Virtual DiabetesEd Specialist Conference
Reserve your spot now for our
Virtual DiabetesEd Specialist Conference | April 15-17, 2021

Whether you are new to diabetes or a seasoned expert, you’ll benefit from this virtual conference with the latest research plus critical content that you can immediately apply to your clinical practice.
Entire Program Fee: $399
Dates: April 15-17, 2021
Live Webinar Schedule: All webinars start and end times are in Pacific Standard Time
DiabetesEd Virtual Conference Flyer 2021
Diabetes Ed Virtual 3-Day Schedule 2021
Team of Experts & Schedule
Coach Beverly Thomassian, RN, MPH, BC-ADM, CDCES

Author, Nurse, Educator, Clinician and Innovator, Beverly has specialized in diabetes management for over twenty years. As president and founder of Diabetes Educational Services, Beverly is dedicated to optimizing diabetes care and improving the lives of those with diabetes.
Diana Isaacs, PharmD, BCPS, BC-ADM, BCACP, CDCES

We are thrilled to welcome our newest speaker, Diana Isaacs, who will be joining our Virtual and Live Courses!
Dr. Isaacs was named 2020 AADE Diabetes Educator of the Year for her educational platform promoting the use of CGM for people with diabetes and other innovations. Dr. Isaacs was awarded the Ohio Pharmacists Association Under 40 Award in 2019. Dr. Isaacs has served in leadership roles for several pharmacies and diabetes organizations. She has numerous diabetes publications and research projects with a focus on medications, CGM and diabetes technology.
As the CGM Program Coordinator and clinical pharmacist specialist in the Cleveland Clinic Diabetes Center, Dr. Isaacs brings a wealth of clinical knowledge combined with extensive research experience to this program.
Diabetes Meds and Insulin Toolkit – with Dr. Diana Isaacs | 4.0 CEs
April 15 10:30 am – 12:30 BREAK and 1:15 – 3:15 PST
*Topics include:
- Diabetes Medications, What Diabetes Specialists Need to Know
- Update on the latest medication information
- How to put ADA and AACE Algorithms into practice
- Critical teaching points with a focus on safety
- Insulin – The Ultimate Hormone Replacement Therapy
- Latest update on available insulins
- How to use ADA algorithm for insulin management
- Teaching pointers for safe and effective insulin use
Technology Toolkit with CV Management Update – Dr. Diana Isaacs | 4.0 CEs –
April 16 with 8:30—12:30 am
- Intensive Insulin Therapy— From Carbs to Correction to reach glucose targets
- Formulas on determining insulin coverage for carbs and hyperglycemia
- Using glucose results to evaluate effectiveness
- Integrating Technology, Continuous Glucose Monitoring and Insulin Pumps into care.
- Update on the latest technology, from meters to CGM with an emphasis on problem solving.
- Delivering insulin, from pens to pumps
- Understanding glucose reports and determining best action
- CV Risk Management with a Pharmacology Focus
- Apply the ADA guidelines to improve CV outcomes
- Describe the preferred medication using a case study approach
Ashley LaBrier, MS, RD, CDCES

Ashley is an educator, dietitian, and the Diabetes Education Program Coordinator at the Salinas Valley Medical Clinic’s Diabetes & Endocrine Center. Her work with people living with diabetes focuses on the value of healthy nutrition and movement to improve well-being.
Ashley is passionate about providing person-centered education to empower those who live with diabetes. Having been diagnosed with type 1 diabetes herself nearly 20 years ago, she combines her professional knowledge with personal experience and understanding.
April 17 with Ashley LaBrier, MS, RD, CDCES
8:30 am — 12:30 pm PST
- Medical Nutrition Therapy Overview
- Meal Planning – How to Eat by the Numbers
- Keeping Well Through Activity and Nutrition
*Dates and times subject to change. Course start and end time are for Pacific Standard Timezone.
