Winter Solstice – The Great Conjunction

Today, is Winter Solstice, when we experience the shortest day and longest night of the year. From here we will slowly gain more light each day, marking this as an astronomical shift from darkness to light.
For many cultures, winter solstice marks a day of rebirth, saying goodbye to the past year and a universal deep breath for the future.
Susan Cooper penned a beautiful poem about winter solstice that we are thrilled to share with you below. Given this incredibly difficult year, it seems especially poignant and I hope you enjoy the read.
Great conjunction this close last happened 400 years ago.
As a special bonus this year, Jupiter and Saturn will align in the night sky today, December 21st, in an event astronomers call the “great conjunction.”
The last time Jupiter and Saturn came this close was 1623, but that conjunction was too near the sun to be seen by Earthlings. 1226 is actually the most recent time such close conjunction of Jupiter and Saturn was visible to humans.
You can watch it online with webcasts from The Virtual Telescope Project, Slooh at NASA Telescope here.
The Shortest Day by Susan Cooper
And so the Shortest Day came and the year died
And everywhere down the centuries of the snow-white world
Came people singing, dancing
To drive the dark away
They lighted candles in the winter trees
They hung their homes with evergreen
They burned beseeching fires all night long
To keep the year alive
And when the new year’s sunshine blazed awake
They shouted, reveling
Through all the frosty ages you can hear them
Echoing behind us—listen!
All the long echoes, sing the same delight
This Shortest Day
As promise wakens in the sleeping land:
They carol, feast, give thanks
And dearly love their friends
And hope for peace.
And now so do we, here, now,
This year and every year.
Welcome, Yule!
This poem is available as a children’s hardcover with beautiful watercolor illustrations by Carson Ellis.
Happy World Diabetes Day
Today, November 14, is Dr. Banting’s Birthday
World Diabetes Day is celebrated in honor of Dr. Fredrick Banting, whose leadership, tenacity and belief led to the discovery of insulin.
The discovery of insulin has saved the lives of countless millions of people over the past hundred years and will continue to save millions of lives in the near future and beyond.
During a hot summer in 1921, Dr.Banting secured space to test out his theory at the University of Toronto. Along with his colleague, Charles Best, and a bare-bones lab, they conducted dozens of experiments on dogs, which ultimately led to the discovery of insulin.


Dr. Banting and Charles Best began their experiments ligating the pancreases of dogs, thinking this would prevent destruction by the digestive pancreatic juices, and then isolating the extract from the islet cells. They then processed the extract from the islet cells and injected this extract they called “insulin” into diabetic dogs. According to an audio interview with Dr. Best, by July 1921, they had 75 positive examples of insulin lowering blood glucose levels in dogs.

In February 1922, doctor Frederick Banting and biochemist John Macleod published their paper on the successful use of an alcohol-based pancreatic extract for normalizing blood glucose levels in a human patient.
Here are some photos of the first insulin bottles produced by the University of Toronto and Eli Lilly.
Soon, word of their discovery got out and the race was on to produce enough insulin to treat the flood of type 1 patients arriving in Toronto to receive this miracle injection.
But, as with any amazing discovery, there is always more to the story.
One of the biggest barriers to Banting was the simple fact that he was not involved in the field of diabetes research. The idea leading to the discovery of insulin came to him after preparing a lecture on the pancreas and diabetes, a subject he knew little about. He wasn’t a trained researcher and thus securing support for the project was initially difficult.
First Children to Receive Insulin
The first patient to receive insulin was a ‘welfare’ case at Toronto General Hospital – no clinical trial structure to say the least. People from Canada/US flooded into Toronto to receive treatment. Banting struggled with the lack of accessibility of insulin – volume needed issues of purification.
The earliest patients were “selected”, some youths from Canada/US, some soldiers with diabetes (probably because of Banting’s service in the First World War), and then later some select private patients. During this time they were working hard to increase the volume and continue to improve the purification process. Insulin was available for testing in the US, namely through Dr. Elliot Joslin in the late summer of 1922.
Takes a Team

