Is Metformin associated with Low B12 levels?
Metformin is one of the most widely dispensed oral diabetes medications for good reason. It works great, lowering A1c 1-2% points, with an added benefit of dropping LDL cholesterol levels. It doesn’t cause hypoglycemia or weight gain and it is incredibly cheap. Many pharmacies offer a 3 month supply of this highly effective glucose-lowering medication for $10 or less, and that’s without insurance. This medication also seems to boost the diversity of the gut microbiota, in particularly increased levels of the very beneficial Akkermansia muciniphila.
However, it does have a few drawbacks. A small group of people on metformin will experience a B12 deficiency. This B12 deficiency may manifest as neuropathic pain or anemia.
Plus, a percentage of people will experience upset stomach, bloating, and diarrhea. People with these complaints will often respond better to the extended-release version (metformin XR), which isn’t any more expensive and it can be taken once a day. See our Mediation PocketCards for more info.
How prevalent is B12 Deficiency with metformin?

Currently, the ADA Standards have no clear recommendation for checking B12 for those on metformin, but it does note that long-term metformin use is associated with B12 deficiencies and that “measuring B12 levels should be considered for those with type 1 diabetes, peripheral neuropathy or unexplained anemia”.
To add to this, a study published this month in Human Nutrition and Metabolism, found the prevalence of B12 deficiency appears to be about 17% in people on metformin therapy. The highest rates of B12 deficiency were seen in those taking metformin for 2 years. Moreover, vitamin B12 deficiency is influenced by the occurrence and duration of diabetes.
They also measured the intake of vitamin B12 in the daily diet of the study participants. Those with lower vitamin B12 blood levels were also consuming less foods rich in vitamin B12 in their daily meal plan.
Recommendations for Regular B12 Monitoring and Replacement
The authors of this article suggest that routine monitoring for vitamin B12 serum levels is needed in people with T2DM, particularly when metformin is used for more than 2 years with a dose of over 1000 mg per day. They also recommend further studies are needed to assess the correlation between metformin duration and dose and patients with T2DM and other metabolic syndromes.
B12 replacement therapy
This article, nor the ADA Standards recommend dosing for B12 replacement therapy. However, based on several articles, including this 2005 Cochrane review, high-dose oral replacement (1 mg to 2 mg per day) for B12 deficiency, seems to be as effective as parenteral B12 administration for correcting anemia and neurologic symptoms.
Conclusion – Vitamin B12 deficiency is associated with worsening nerve pain and anemia. Testing B12 levels for those on long-term metformin therapy, especially for those taking more than 1000 mg of metformin a day seems like a reasonable approach. Increasing the intake of foods high in vitamin B12 and providing oral B12 replacement therapy of 1 mg to 2 mg a day, are both helpful interventions to boost B12 levels.
Resources from our Article Library
Plant Based Eating Resources and Recipes
Carbohydrate Counting Resource Page
Want to learn more about this topic? Enroll in our
Meds Management for Type 2 Standards | 1.5 CEs
Recorded & Ready to Watch!
Coach Beverly will highlight the key elements of the latest Medication Guidelines by AACE and ADA. We will explore clinical factors to consider when determining the best strategy to improve glucose management in people with type 2 diabetes and other co-conditions. There will be a special focus on cardiovascular risk reduction and renal protection.
Objectives:
- Describe the role of Diabetes Care and Education Specialists in stopping clinical inertia
- Discuss using the latest ADA and AACE Guidelines to determine the best therapeutic approach.
- Using the ADA and AACE Guidelines, describe strategies to initiate and adjust injectable therapy.
Enroll in the entire
Level 2 | Standards of Care Intensive Series | 20 CEs | $199
2022 Updates Airs March 17 – May 26, 2022
This bundle is specifically designed for healthcare professionals who want to learn more about the ADA Standards of Diabetes Care for their clinical practice or for those who are studying for the BC-ADM or the CDCES certification exam.
- Recorded on December 15, 2021 – Hyperglycemic Crises, DKA & HHS Standards | 1.0 CE
- Recorded on December 21, 2021 – Assessing and Promoting Well-Being: From Population Health to a Person-Centered Approach Standards | 1.5 CEs
- Recorded on February 3, 2022 – ADA Standards of Care | 2.0 CEs
- Recorded on March 17, 2022 – Setting up a Successful Diabetes Program 1.5 CEs
- Recorded on March 22, 2022 – Lower Extremity Assessment 1.5 CEs
- Recorded on March 24, 2022 – Meds Management for Type 2 – 1.5 CEs
- April 26, 2022 – Microvascular Complications, Eye, Kidney Nerve Disease 1.5 CEs
- April 28, 2022 – Critical Assessment of Diabetes Patient 2.0 CEs
- May 10, 2022 – Cardiovascular Disease and Diabetes Standards 1.5 CEs
- May 12, 2022 – Older Adults and DIabetes 1.5 CEs
- May 17, 2022 – Tots to Teens – Diabetes Standards 1.5 CEs
- May 19, 2022 – Pregnancy and Diabetes 1.5 CEs
- May 26, 2022 – Hospital and Hyperglycemia 1.5 CEs
Accreditation: Diabetes Education Services is an approved provider by the California Board of Registered Nursing, Provider 12640, and Commission on Dietetic Registration (CDR), Provider DI002. Since these programs are approved by the CDR it satisfies the CE requirements for the CDCES regardless of your profession.
The use of DES products does not guarantee the successful passage of the CDCES exam. CBDCE does not endorse any preparatory or review materials for the CDCES exam, except for those published by CBDCE.
Sign up for Diabetes Blog Bytes – we post one daily Blog Byte from Monday to Friday. And of course, Tuesday is our Question of the Week. It’s Informative and FREE! Sign up below!