DiabetesEd Virtual Conference Flyer 2021
Diabetes Ed Virtual 3-Day Schedule 2021
Bonus Courses – Course registration includes FREE enrollment into our Level 2 Standard of Care Course Series including:
- Level 2 – Assessing and Promoting Well-Being: From Population Health to a Person-Centered Approach 1.5 CEs
- Level 2 – Hospital and Hyperglycemia 1.5 CEs
- Level 2 – Hyperglycemic Crisis, DKA and HHS Standards 1.0 CEs
- Level 2 – Meds Management Update for Type 2 – 1.5 CEs
- Level 2 – Pattern Management Gone Crazy 2.65 CEs
- Level 2 – Setting up a Successful Diabetes Program 1.5 CEs
- Level 2 – Women and Diabetes 1.5 CEs
- Level 2 – From Tots to Teens – Diabetes Standards 1.5 CEs
- Level 2 – From Tots to Teens – Diabetes Standards 1.5 CEs
- Level 2 – Older Adults and Diabetes 1.5 CEs
- Test Taking Toolkit
- Mindfulness and Compassion in the Diabetes Encounter – 1.0 CE
Team of expert faculty includes:
- Diana Isaacs, PharmD, BCPS, BC-ADM, BCACP, CDCES – Educator of the Year, 2020
- Coach Beverly Thomassian, RN, MPH, CDCES, BC-ADM
- Ashley LaBrier, MS, RD, CDCES, Diabetes Program Coordinator
In addition to informative lectures, we also use group activities and case studies to highlight the essential knowledge, skills, and strategies needed to succeed in diabetes education today!
Prepare for CDCES or BC-ADM certification or earn hours for renewal.
Your registrations include access to all the Online Sessions plus Bonus Courses through December 31st, 2021.
This virtual program includes:
3 day live webinar courses from April 15th-17th (20 CEs) + enrollment in our Bonus Bundle (14.0+ CEs) from now through December 2021.
- Live Q & A Session with the instructor after each webinar
- Presentations by our team of experts
- Handouts and Resources for each session
- Post-test questions
- A sense of community
- If you can’t attend the live webinars, a recorded version will be posted later the same day for viewing.
View full Conference Schedule and Faculty.
Sign up for Diabetes Blog Bytes – we post one daily Blog Byte from Monday to Friday. And of course, Tuesday is our Question of the Week. It’s Informative and FREE! Sign up below!
[yikes-mailchimp form=”1″]Accreditation: Diabetes Education Services is an approved provider by the California Board of Registered Nursing, Provider 12640, and Commission on Dietetic Registration (CDR), Provider DI002. Since these programs are approved by the CDR it satisfies the CE requirements for the CDCES regardless of your profession.*
The use of DES products does not guarantee the successful passage of the CDCES exam. CBDCE does not endorse any preparatory or review materials for the CDCES exam, except for those published by CBDCE.
Treating DKA with Sub-Q Insulin?
What are the treatment options for people with type 1 diabetes with a COVID infection hospitalized for Diabetes KetoAcidosis (DKA)?
The typical treatment for DKA is fluids coupled with an IV insulin drip. Given the frequent monitoring and ICU bed required for treatment of DKA with an insulin drip, there has been a renewed interest in treating DKA with subcutaneous or sub-q insulin.
But after doing some research, I discovered an excellent 2004 paper co-authored by Dr. Guillermo Umpierrez et al. on using Sub-Q Insulin to Treat DKA. After completing a study comparing treatment of DKA using sub-q insulin vs. insulin drip, the author’s conclude that sub-Q insulin treatment is a safe and effective alternative treatment to IV insulin in the management of people with mild or moderate DKA.
With a little more digging, I found 2 more recent papers that suggest considering Sub-Q insulin treatment as an option for mild or moderate DKA.
It is important to note that sub-Q insulin treatment for DKA is NOT recommended for patients with arterial hypotension, severe and complicated DKA, or with HHS.
Treating DKA with Sub-Q insulin Steps
Insulins: Use either rapid acting lispro or aspart insulin.