While Best played a critical and important role, credit must also go to Professor Macleod, from the University of Toronto, who provided the lab space, showed Dr. Banting how to operate on dogs, provided his student Best and suggested they switch from saline to alcohol to purify the ‘extract’. Dr. Macleod also secured the support of JB Collip, the 4th man on the team, and the first person to purify insulin for human use. Best is also known for pushing Banting to return to the research during a particularly dark period of failure.
Dr. Banting – Fun and Interesting Facts
- Sold insulin patent for $1
- Was wounded during the First World War and received the Military Cross
- Youngest Nobel Laureate in Medicine
- First Canadian on the cover of Time Magazine
- Among the last Canadians to receive a knighthood and have the title, Sir Frederick Banting
- One of only two “non-Americans” to have a Second World War Liberty Ship named after him (USS Frederick Banting)
- Has as a crater on the Moon named after him (between Apollo 15 & 17 landing sites).
Want to Learn More About Dr. Banting?
Visit Banting House FaceBook Page
Sign up for Diabetes Blog Bytes – we post one daily Blog Byte from Monday to Friday. And of course, Tuesday is our Question of the Week. It’s Informative and FREE! Sign up below!
[yikes-mailchimp form=”1″]Keeping it Person-Centered | QoW Rationale

Our October 27th Question of the week quizzed test takers on person-centered language. We are happy to report that 88% of respondents chose the correct answer. We thought that this was an important topic to discuss further, so we can pass on correct info to people living with diabetes.
Before we start though, if you don’t want any spoilers and haven’t tried the question yet, you can answer below: Answer Question
Question: Language use while interviewing someone with diabetes can have a profound impact on the meaningfulness of the interaction.
Which of the following comments uses a person-centered approach and exemplifies the use of updated diabetes language?
Answer Choices:
- We don’t recommend avoiding breakfast
- Tell me more about skipping your afternoon insulin
- I notice you haven’t tested your blood sugars daily
- Exercise is important because it helps control your glucose levels
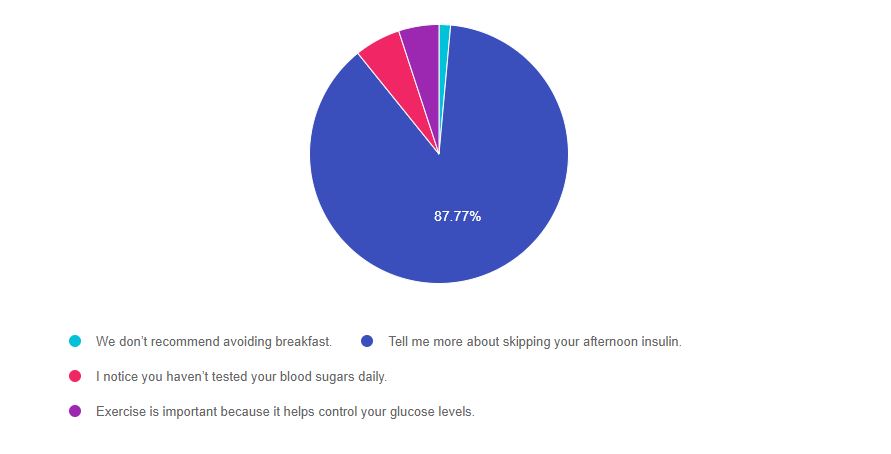
As shown above, the most common choice was option 2, the second most common answer was option 3, then option 3, and finally option 1.
Getting to the Best Answer
If you are thinking about taking the certification exam, this practice test question will set you up for success. Test writers anticipate possible answers based on the details in the question. They will wave those “juicy answers” right under your nose. Your job is to weed through the particulars, pluck out the most important elements and choose the BEST answer.
Most of you chose the correct answer, which is really terrific. I have noticed an increased awareness of the new language paradigm when coaching people with diabetes. I am confident this person-centered approach will strengthen the meaningfulness of our interactions and improve quality of life for people living with diabetes.
Answer 1 is incorrect. 1.44% chose this answer. “We don’t recommend avoiding breakfast”
The fact that this sentence starts with the word “we”, gives us the first clue it is not person-centered. This approach and language align more with the out-dated compliance model, which simply gives people direction without seeking input or collaboration.