[yikes-mailchimp form=”1″]The use of DES products does not guarantee the successful passage of the CDCES exam. CBDCE does not endorse any preparatory or review materials for the CDCES exam, except for those published by CBDCE.
From Med Updates to Successful DSME Programs | Webinars Begin March 17th
Join us for 3 exciting Webinars this month or sign up for our entire Level 2 Standards Bundle. As part of our Standards of Care Intensive, we take a deep dive into the content of each of the ADA Standards.
Setting up a Successful DSME Program Standards | Level 2 $29 | 1.5 CEs
Join us live Thursday March 17th at 11:30 am PST

Join us live on March 17, 2022, at 11:30 am PST for our Level 2 | Setting up a Successful DSME Program Standards live webinar
This course provides you with a succinct overview of the latest standards for Diabetes Self-Management Education (DSME) and Support Programs. If you are taking certification exams or considering setting up a DSME program, this program is designed for you. We highlight the newly revised and simplified 2022 Standards and provide strategies on program implementation. In addition, we discuss Medicare Reimbursement and covered benefits. This course provides insights into the exam philosophy and also highlights critical content areas.
Objectives:
- Describe DSME program examples from across the country.
- List the six standards for creating a successful DSME program
- Discuss marketing strategies for success
- Describe Medicare Reimbursement for diabetes care and education
Lower Extremity Assessment Standards | Level 2
$29 for 1.5 CEs
Join us live Tuesday March 22nd at 11:30 am PST
Join us live on March 22, 2022, at 11:30 am PST for our Level 2 | Lower Extremity Assessment Standards live webinar
People with diabetes are at increased risk of Lower Extremity Complications. This course reviews the steps involved in performing a detailed assessment of the lower extremities, including how to use a monofilament and tuning fork to detect neuropathy. We also discuss the significance of Ankle Brachial Index and strategies to prevent lower extremity complications.
Objectives:
- Describe the risk factors for lower extremity complications
- Discuss prevention strategies
- Demonstrate steps involved in a lower extremity assessment
Meds Management for Type 2 Standards | 1.5 CEs
Join us live Thursday March 24th at 11:30 am PST
Join us live on March 24, 2022, at 11:30 am PST for our Level 2 | Meds Management for Type 2 Standards live webinar
Coach Beverly will highlight the key elements of the latest Medication Guidelines by AACE and ADA. We will explore clinical factors to consider when determining the best strategy to improve glucose management in people with type 2 diabetes and other co-conditions. There will be a special focus on cardiovascular risk reduction and renal protection.
Objectives:
- Describe the role of Diabetes Care and Education Specialists in stopping clinical inertia
- Discuss using the latest ADA and AACE Guidelines to determine the best therapeutic approach.
- Using the ADA and AACE Guidelines, describe strategies to initiate and adjust injectable therapy.
Enroll in the entire
Level 2 | Standards of Care Intensive Series | 20 CEs | $199
2022 Updates Airs March 17 – May 26, 2022
This bundle is specifically designed for healthcare professionals who want to learn more about the ADA Standards of Diabetes Care for their clinical practice or for those who are studying for the BC-ADM or the CDCES certification exam.
- Recorded on December 15, 2021 – Hyperglycemic Crises, DKA & HHS Standards | 1.0 CE
- Recorded on December 21, 2021 – Assessing and Promoting Well-Being: From Population Health to a Person-Centered Approach Standards | 1.5 CEs
- Recorded on February 3, 2022 – ADA Standards of Care | 2.0 CEs
- March 17, 2022 – Setting up a Successful Diabetes Program 1.5 CEs
- March 22, 2022 – Lower Extremity Assessment 1.5 CEs
- March 24, 2022 – Meds Management for Type 2 – 1.5 CEs
- April 26, 2022 – Microvascular Complications, Eye, Kidney Nerve Disease 1.5 CEs
- April 28, 2022 – Critical Assessment of Diabetes Patient 2.0 CEs
- May 10, 2022 – Cardiovascular Disease and Diabetes Standards 1.5 CEs
- May 12, 2022 – Older Adults and DIabetes 1.5 CEs
- May 17, 2022 – Tots to Teens – Diabetes Standards 1.5 CEs
- May 19, 2022 – Pregnancy and Diabetes 1.5 CEs
- May 26, 2022 – Hospital and Hyperglycemia 1.5 CEs
Virtual DiabetesEd Specialist Conference
30+ CEs | April 13-15, 2022

Whether you are new to diabetes or a seasoned expert, you’ll benefit from this virtual conference with the latest research plus critical content that you can immediately apply to your clinical practice.
If you are seeking a state-of-the-art review of current diabetes care, this course is for you. Our team has been fine-tuning this course for over fifteen years, and we know what you need. This program can also be a great addition to your CDCES or BC-ADM exam study plan.
Join us LIVE for this Virtual Course and enjoy a sense of community!
Team of expert faculty includes:
- Diana Isaacs, PharmD, BCPS, BC-ADM, BCACP, CDCES – Educator of the Year, 2020
- Coach Beverly Thomassian, RN, MPH, CDCES, BC-ADM
- Ashley LaBrier, MS, RD, CDCES, Diabetes Program Coordinator
Two Registration Options
Virtual DiabetesEd Specialist Conference Deluxe | 30+ CEs
Deluxe Option for $499: Virtual Program includes:
- Q & A Session with the instructor after each webinar.
- LIVE Presentations by our team of experts.
- State of the art review of current diabetes care and technology.
- Resources for each session.
- Access to free podcasts and video recordings within a week of each live session for one year.
Deluxe Version includes Syllabus, Standards and Swag*:
- Diabetes Educator Course 2022 Syllabus Hard Copy – over 100 pages -This spiral-bound workbook contains the printed version of all of the instructor’s slides.