1st Bolus: Starting dose is 0.1 or 0.2 or 0.3 units/kg of insulin (depending on initial blood glucose and clinical presentation)
Example: Pt weighs 100 kg, give 100kg x 0.1 – 0.2 – 0.3 units/kg of insulin = 10 or 20 or 30 units insulin sub-q bolus respectively.
Next Step – Sub-q insulin every 2 hours | Give 0.1 – 0.2 units of insulin /kg every 2 hours until blood glucose is less than 250.
Example: Pt weighs 100 kg, give 100kg x 0.1 – 0.2 units/kg of insulin = 10 or 20 units insulin sub-q bolus respectively every 2 hours.
Blood glucose less than 250 | Now give 1/2 the sub-q insulin dose every 2 hours. Calculate 0.05 to 0.1 units/kg every 2 hours until glucose at target and ketosis is resolved.
Example: Pt weighs 100 kg, give 100kg x 0.05 – 0.1 units/kg of insulin = 5 or 10 units insulin sub-q bolus respectively every 2 hours.
Using scheduled subcutaneous insulin allows for safe and effective treatment in the emergency room and step-down units without the need for ICU care. Umpierrez et al
Please see reference chart and articles below for more detailed information.
Fluids and Electrolytes
Of course, fluid and electrolyte status needs to be assessed before starting insulin.
If the K+ is less than 3.3, hold insulin and start with IV fluids (NS or LR) first with potassium replacement. Once the K is stable, start the insulin injection every 2 hours (see article and flow chart below).
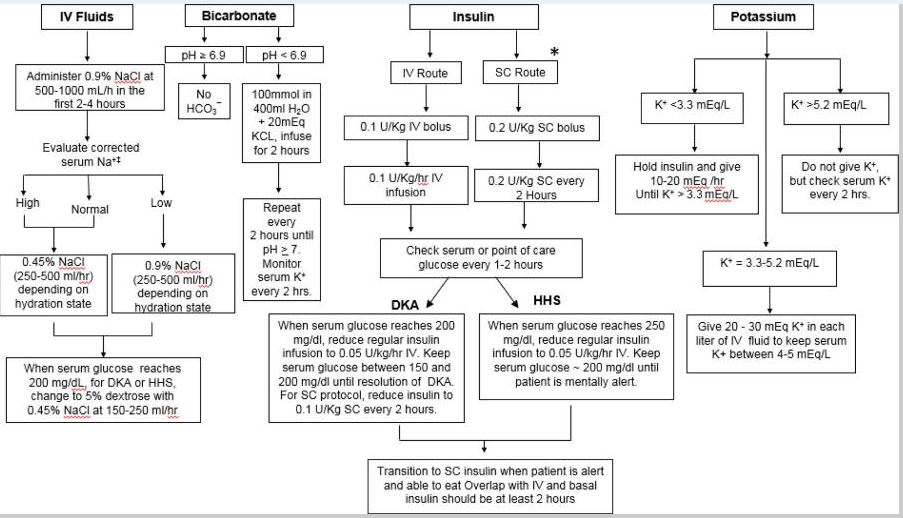
doi: 10.1016/j.mcna.2016.12.011
Management of Hyperglycemic Crises: Diabetic ketoacidosis and hyperglycemic hyperosmolar state
Thank you for reading this article. Please share any feedback or your experiences using sub-q insulin for DKA. We always love to hear from you. You can email us at [email protected]
Reference Articles
Eledrisi MS, Elzouki AN. Management of Diabetic Ketoacidosis in Adults: A Narrative Review. Saudi J Med Med Sci. 2020;8(3):165-173. doi:10.4103/sjmms.sjmms_478_19
Fayfman M, Pasquel FJ, Umpierrez GE. Management of Hyperglycemic Crises: Diabetic Ketoacidosis and Hyperglycemic Hyperosmolar State. Med Clin North Am. 2017;101(3):587-606. doi:10.1016/j.mcna.2016.12.011
Hyperglycemic Crises, DKA & HHS | 1.0 CEs
Join Coach Beverly to learn more about causes and treatment of hyperglycemic crisis. (opens in a new tab)”>Find out more here>>

This course is included in: Level 2 – Standards of Care. Purchase this course individually for $19 or the entire bundle and save 70%.