Answer 2 is correct. 87.77% of you chose this answer. “Tell me more about skipping your afternoon insulin”
This is an example of the preferred curiosity-based approach that is free of judgment. It simply acknowledges the fact that the person is skipping their afternoon insulin and requests more information about the circumstances. It represents a person-centered and collaborative approach.
Answer 3 is incorrect. About 5.76% of respondents chose this. “I notice you haven’t tested your blood sugars daily”
This approach is not strength-based, instead, it has a hint of judgment and criticism. The person receiving this message might feel shame or embarrassment. A strength-based approach would be, “You have been checking your blood sugars 4 times a week.” Then we could have a conversation to determine if that is often enough or if more checks would be beneficial. This strength-based approach engages the participant and acknowledges what they ARE doing.
Finally, Answer 4 is incorrect. 5.04% chose this answer. “Exercise is important because it helps control your glucose levels.”
Instead of telling people TO exercise, a better approach would be starting with a question like, “Did you know that every minute of exercise lowers your blood sugar about one point?”. Or, “Is there a type of activity you have done in the past that you enjoyed?” In addition, we avoid using the word “control” and replacing it with the word “manage”. We could also say, “The great thing about exercise is that helps manage blood sugars for 24-28 hours.”
Want more info on Language and Diabetes?
Check our our FREE Webinar and Resources Page – Lifting People UP with our Words.
We hope you appreciate this week’s rationale! Thank you so much for taking the time to answer our Question of the Week and participate in this fun learning activity!
Test Taking Toolkit (220+ practice questions) | Online | $ 49.00
Whether you are preparing for the updated CDCES or BC-ADM exam, this test-taking toolkit is designed to prepare you for success. This toolkit includes two courses with over 220 practice questions to help you prepare and simulate the exam.
Our exams incorporate changes to the CDCES content outline, including a more intensive focus on technology, social issues, and emergency readiness. Plus, we have added a FREE bonus course, Language and Diabetes – What we say matters (0.5 CEs). Coach Beverly added this course because she believes it contains critical content for the exam and for our clinical practice!
- ADA Standards Test Taking Tips
- Preparing for CDCES Practice Exam
Sign up for Diabetes Blog Bytes – we post one daily Blog Byte from Monday to Friday. And of course, Tuesday is our Question of the Week. It’s Informative and FREE! Sign up below!
[yikes-mailchimp form=”1″]Accreditation: Diabetes Education Services is an approved provider by the California Board of Registered Nursing, Provider 12640, and Commission on Dietetic Registration (CDR), Provider DI002. Since these programs are approved by the CDR it satisfies the CE requirements for the CDCES regardless of your profession.*
The use of DES products does not guarantee the successful passage of the CDCES exam. CBDCE does not endorse any preparatory or review materials for the CDCES exam, except for those published by CBDCE.
Self-Kindness Improves Mental and Physical Health