- ADA 2022 Standards of Care Book -The ADA Standards of Medical Care in Diabetes is a key resource for healthcare professionals involved in diabetes care, education, and support.
- DiabetesEd Services highlighters, Medication PocketCard, Tote Bag and Pen
Virtual DiabetesEd Specialist Conference Basic | 30+ CEs
Deluxe Option for $499: Virtual Program includes:
- Q & A Session with the instructor after each webinar.
- LIVE Presentations by our team of experts.
- State of the art review of current diabetes care and technology.
- Resources for each session.
- Access to free podcasts and video recordings within a week of each live session for one year.
2022 Live Webinar Events
See Full Calendar for upcoming webinars and Virtual Courses.
Can’t make it live? All paid registrants are guaranteed access to the video presentation, handouts and podcasts.
Accreditation: Diabetes Education Services is an approved provider by the California Board of Registered Nursing, Provider 12640, and Commission on Dietetic Registration (CDR), Provider DI002. Since these programs are approved by the CDR it satisfies the CE requirements for the CDCES regardless of your profession.
The use of DES products does not guarantee the successful passage of the CDCES exam. CBDCE does not endorse any preparatory or review materials for the CDCES exam, except for those published by CBDCE.
Concentrated Insulin and GFR Guidelines for SGLT2s
Did you know that Toujeo U-300 insulin pens are good for 56 days once opened? And that the max dose for Tresiba U-200 FlexTouch Pen is 160 units?
For our latest version of our printed PocketCards, we now include the number of pens in a box, max injection dose, total insulin amount per pen, and shelf life on the Concentrated Insulin Card. We also added Lyumjev KwikPen u200 insulin.
When determining the best insulin for people taking concentrated insulins, shelf life, max dosing, and total units of insulin in each device are important considerations.
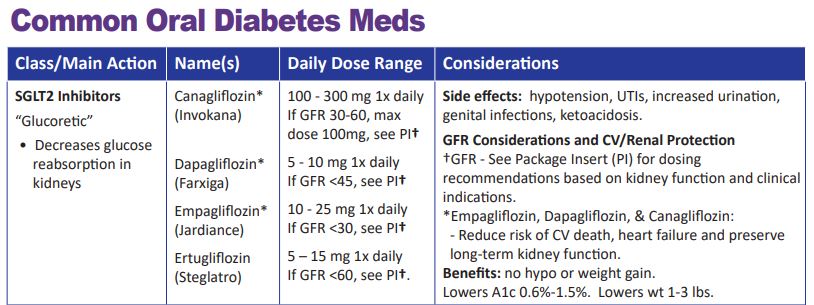
We have also updated the GFR parameters for SGLT2 Inhibitors. This class of medication not only substantially lowers blood glucose but also has a profound impact on renal protection.
As more trial data become available, the GFR cutoff levels may change, so periodically refer to the package insert (PI) or our DES electronic pocket care version, for the most up-to-date information.
We update the printed version of our PocketCard once or twice a year.
We update our electronic PocketCard on an ongoing basis.
Fortunately, we can immediately update our electronic version of the PocketCard on our website and CDCES Coach App to reflect the latest medication recommendations and guidelines. In the electronic version, we also include that the GLP-1 Exenatide (Bydureon) is now approved for peds, age 10 and older and the GFR cut-off for empagliflozin is now approved for a GFR 30 or greater (please see package insert for details).
Preparing for the BC-ADM Exam Free Webinar – What you need to know

Becoming Board Certified in Advanced Diabetes Management (BC-ADM) provides an opportunity for diabetes specialists with an advanced degree in their field (plus a professional license as an advanced practice nurse, registered dietitian, registered pharmacist, or provider) to increase the breadth and depth of their diabetes knowledge. The scope of advanced diabetes practice includes management skills such as medication adjustment, medical nutrition therapy, exercise planning, counseling for behavior management, and psychosocial issues.
Attaining optimal diabetes management includes using a person-centered approach coupled with assessment, screening, management, and monitoring of acute and chronic diabetes co conditions. This webinar will review changes in requirements for this year’s exam eligibility and test format, strategies to succeed along with a review of study tips and test-taking tactics. We will review sample test questions and the reasoning behind choosing the right answers. We hope you can join us for this webinar.
See Full Calendar for upcoming webinars and Training Conferences.
Can’t make it live? All paid registrants are guaranteed access to the video presentation, handouts and podcasts.
Sign up for Diabetes Blog Bytes – we post one daily Blog Byte from Monday to Friday. And of course, Tuesday is our Question of the Week. It’s Informative and FREE! Sign up below!
[yikes-mailchimp form=”1″]Accreditation: Diabetes Education Services is an approved provider by the California Board of Registered Nursing, Provider 12640, and Commission on Dietetic Registration (CDR), Provider DI002. Since these programs are approved by the CDR it satisfies the CE requirements for the CDCES regardless of your profession.
The use of DES products does not guarantee the successful passage of the CDCES exam. CBDCE does not endorse any preparatory or review materials for the CDCES exam, except for those published by CBDCE.
Diabetes Medication approved for Kids
The Food and Drug Administration (FDA) just approved another GLP-1 RA for use in children ages 10-17 with diabetes.
The injectable extended-release exenatide (Bydureon) is now the second glucagonlike peptide-1 receptor agonist (GLP-1 RA) approved for use in pediatric type 2 diabetes and the first with once-weekly administration. Liraglutide (Victoza) a daily injectable GLP-1 RA received approval for pediatric use in 2019 and metformin an oral biguanide has long been FDA approved for use children ten and older with type 2 diabetes.
