gut, Meet Your Microbiome airs November 9th at 11:15 am PST
Join the wonderment as we explore the role of our Microbiome.

“This Webinar is filled with Bev’s energy, knowledge, and passion for diabetes that she replicates in all her teachings. She puts a demand on herself to be a mentor to all. Her information is well organized, full of current/relevant research, and helps CDCES’ view into the future as a changing world impacts diabetics. I find her to be the most exciting and engaging educator and … OUTSTANDING teacher!!” – recent participant
This one-hour complimentary journey will expand your view of how the trillions of bacterial hitchhikers profoundly influence our health. We will discuss how foods, the environment, and our medical practices have impacted our gut bacteria over time and strategies we can take to protect these old friends.
Webinar topics:
- Discuss the latest research on our microbiome
- State the relationship between gut health and diabetes risk
- Describe 3 strategies to get our microbiome back to better health.
Sign up for Diabetes Blog Bytes – we post one daily Blog Byte from Monday to Friday. And of course, Tuesday is our Question of the Week. It’s Informative and FREE! Sign up below!
[yikes-mailchimp form=”1″]
Accreditation: Diabetes Education Services is an approved provider by the California Board of Registered Nursing, Provider 12640, and Commission on Dietetic Registration (CDR), Provider DI002. Since these programs are approved by the CDR it satisfies the CE requirements for the CDCES regardless of your profession.*
The use of DES products does not guarantee the successful passage of the CDCES exam. CBDCE does not endorse any preparatory or review materials for the CDCES exam, except for those published by CBDCE.