By taking time for self-compassion, you can decrease your body’s threat response, lower heart rate, and even boost your immune system.
This is especially important to keep in mind and share with our clients during the pandemic since many people are struggling with feelings of isolation, fear, and sorrow.
According to a study conducted by the Universities of Exeter and Oxford, thinking compassionate thoughts about yourself and others has physical benefits.
Researchers believe that meeting negative thoughts with self-compassionate thoughts can be highly beneficial to not only mental health but physical health as well.
In the past, studies have shown a link between self-care and higher levels of overall health and well-being, but scientists didn’t understand why.
“Our study is helping us understand the mechanism of how being kind to yourself when things go wrong could be beneficial in psychological treatments. By switching off our threat response, we boost our immune systems and give ourselves the best chance of healing.”
Mindfully decreasing our threat response, increases relaxation, which is a key factor in allowing the body to regenerate and heal. Our threat response, includes “increased heart rate and sweating, the release of the stress hormone cortisol and over-activity of the amygdala, an integral part of the brain’s emotional network. And a persistent threat response can impair the immune system.”
The study asked participants to listen to either compassionate audio recordings or critical and competitive recordings. Scientists would then record their vitals and ask them a series of questions.
Those encouraged to practice self-compassion had a lower heart rate and a general feeling of “safety.” While those who listen to negative critical audio statements had an increase in heart rate and higher sweat response.
We invite you to watch our FREE Mindful Diabetes Encounter Webinar designed for diabetes professionals.
To learn more: Self-Compassion Exercises Show Physical, Psychological Benefits – Psych Central
Sign up for Diabetes Blog Bytes – we post one daily Blog Byte from Monday to Friday. And of course, Tuesday is our Question of the Week. It’s Informative and FREE! Sign up below!
[yikes-mailchimp form=”1″]Accreditation: Diabetes Education Services is an approved provider by the California Board of Registered Nursing, Provider 12640, and Commission on Dietetic Registration (CDR), Provider DI002. Since these programs are approved by the CDR it satisfies the CE requirements for the CDCES regardless of your profession.*
The use of DES products does not guarantee the successful passage of the CDCES exam. CBDCE does not endorse any preparatory or review materials for the CDCES exam, except for those published by CBDCE.
Blessing the Boats | Mindful Monday
With everything going on in the world, I thought today we would move gently into Monday with a poem by Lucille Clifton.

Blessing the Boats
may the tide
that is entering even now
the lip of our understanding
carry you out
beyond the face of fear
may you kiss
the wind then turn from it
certain that it will love you back
may you
open your eyes to water
water waving forever
and may you in your innocence
sail through this to that
~ Lucille Clifton (at St. Mary’s)
Mindfulness and Compassion | A Special Webinar for Diabetes Specialists
View OnDemand FREE Webinar Now

Being a diabetes educator can be challenging. This one-hour presentation by Heather Nielsen, MA, LPC, CHWC will provide diabetes educators with helpful hands-on strategies to incorporate mindfulness and self-compassion into our daily lives and professional practice. As a counselor and a certified wellness coach, Heather has an abundance of wellness wisdom to share with educators who provide lifesaving diabetes education and support to people living with diabetes.
Objectives:
- Understand why mindfulness and compassion skills can positively affect both our personal and professional lives-and participant outcomes.
- Experience several types of mindfulness and compassion practices.
- Discuss and plan how you can take these tools into your work and personal lives.
- Gain new resources to use following the workshop.
Sign up for Diabetes Blog Bytes – we post one daily Blog Byte from Monday to Friday. And of course, Tuesday is our Question of the Week. It’s Informative and FREE! Sign up below!
[yikes-mailchimp form=”1″]
Accreditation: Diabetes Education Services is an approved provider by the California Board of Registered Nursing, Provider 12640, and Commission on Dietetic Registration (CDR), Provider DI002. Since these programs are approved by the CDR it satisfies the CE requirements for the CDCES regardless of your profession.*
The use of DES products does not guarantee the successful passage of the CDCES exam. CBDCE does not endorse any preparatory or review materials for the CDCES exam, except for those published by CBDCE.
“Awe” Walks Improve Well-Being
Looking for awe helps us move from dis-ease to a sense of well-being.

We all know the physical health benefits of walking, but what if we add the intention to experience “awe” during our jaunts?
Researchers divided older subjects, (60 years plus) into 2 different groups. Both groups walked for 15 minutes and logged how they were feeling and thinking about during their walks.
Intentionally Look for Awe
However, the experimental group was asked to walk for 15 minutes in a natural setting and to intentionally look for moments of “awe” during their outings.
In the study, people who took a fresh look at the objects, moments and vistas that surrounded them during brief, weekly walks felt more upbeat and hopeful in general than walkers who did not. The findings are subjective but indicate that awe walks could be a simple way to combat malaise and worry.
Gretchen Reynolds
Examples of “awe” discoveries could include simple things like noticing a frog peeking at you from a nearby pond. Or observing the variety of hues during sunset. Or looking up at the sky through a rainbow of trees.