During the annual scientific sessions of the American Diabetes Association, speakers expressed alarm about the rise in youth developing type 2 diabetes, noting that the condition typically progresses more rapidly and is less likely to respond well to metformin, compared with adults.
The approval was based on a 24-week, double-blind, placebo-controlled study in 82 children with type 2 diabetes aged 10 and older. They were randomized to 2 mg once-weekly exenatide extended release or placebo. At week 24, hemoglobin A1c in those randomized to the drug had dropped by 0.25 percentage points, compared with a 0.45 percentage point increase in the placebo group.
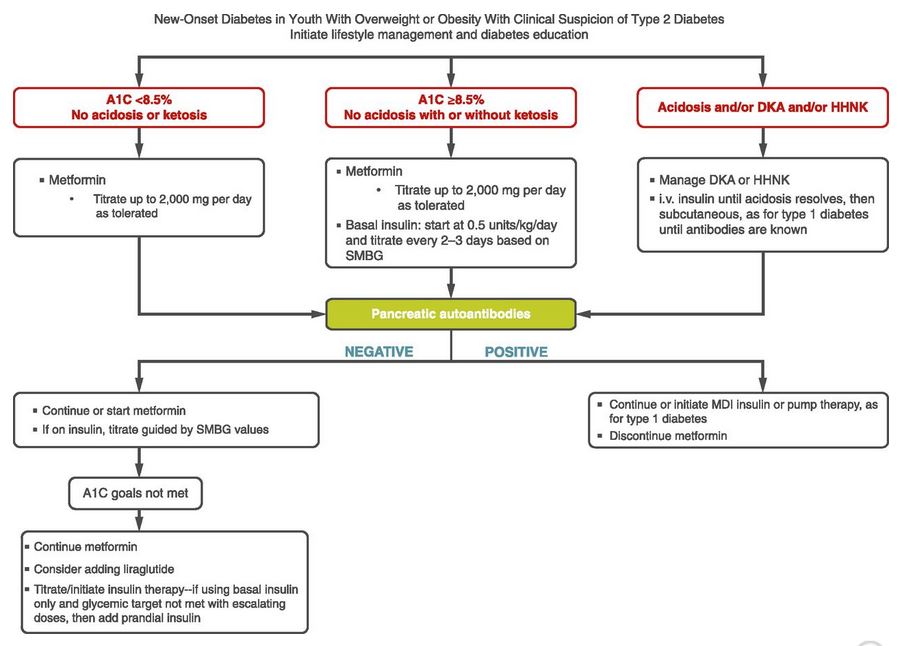
Based on the ADA Standards of Care for treating pediatrics with diabetes, the first treatment includes weight loss and exercise plus first line medications metformin and insulin if A1c is 8.5% or greater.
Furthermore, the initiation of any GLP-1 RA is only recommended once pancreatic antibodies are determined to be absent and if A1c goals have not met despite the initiation of metformin or insulin (see ADA standards algorithm below stating consider adding liraglutide (GLP-1 RA))
We have updated the electronic version of our Injectable PocketCard to reflect this update.
Download our Medication PocketCards today on our Website PocketCards , or CDCES Coach App (free).
Want to learn more about this topic and more?
Enroll in our Virtual DiabetesEd Specialist Program!
Did you miss the live conference? No worries! You can register now to watch on-demand
Whether you are new to diabetes or a seasoned expert, you’ll benefit from this virtual conference with the latest research plus critical content that you can immediately apply to your clinical practice.
If you are seeking a state-of-the-art review of current diabetes care, this course is for you. Our team has been fine-tuning this course for over fifteen years, and we know what you need. This program can also be a great addition to your CDCES or BC-ADM exam study plan.
Team of expert faculty includes:
- Diana Isaacs, PharmD, BCPS, BC-ADM, BCACP, CDCES – Educator of the Year, 2020
- Coach Beverly Thomassian, RN, MPH, CDCES, BC-ADM
- Ashley LaBrier, MS, RD, CDCES, Diabetes Program Coordinator
In addition to informative lectures, we also use group activities and case studies to highlight the essential knowledge, skills, and strategies needed to succeed in diabetes education today!

CEs: Includes over 30 CEs
Program Info: 2021 Diabetes Educator Course Flyer & Schedule (subject to change)
Speakers: View Conference Faculty.
Dates: Your registration fee includes access to FREE podcast and all recorded webinars for one year.
Two Registration Options
Virtual DiabetesEd Specialist Conference Deluxe | Oct. 6-8 | 30+ CEs
Deluxe Virtual Program for $459 includes:
- Presentations by our team of experts
- Q & A Session with the instructor after each webinar
- State-of-the-art review of current diabetes care and technology.
- Resources for each session
- Access to FREE podcast and recorded webinars within a week of each live session for one full year.
+Plus Syllabus, Standards and Swag:
- Diabetes Educator Course 2021 Syllabus Hard Copy – over 100 pages -This spiral-bound workbook contains the printed version of all of the instructor’s slides.
- DiabetesEd Services highlighters, Medication PocketCard and Pen
2021 Diabetes Educator Course Flyer & Schedule (subject to change)
Virtual DiabetesEd Specialist Conference Basic | Oct. 6-8 | 30+ CEs
Basic virtual program for $359 includes:
- Presentations by our team of experts
- Q & A Session with the instructor after each webinar
- State-of-the-art review of current diabetes care and technology.
- Resources for each session
- Access to FREE podcast and recorded webinars within a week of each live session for one full year.
2021 Diabetes Educator Course Flyer & Schedule (subject to change)
Team of Experts: Our team of expert faculty has been fine-tuning this course for over fifteen years and we know what you need to succeed! In addition to informative lectures, we also use group activities and case studies to highlight the essential knowledge, skills, and strategies needed to succeed in diabetes education today!