This 60-minute course discusses common causes of hyperglycemia crises. Topics include hyperglycemia secondary to medications and insulin deprivation. The difference and similarities between Diabetes Ketoacidosis and Hyperosmolar Hyperglycemic Syndrome are also covered. Treatment strategies for all situations are included.
Topics include:
- Common causes of hyperglycemic crises.
- The difference and similarities between DKA and HHS and treatment strategies
- Causes and treatment of hyperglycemic crises.
Sign up for Diabetes Blog Bytes – we post one daily Blog Byte from Monday to Friday. And of course, Tuesday is our Question of the Week. It’s Informative and FREE! Sign up below!
[yikes-mailchimp form=”1″]
Accreditation: Diabetes Education Services is an approved provider by the California Board of Registered Nursing, Provider 12640, and Commission on Dietetic Registration (CDR), Provider DI002. Since these programs are approved by the CDR it satisfies the CE requirements for the CDCES regardless of your profession.*
The use of DES products does not guarantee the successful passage of the CDCES exam. CBDCE does not endorse any preparatory or review materials for the CDCES exam, except for those published by CBDCE.
Insulin Cost Savings Toolkit
Coach Bev’s Diabetes Cheat Sheets
We know that a great resource page full of accurate and helpful cheat sheets can save busy diabetes specialists time and energy.
That’s why we have put together our entire list of cheat sheets so you can access them with ease.
These sheets and cards include information to study for certification exams and to use in your clinical setting. Plus, we have included teaching sheets for people with diabetes.
Our Summer 2020 Boot Camp begins September 16th!

In each webinar, either Coach Beverly, Dr. Isaacs, or Ms. Armstrong, highlight the critical content of each topic area, so you can focus your study time most efficiently. They also launch multiple poll questions to help participants focus on key concepts and assess their knowledge while learning the best test-taking strategies.
2020 Boot Camp Live Stream Webinar Schedule with Coach Beverly
All courses air at 11:30 a.m. (PST)
- Diabetes – Not Just Hyperglycemia | Sept 16
- ADA Standards of Care | Sept 23
- Insulin Therapy – From Basal/Bolus to Pattern Management | Sept 30
- Insulin Intensive – Monitoring, Sick Days, Lower Extremities | Oct 7
- Meds for Type 2 | Oct 14
- Exercise and Preventing Microvascular Complications | Oct 21
- Coping & Behavior Change | Oct 28
- “The Big Finish” Test Taking Boot Camp | Nov 4
Can’t make it live?
No worries! All video presentations and podcasts will be available now on-demand.
Sign up for Diabetes Blog Bytes – we post one daily Blog Byte from Monday to Friday. And of course, Tuesday is our Question of the Week. It’s Informative and FREE! Sign up below!
[yikes-mailchimp form=”1″]Accreditation: Diabetes Education Services is an approved provider by the California Board of Registered Nursing, Provider 12640, and Commission on Dietetic Registration (CDR), Provider DI002. Since these programs are approved by the CDR it satisfies the CE requirements for the CDCES regardless of your profession.*
The use of DES products does not guarantee the successful passage of the CDCES exam. CBDCE does not endorse any preparatory or review materials for the CDCES exam, except for those published by CBDCE.
[yikes-mailchimp form=”1″]CGMs Lead to Cost Savings
For people with type 1 diabetes, access to Continuous Glucose Monitoring (CGM) technology, is considered a standard of care by most experts.
There is plenty of research that demonstrates CGM use is associated with not only improved A1c but significantly decreases time in hypoglycemic range and ketoacidosis rates.

Researchers wondered if this translates into cost savings?
YES.
According to a study presented at the Heart in Diabetes virtual meeting.
After three years of follow-up, the savings were substantial.
- Multiple daily injection plus CGM users saved between $5,777 and $8,549.