Awe Moments Improve Well- Being
As expected, the study participants who simply looked for these moments of awe, had an associated improvement in their sense of well being. Overall, the awe walkers felt happier, less upset, and more socially connected than the men and women in the control group.
The Take-Home Message is “Awe” some
As diabetes specialists, we encourage people to walk to help lower glucose, improve balance, and gain muscle mass. By adding this element of awe, we just might be helping people gain enhanced quality of life too.
Life is hard right now and many people are feeling isolated and sorrowful. By taking a fresh look at these little wonders all around us, it reminds us that we are a part of something bigger than ourselves. And in that knowing, that each of us is important, meaningful, and loved.
Happy Monday. Love, Coach Beverly
Sign up for Diabetes Blog Bytes – we post one daily Blog Byte from Monday to Friday. And of course, Tuesday is our Question of the Week. It’s Informative and FREE! Sign up below!
[yikes-mailchimp form=”1″]Accreditation: Diabetes Education Services is an approved provider by the California Board of Registered Nursing, Provider 12640, and Commission on Dietetic Registration (CDR), Provider DI002. Since these programs are approved by the CDR it satisfies the CE requirements for the CDCES regardless of your profession.*
The use of DES products does not guarantee the successful passage of the CDCES exam. CBDCE does not endorse any preparatory or review materials for the CDCES exam, except for those published by CBDCE.
Impacts of Healthcare Inequities & How We Can Change Them
As Diabetes Education Specialists and advocates, we see first-hand how healthcare inequalities impact the health of under-resourced communities.
Just as diabetes is systemic, affecting the entire body, so are the disparities in our public and private healthcare systems.
This is not only a result of public policies, healthcare education, medical racism, and medical classism, but also access to nutritious whole foods, stable housing, insurance coverage, and even enough time in the day to focus on one’s health.
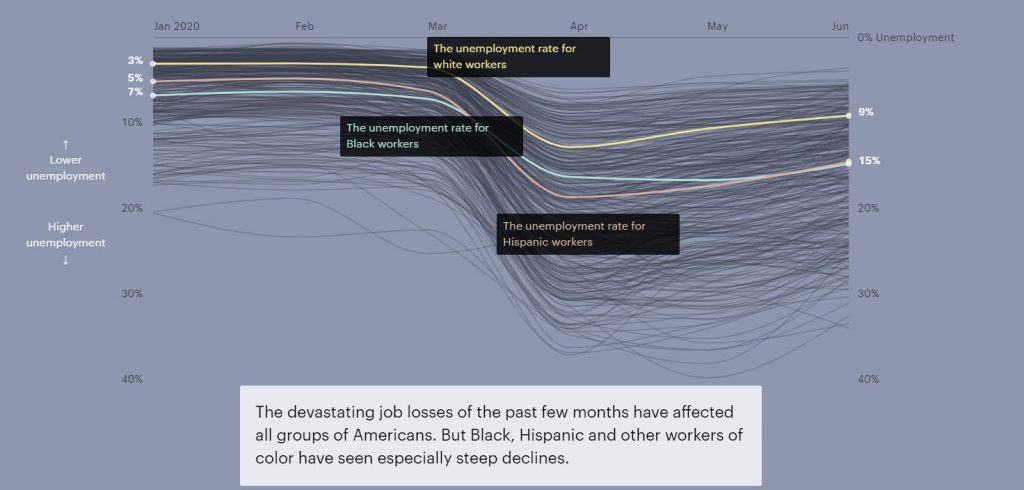
Under the COVID-19 pandemic, these disparities have become even more apparent.
“Black and Latino patients are two to three times as likely as white patients to be diagnosed with COVID-19, and more than four times as likely to be hospitalized for it. Black patients are more than twice as likely to die from the virus. They also die from it at younger ages“ wrote Ezekiel J. Emanuel, Oncologist, bioethicist, and vice provost of the University of Pennsylvania and Risa Lavizzo-Mourey, Professor at the University of Pennsylvania for The Atlantic.
Acknowledging these perforations of care is an important first step towards a more inclusive healthcare system. This reparative practice can result in more positive outcomes and improve the quality of life for many.
Insurance Coverage & Reimbursement Rates
Equal access to healthcare coverage is key.
The economic impacts of the pandemic have widened the gap in insurance coverage. Around 12 million people living in the U.S. lost employer insurance due to the pandemic, with higher unemployment rates for Black and Latino workers (see above graph).
Since the implementation of the Affordable Care Act (ACA) the number of uninsured individuals and families was reduced. However, 15 states opted out of the widening of programs like Medi-Caid under ACA.
For those insured under Medi-Caid, there is still the hurdle of finding a provider that accepts their insurance. This is because many healthcare professionals do not accept Medi-Caid due to low reimbursement rates.