Bonus Courses worth 12+ CEs, FREE
When you register for our Virtual Course, you have immediate access to these Bonus DiabetesEd University Online Courses – for FREE!
- Test Taking Toolkit – Over 200 sample test questions!
- Level 2 – Assessing and Promoting Well-Being: From Population Health to a Person-Centered Approach 1.5 CEs
- Level 2 – Hospital and Hyperglycemia 1.5 CEs
- Level 2 – Hyperglycemic Crisis, DKA and HHS Standards 1.0 CEs
- Level 2 – Meds Management Update for Type 2 – 1.5 CEs
- Level 2 – Setting up a Successful Diabetes Program 1.5 CEs
- Level 2 – Pregnancy and Diabetes 1.5 CEs
- Level 2 – From Tots to Teens – Diabetes Standards 1.5 CEs
- Level 2 – Older Adults and Diabetes 1.5 CEs
- Mindfulness and Compassion in the Diabetes Encounter – 1.0 CE
2021 Diabetes Educator Course Flyer & Schedule (subject to change)
Sign up for Diabetes Blog Bytes – we post one daily Blog Byte from Monday to Friday. And of course, Tuesday is our Question of the Week. It’s Informative and FREE! Sign up below!
[yikes-mailchimp form=”1″]Accreditation: Diabetes Education Services is an approved provider by the California Board of Registered Nursing, Provider 12640, and Commission on Dietetic Registration (CDR), Provider DI002. Since these programs are approved by the CDR it satisfies the CE requirements for the CDCES regardless of your profession.*
The use of DES products does not guarantee the successful passage of the CDCES exam. CBDCE does not endorse any preparatory or review materials for the CDCES exam, except for those published by CBDCE.
New Lipid and Kidney Protection Meds Approved

Since heart disease is the leading cause of death in people with diabetes, these new treatment options including PCSK9 Inhibitors and ACL Inhibitors, offer hope of decreasing cardiovascular mortality and morbidity. In addition rates of Chronic Kidney Disease (CKD) rates are rising worldwide and people with diabetes account for the majority of people receiving treatment for end-stage renal disease.
The new nonsteroidal Selective Mineralcorticoid Antagonists reduce the risk of kidney function decline and failure, plus reduce risk of cardiovascular death. We asked our PharmD experts to update our Cheat Sheets with the latest info and provide a summary of these medication classes, action and considerations. Special thanks to our contributing experts Diana Isaacs, PharmD, BCPS, BCACP, BC-ADM, CDCES, FADCES, FCCP and Kristapor Thomassian, PharmD, BCPS.
Download Updated Cheat Sheets Here
Medication Update Summary
PCSK9 Inhibitors (proprotein convertase subtillisin / kexin type 9)
- Alirocumab (Profluent)
- Evolocumab (Repatha)
This class of drugs are monoclonal antibodies designed to bind to the PCSK9 enzyme in the liver. PCSK9 enzyme is involved in inactivating LDL receptors, resulting in continued high levels of LDL circulating in the blood. The PCSK9 inhibitors (monoclonal antibodies) bind to the enzyme and increase the LDL receptors, helping reduce circulating LDL in the blood by appropriately metabolizing LDL in the liver.
There are specific FDA approved indications for this class of medications. Please refer to appropriate guidelines to determine if the individual meets criteria for agents in this class for treatment.
ACL Inhbitor (Adenosine Triphosphte-citrate Lyase)
- Bempedoic acid
This class of drug is designed to bind to the ATP-citrate Lyase enzyme. The ATP-citrate Lyase enzyme is the one of the initial enzymes involved in Cholesterol synthesis. Statins are the main class of agents we currently use to help block the HMG-CoA reductase enzyme, one of the primary enzymes involved in cholesterol production. The ACL inhibitor works upstream on the same cascade to help reduce cholesterol production, to achieve additional LDL lowering.
Nonsteroidal Selective Mineralocorticoid Receptor Antagonist
- Finerenone (Kerendia)
This class of drug is designed to bind to the Mineralocorticoid receptor. Mineralocorticoid receptors are found in regions most important for regulating electrolytes like sodium and potassium in key organs such as the kidney, heart and brain. Reducing the progression of chronic kidney disease (CKD) is one of our most important goals in keeping preventing end stage renal disease and CB events. Excess aldosterone production, the primary steroid based mineralocorticoid found in our bodies, has been implicated in nephrololgy and cardiovascular pathophysiology. The mineralocorticoid receptor antagonist blocks the effects of aldosterone and reduces the risk of kidney function decline as well as heart failure.
Download Updated Cheat Sheets Here
First Interchangeable Biosimilar Insulin Approved
Semglee (insulin glargine-yfgn) is a biosimilar basal insulin with the same chemical composition as insulin glargine. However, since it is a biosimilar, it is a less costly version of this widely popular basal insulin. Up until now, pharmacists could not make “pharmacy-level substitution”—much like how generic drugs are substituted for brand name drugs, without provider approval.
With this new FDA approval, an interchangeable biosimilar product may be substituted for the reference product without the intervention of the prescriber. Biosimilars marketed in the U.S. typically have launched with initial list prices 15% to 35% lower than comparative list prices of the reference products.

Bottom line, the pharmacist can now interchange or substituted semglee for its reference product Lantus (insulin glargine) without prescriber approval.
“This is a momentous day for people who rely daily on insulin for treatment of diabetes, as biosimilar and interchangeable biosimilar products have the potential to greatly reduce health care costs,” said Acting FDA Commissioner Janet Woodcock, M.D.