- CGM users with continuous subcutaneous insulin infusion saved between $2,732 and $4,753 per person, compared with non-CGM users.
“In this study, we showed that it didn’t make any difference how you deliver insulin,” Grunberger said. “This difference is in how you monitor glucose.”
George Grunberger, MD, FACP, MACE, Chairman Grunberger Diabetes Institute and more
Glucose Crises are Expensive
According to Grunberger, the cost of diabetes ketoacidosis (DKA) in the U.S. is over 5 billion dollars a year.
Having a CGM reduces DKA rates, hospitalization, and leads to cost savings.
A study in the United Kingdom showed that for 900 people using the Freestyle Libre (Abbott), DKA episodes were reduced by 80% within six months of using this device.
A study in Belgium followed 1,913 people with type 1 diabetes using the Freestyle Libre CGM.
Not only did they see a dramatic reduction in hospitalizations from DKA and hypoglycemia, but the researchers also observed a fifty percent drop in work absenteeism.
The data shows CGM’s are associated with cost savings due to less diabetes emergencies and decreased work absenteeism.
Full Story: Healio (free registration)/Endocrine Today (8/31)
Sign up for Diabetes Blog Bytes – we post one daily Blog Byte from Monday to Friday. And of course, Tuesday is our Question of the Week. It’s Informative and FREE! Sign up below!
[yikes-mailchimp form=”1″]Accreditation: Diabetes Education Services is an approved provider by the California Board of Registered Nursing, Provider 12640, and Commission on Dietetic Registration (CDR), Provider DI002. Since these programs are approved by the CDR it satisfies the CE requirements for the CDCES regardless of your profession.*
The use of DES products does not guarantee the successful passage of the CDCES exam. CBDCE does not endorse any preparatory or review materials for the CDCES exam, except for those published by CBDCE.
[yikes-mailchimp form=”1″]Metformin XR Warning due to NDMA impurity
Some brands of long acting Metformin are being recalled since they contain higher than acceptable levels of NDMA (see list below).
The U.S. Food and Drug Administration has recommended recalls of certain metformin products that may contain the impurity N-nitrosodimethylamine (NDMA) above the acceptable intake limit.
Patients taking recalled metformin should continue taking it until a doctor or pharmacist gives them a replacement or a different treatment option. It could be dangerous for patients with type 2 diabetes to stop taking their metformin without first talking to their health care professional.
Remind patients not to stop medication until they check with their provider.
Find more info on the FDA Website here
Recalled Products
- The agency is also asking all manufacturers of extended release versions of metformin to evaluate their risk of excessive NDMA and to test at-risk product before each batch is released onto the U.S. market. If testing shows NDMA above the acceptable intake limit, the manufacturer must inform the agency and should not release the batch to the U.S. market.
- FDA’s testing has shown elevated levels of NDMA in some extended release (ER) metformin formulation but not in the immediate release (IR) formulation or in the active pharmaceutical ingredient.