This also has implications for future, lower cost biosimilars says Dr. Woodcock. “Today’s approval of the first interchangeable biosimilar product furthers FDA’s longstanding commitment to support a competitive marketplace for biological products and ultimately empowers patients by helping to increase access to safe, effective and high-quality medications at potentially lower cost.”
Semglee (insulin glargine-yfgn), offered in 10 mL vials and 3 mL prefilled pens, is administered subcutaneously once daily.
Access to affordable insulin is critical and the approval of this first biosimilar heralds good news for future biosimilar interchangeability.
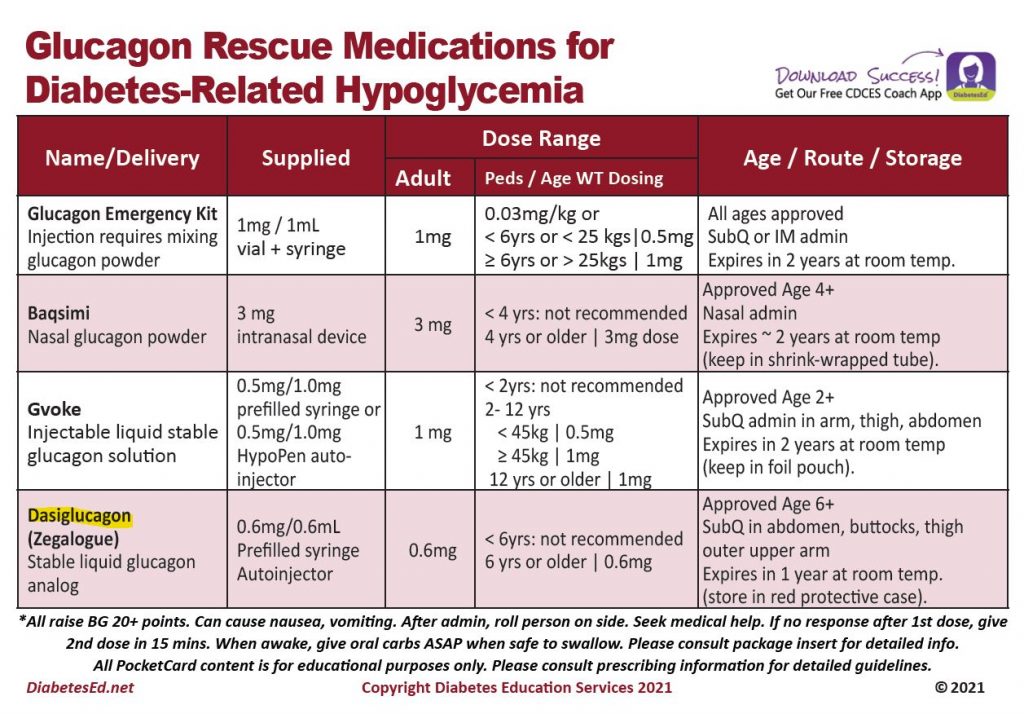
New Glucagon Rescue Med Approved
A new aqueous glucagon analog formulation has been FDA approved and should be available in pharmacies later this year.
Dasiglucagon (Zegalogue) is an effective, reliable treatment to increase glucose levels following insulin-induced hypoglycemia in children and adolescents with type 1 diabetes. This conclusion is based on a double-blind study recently published in Diabetes Care, April 2021.
This ready-to-use, next-generation formulation is approved for ages 6 or older. Subcutaneous injection sites include the abdomen, buttocks, thighs, and upper arms. This prefilled syringe contains a stable liquid glucagon analog and can be stored for one year at room temperature.
The investigators report that dasiglucsagon treatment was well tolerated, with the usual adverse effects (nausea and vomiting) expected from glucagon treatment.
The dose of dasiglucagon is 0.6 mg to treat severe hypoglycemia in pediatrics over the age of 6 years and adults with diabetes. Download our Glucagon PocketCard to post and share with colleagues and people living with diabetes.
Keeping It Safe
As with all glucagon injections, dasiglucagon can cause nausea and vomiting. After the dose is administered, roll the person on the side and seek medical help. When awake, give oral carbohydrates ASAP when safe to swallow, and consult package insert for detailed guidelines!
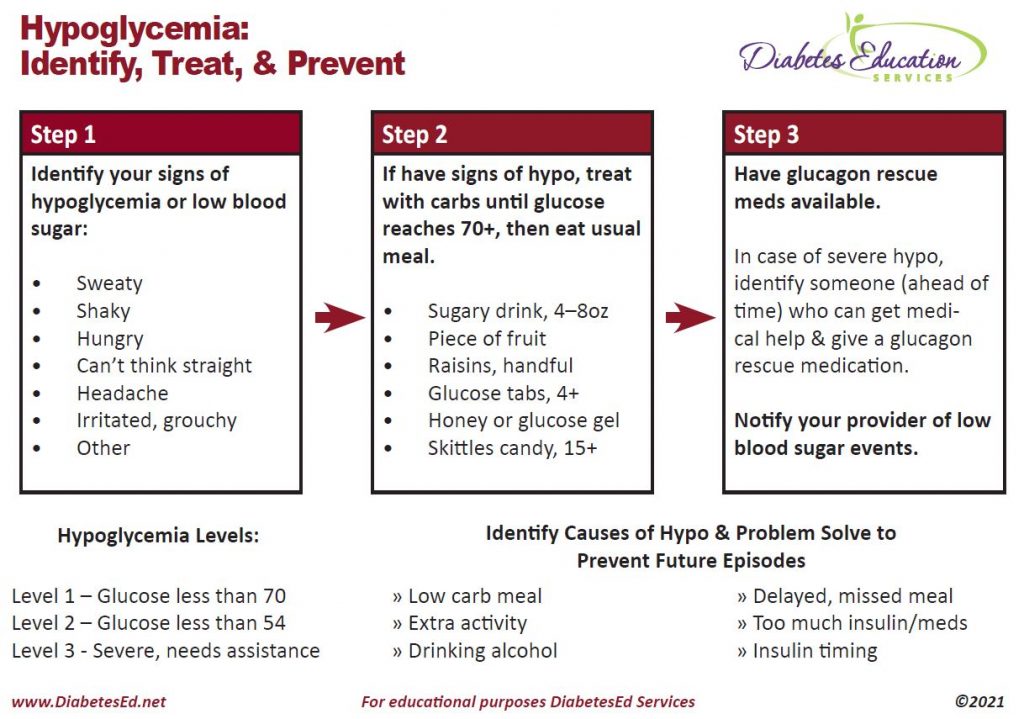
Preventing Future Episodes of Hypoglycemia
Most importantly, encourage people experiencing a severe low blood sugar to determine the cause of the hypoglycemic event and implement strategies to prevent future lows. Our free Glucagon Card is the perfect teaching tool to help reinforce prevention and early action!
Saving lives
Thank you for helping get the word out about these rescue medications for severe hypoglycemia. This hormone injection saves lives and is a must-have for anyone living with type 1 diabetes or those with type 2 on intensive insulin therapy.
Want to learn more about this topic? Join us for our
Level 4 | Solving Glucose Mysteries for Type 1 | 1.5 CEs | Recording & Ready for Viewing!

Why do the blood sugars keep dropping after meals? Is the basal insulin set correctly? What adjustments are needed for exercise?
During this 60 -90 minute webinar Coach, Beverly addresses each of these glucose mysteries and more, using a person-centered approach. She describes a stepwise approach to evaluate glucose patterns and correct common issues encountered by people living with type 1 diabetes.
By attending this webinar, you will gain confidence in evaluating glucose patterns and making recommendations for improvement.
Objectives
- Describe common glucose mysteries encountered by people with type 1 diabetes.
- Using a stepwise approach, evaluate factors affecting glucose patterns.
- State interventions to increase time-in-range and improve quality of life.
Join us for our Live Webinars
Including Brand New Specialty Courses!
Can’t join live? No worries, we will record the webinar and post it to the Online University!
Sign up for Diabetes Blog Bytes – we post one daily Blog Byte from Monday to Friday. And of course, Tuesday is our Question of the Week. It’s Informative and FREE! Sign up below!
[yikes-mailchimp form=”1″]Accreditation: Diabetes Education Services is an approved provider by the California Board of Registered Nursing, Provider 12640, and Commission on Dietetic Registration (CDR), Provider DI002. Since these programs are approved by the CDR it satisfies the CE requirements for the CDCES regardless of your profession.*
The use of DES products does not guarantee the successful passage of the CDCES exam. CBDCE does not endorse any preparatory or review materials for the CDCES exam, except for those published by CBDCE.
Steroids, Sugar Spikes and Management Strategies
JR is 64 years old, in hospital with type 2 diabetes and COVID. JR normally manages their diabetes with metformin, but during this inpatient stay, JR is on prednisone therapy which has spiked sugar levels into the 250 mg/dl to 350 range. JR is receiving bolus insulin sliding scale with meals and bedtime glargine, but blood sugars are persistently elevated. To improve outcomes for JR, it is important to keep blood glucose levels less than 180 mg/dl, but what should we recommend to get glucose to goal?
What are some strategies to get blood sugar to target while on steroids?
There is no consensus on the best approach to manage this situation. Up until this point in history, steroid-induced hyperglycemia was mostly found in people with diabetes in COPD, those undergoing chemotherapy or in post-transplant situations.

Oral Meds plus an Old Friend
With the COVID pandemic, many people with diabetes in hospitals and at home, are on steroids. Health care professionals are trying to figure out how to lower glucose levels.
For people with type 2 diabetes and COVID, the latest research indicates that sitagliptin (Januvia) not only helps maintain blood glucose but also decreases the inflammatory response associated with COVID infections. If not contraindicated, sitagliptin can be used in conjunction with insulin, to treat the extreme insulin resistance and hyperglycemia caused by steroid therapy.
To treat steroid induced hyperglycemia, we are going to call on our old insulin friend, NPH. Neutral Protamine Hagedorn (NPH) is an intermediate acting basal insulin. NPH insulin is made by mixing regular insulin and protamine in exact proportions with zinc and phenol such that a neutral-pH is maintained and crystals form.
NPH insulin’s peak action time matches steroid’s action time
NPH insulin is cloudy and has an onset of 1–4 hours. Its peak is 6–10 hours and its duration is about 10–16 hours.
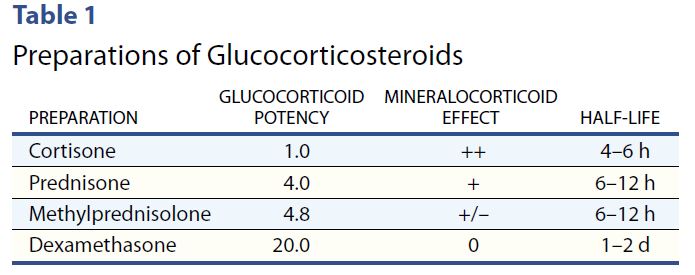
Steroids have their highest potency at 4-12 hours, with the exception of the very potent dexamethasone, which has a half life of 1-2 days.
However, with all steroids, including dexamethasone, people will experience elevated glucose values after breakfast, lunch, dinner, and at bedtime but will have a significant drop toward normal glucose overnight.
Therefore, hyperglycemia is greatest 1–2 hours after a meal, with persistent elevation until the following meal, followed by a return to normal overnight.