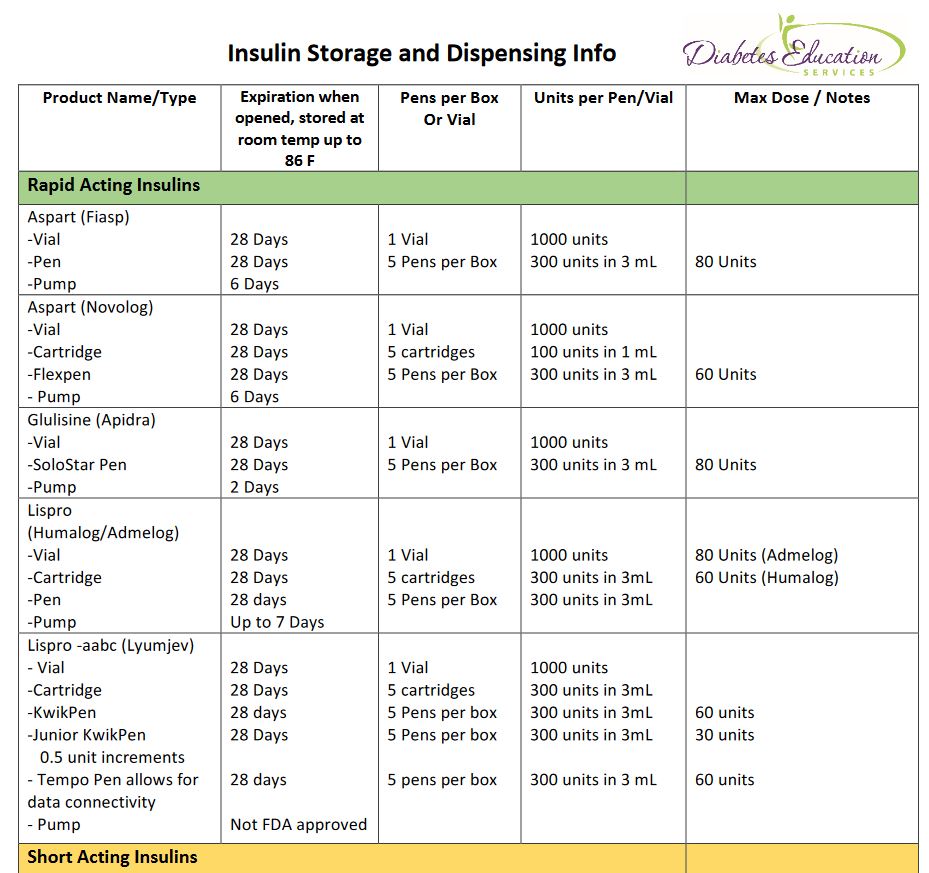
For a complete listing of diabetes medications and insulin, download our DiabetesEd Medication PocketCards
Join Meds Management for Type 2 Webinar with Coach Beverly
Purchase or No CEs | Free
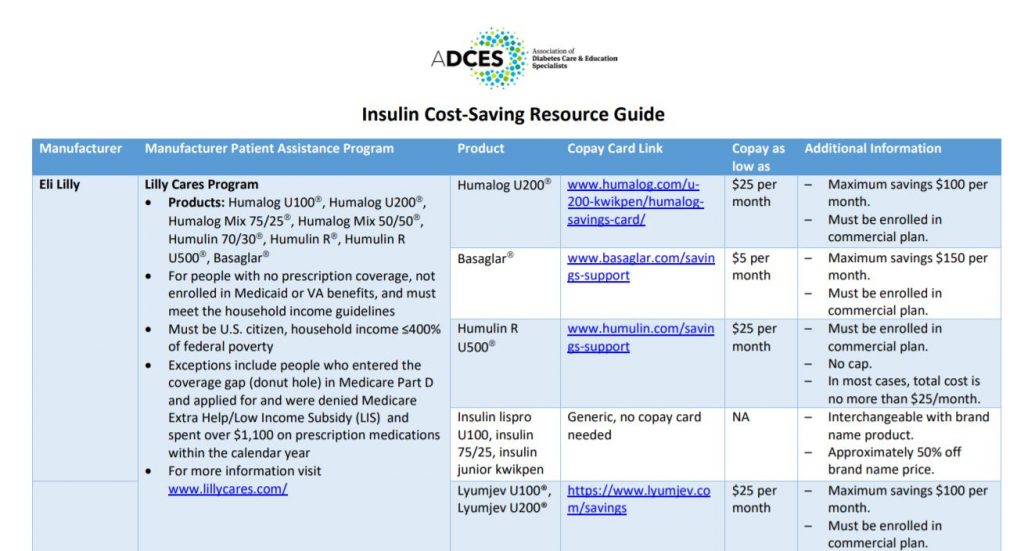
Insulin Cost Savings | Resources for Diabetes Specialists

Written by Diana Isaacs, PharmD, BCPS, BC-ADM, BCACP, CDCES & ADCES 2020 Diabetes Educator of the year
The cost of insulin is a real problem. It can lead to insulin rationing and at its worst, people have died due to a lack of insulin.
A recent survey reported that 26% of respondents living in the US rationed insulin at last once in the last year.
The retail price for a box of insulin pens is about $500. Many people need more than one box of pens per month. Even with health insurance, people struggle to afford this. I remember one of my patients telling me she was only taking half of her prescribed dose of insulin glargine because her daughter was taking the same insulin and they both needed it. This just broke my heart!
Fortunately, the Food and Drug Administration (FDA), as well as drug companies, have heard the outcries from people who require insulin to live. In response, there are some helpful new programs that make insulin more affordable. However, it can be difficult to navigate all of the new information. To help make navigation easier, we have created an ADCES Access & Affordability page with Insulin Cost-Savings Resource Guide.
Here is a list of different strategies to access affordable insulin.
Why is insulin so expensive?
Insulin is considered a Biologic Drug, which makes it more expensive to produce.
Insulin is made from recombinant DNA technology, making it a biologic drug. Biologic drugs depend on unique manufacturing conditions that are proprietary and difficult to exactly replicate. Therefore, when the drug brand name patent expires, other companies can’t make true generics.
Until recently, the pathway for approval was called a follow-on biologic. This is how Basaglar (insulin glargine) and Admelog (insulin lispro) are classified. In March 2020, the FDA announced that regulatory requirements would change allowing for biosimilar products. This may ultimately increase market competitiveness in hopes to further reduce insulin prices. Basaglar and Admelog offer about a 15-20% discount from their reference products of Lantus and Humalog, respectively. Many argue these cost savings is just not enough.
Generic Insulins
Because insulin is a biologic drug, a true generic must come from the same manufacturer. Recently Lilly and Novo Nordisk have created generic insulins.
Lilly offers generics of insulin lispro, insulin lispro mix 75/25, and insulin lispro junior kwik pen.
Novo Nordisk offers generics of their insulin, which they are calling a “follow on Brand” and includes insulin apart and insulin aspart mix 70/30.
Both Lilly and Novo offer approximately a 50% cost savings from the original insulin product and the pharmacist can make an automatic substitution if you ask.
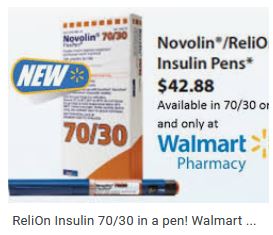
Walmart and some other pharmacies also offer ReliOn insulins. These include Novolin R, Novolin N, and Novolin 70/30. These are slower acting insulins that may predispose people to more hypoglycemia, but they are only $25/vial or $44/5 pack of pens and do not require a prescription in most states. Access to these insulins can be truly life-saving in some circumstances. Every person with diabetes needs to be aware that they can purchase these insulins without a prescription if they are ever out of insulin.

New Programs that Cap Insulin Pricing
Lilly announced a program capping insulin co-pays at $35/month for those paying with cash or commercial insurance. This will dramatically lower monthly costs for many people with diabetes.
Sanofi has a Valyou program that allows up to 10 vials or 10 boxes of insulin pens for a maximum of $99/month. Of note, Sanofi’s program will only work for those without insurance.
Novo Nordisk recently started the My $99 insulin program. What’s unique about this program is that it will work for those with commercial insurance or government plans like Medicare. Most other programs exclude people with Medicare. This program covers up to 3 vials or 2 packs of pens.
Co-Pay Cards
Most insulins offer a co-pay card which can bring down the price of insulin most commonly to $0 to $25/month depending on the manufacturer and type of insulin. For any person with a commercial insurance plan, it’s good to check if a co-pay card is available for the insulin before picking it up from the pharmacy.
The things to be aware of about these cards are that they have maximum savings and sometimes that is much less than the total cost of the insulin. Also, they only work for people with commercial insurance meaning they won’t for people without health insurance or that have a government insurance plan like Medicare. They also do not always work if the drug is not covered on the insurance plan. In that case, it would be preferable to switch to an insurance-covered on the insurance plan.