NPH Insulin Dosing Strategies
There are several articles (see below) that recommend a variety of NPH dosing strategies. Generally, insulin dosing is based on a combination of steroid dose and body weight. For those on lower dose steroid (ie less than 40 mg prednisone daily) a starting NPH insulin dose of 0.1 – 0.2 units per kg is reasonable. If JR weighs 100 kg, that means 10 to 20 units of NPH daily.
If JR is on a higher steroid dose, or blood sugars are extremely elevated, JR may need 0.3 units/kg or 30 units of NPH daily. Of course, we also need to keep nutritional status in mind as we determine best dose. People who are not eating or NPO, will require less insulin, even in the presence of steroids.
The timing of NPH administration matches the timing of the steroid therapy.
In addition, coverage for carbohydrates at meals and correction insulin bolus for hyperglycemia can help prevent post-prandial hyperglycemia.
A simple getting started strategy – 70/30 Insulin
A simple strategy I have used over many years, that I find safe and effective, is giving the basal-bolus premixed 70/30 insulin with the morning dose of steroid. A safe starting range is around 10 units in the morning and gradually increases 10-20% daily to get glucose to target. In addition, bolus coverage for carbs and hyperglycemia can be given at lunch and dinner.
Since blood sugars trend down overnight, nighttime NPH insulin is not usually needed.
Keeping it flexible
As the person starts recovering and steroid doses are gradually tapered down, it is important to also decrease the NPH insulin dose and bolus insulins to prevent hypoglycemia.
In conclusion:
Keeping blood sugars on target improves outcomes. For people with diabetes, steroids can cause a hyperglycemic crisis. Thoughtful and progressive management using NPH and bolus insulins can turn the tide and help get blood glucose levels to goal.
Join Coach Beverly at our Virtual Conference for more information on COVID and Diabetes Management Strategies.
Reference Articles
Glycemic Control in Hospitalized Patients with Diabetes Receiving Corticosteroids Using a Neutral Protamine Hagedorn Insulin Protocol: A Randomized Clinical Trial. Khowaja A, Alkhaddo JB, Rana Z, Fish L. Diabetes Ther. 2018 Aug;9(4):1647-1655.
How to Manage Steroid Diabetes in the Patient With Cancer
David S. Oyer, MD, FACE, Ajul Shah, BS, and Susan Bettenhausen, APRN, CDE, 2006
Virtual DiabetesEd Specialist Course
Earn 30+ CEs | April 15-17, 2021
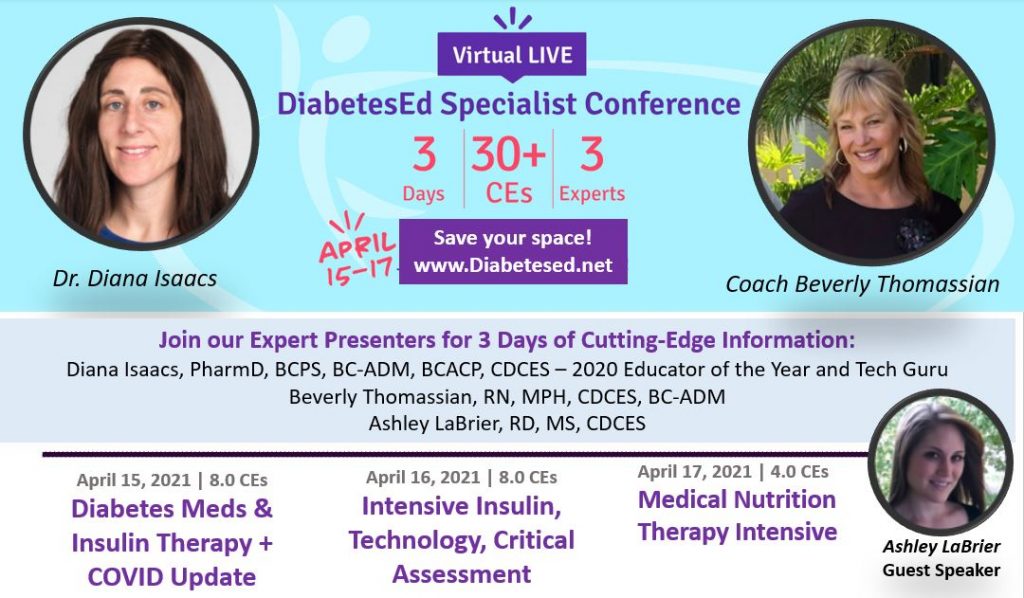
Virtual DiabetesEd Specialist Program
Whether you are new to diabetes or a seasoned expert, you’ll benefit from this virtual conference with the latest research plus critical content that you can immediately apply to your clinical practice.
DiabetesEd Virtual Conference Flyer 2021
Diabetes Ed Virtual 3-Day Schedule 2021
Prepare for CDCES or BC-ADM certification or earn hours for renewal.
If you are interested in taking the CDCES or BC-ADM exam or are seeking a state of the art review of current diabetes care, this course is for you. Our team has been fine-tuning this course for over fifteen years, and we know what you need.
Can’t join live? No worries, your registration guarantees access to the recorded content through Dec 31, 2021!
Team of expert faculty includes:
- Diana Isaacs, PharmD, BCPS, BC-ADM, BCACP, CDCES – Educator of the Year, 2020
- Coach Beverly Thomassian, RN, MPH, CDCES, BC-ADM
- Ashley LaBrier, MS, RD, CDCES, Diabetes Program Coordinator
In addition to informative lectures, we also use group activities and case studies to highlight the essential knowledge, skills, and strategies needed to succeed in diabetes education today!
Your registrations include access to all the Online Sessions plus Bonus Courses through December 31st, 2021.