Patient Assistance Plans
These are programs offered through pharmaceutical companies for people without health insurance or that have Medicare but still struggle to pay for medications. There are various income requirements to be eligible, but depending on the program it can be 250-400% above the Federal poverty line. Many people are surprised to find that they are eligible, so this is a good option to look into which can make the insulin completely free. There is typically a packet of information that needs to be completed and then if eligible, the insulin is shipped to the prescriber’s office for the patient to pick up.
In summary, It can be challenging to keep all of this information straight. This is why I worked with a team of amazing diabetes care and education specialists at ADCES to create the ADCES Access & Affordability page with Insulin Cost-Savings Resource Guide. We update this resource frequently and it includes links to patient assistance programs, co-pay cards, and other cost savings programs. We hope you find it useful and that your patients with diabetes will benefit.
Special thanks to our guest contributor for this article: Diana Isaacs, PharmD, BCPS, BC-ADM, BCACP, CDCES & ADCES 2020 Diabetes Educator of the year
References:
Conner F, Pfiester E, Elliott J, Slama-Chaudhry A. Unaffordable insulin: patients pay the price. The Lancet Diabetes & Endocrinology 7 (10), 748,2019.
For a summary of all this information, see the ADCES Insulin Cost Savings Resources Page.
Sign up for Diabetes Blog Bytes – we post one daily Blog Byte from Monday to Friday. And of course, Tuesday is our Question of the Week. It’s Informative and FREE! Sign up below!
[yikes-mailchimp form=”1″]Accreditation: Diabetes Education Services is an approved provider by the California Board of Registered Nursing, Provider 12640, and Commission on Dietetic Registration (CDR), Provider DI002. Since these programs are approved by the CDR it satisfies the CE requirements for the CDCES regardless of your profession.*
The use of DES products does not guarantee the successful passage of the CDCES exam. CBDCE does not endorse any preparatory or review materials for the CDCES exam, except for those published by CBDCE.
New Triple Combo Pill for Type 2 Diabetes

The FDA made history last month by approving the first-ever triple combination pill for type 2 diabetes. This medication can help simplify the medication regimen for people living with type 2 diabetes.
As the director of the diabetes research unit at the University of Texas Health Science Center at San Antonio, Ralph A. DeFronzo, MD, said, “Type 2 diabetes is a complex disease that often requires the use of multiple antidiabetic medications to improve glycemic control. Having three different diabetes medications in a single tablet is an important advance in diabetes treatment.”
Known as Trijardy XR, this medication combines the SGLT2 inhibitor empagliflozin, the DPP-IV inhibitor linagliptin, and metformin extended-release. Both empagliflozin and linagliptin lower blood glucose and empagliflozin has the added benefit of reducing the risk of cardiovascular death and chronic heart failure for those living with cardiovascular disease or chronic heart failure.
Additionally, a trial that was presented at the American Diabetes Association (ADA) Scientific Sessions by Healio found that linagliptin will not increase the risk for a cardiovascular event, nor will it contribute to the progression of renal disease among people with type 2 diabetes. This trial, known as the CARMELINA trial, was conducted over six years, across a group of 6,000 people. The trial demonstrated that no “between-group differences for the incidence of nonfatal myocardial infarction, nonfatal stroke and CV death during a median of 6 years.”
- Trijardy XR will be available in four dosages:
- 5 mg empagliflozin/2.5 mg linagliptin/1,000 mg metformin ER
- 10 mg empagliflozin/5 mg linagliptin/1,000 mg metformin ER
- 12.5 mg empagliflozin/2.5 mg linagliptin/1,000 mg metformin ER
- 25 mg empagliflozin/5 mg linagliptin/1,000 mg metformin ER.
There is no information on pricing as of yet. Read more about Trijardy here.
Sign up for Diabetes Blog Bytes – we post one daily Blog Byte from Monday to Friday. And of course, Tuesday is our Question of the Week. It’s Informative and FREE! Sign up below!
[yikes-mailchimp form=”1″]