Initially, the ACA increased rates for providers who accepted Medicare and Medi-caid. But they have decreased over time and with that decrease, the number of doctors accepting or even scheduling individuals with Medi-Caid decreased, as well.
“A 2014–15 survey showed that only 68 percent of family-practice physicians accepted new Medicaid patients, while 91 percent accepted those with private insurance,” Ezekiel J. Emanuel and Risa Lavizzo-Mourey.
In addition to raising overall fees for service, implementing a system in which healthcare providers are reimbursed based on health outcomes can be a way to hold us accountable to provide a high level of care, despite factors such as race, gender, sexuality, or class.
Unlearning Medical Biases & Increasing Representation
Medical discrimination is pervasive.
A study conducted earlier in the pandemic found “that doctors were less likely to refer symptomatic Black patients for testing than they were to refer white ones.”
It has also been studied that white medical students and residents rate pain lower for Black people who are experiencing similar symptoms to white people. This bias impacts their care recommendations and the study found lower accuracy of treatment plans for the Black person’s case example.
Educating ourselves on the history of medical racism and classism while engaging in implicit bias training can help us unlearn these inaccurate assumptions.
Representation matters for Healthcare Providers.
Lack of representation often stems from a multitude of factors, such as discriminatory admissions or hiring practices.
An experiment conducted in Oakland found that involving Black doctors in treatment plans reduced the cardiovascular mortality gap by 19% for Black and white men.
Another example of why representation matters are reflected in how commonly medical texts only show white skin tones. Because of this, Malone Mukwende, a 20-year-old medical student is working on a book to show what symptoms look like on darker skin.
Systemic changes begin with each of us.
Educating ourselves on discriminatory medical practices both for healthcare professionals and the people living with diabetes with whom we work with is a great first step to moving towards a more inclusive medical system.
Written by Bryanna, our Director of Operations & Customer Happiness
Read more from The Atlantic article by clicking here. For more information on racial disparities in the treatment of pain click here. For Malone Mukwende’s story click here.
Sign up for Diabetes Blog Bytes – we post one daily Blog Byte from Monday to Friday. And of course, Tuesday is our Question of the Week. It’s Informative and FREE! Sign up below!
[yikes-mailchimp form=”1″]
Accreditation: Diabetes Education Services is an approved provider by the California Board of Registered Nursing, Provider 12640, and Commission on Dietetic Registration (CDR), Provider DI002. Since these programs are approved by the CDR it satisfies the CE requirements for the CDCES regardless of your profession.*
The use of DES products does not guarantee the successful passage of the CDCES exam. CBDCE does not endorse any preparatory or review materials for the CDCES exam, except for those published by CBDCE.
Lainey Koski – Remembering my Friend with a Heart full of Gratitude

It was a beautiful warm evening when I interviewed Lainey Koski in the spring of 2012. Fifteen minutes into our conversation, I was tearing up with joy, because I knew she was exactly the person I didn’t know I needed.
Lainey had just moved to Chico a few weeks earlier to be closer to her grandchildren and answered my ad for an Administrative Assistant.
From our brief interview, a few critical things stood out. She had built a computer from scratch. She was calm and kindhearted, but she had a certain fierceness and determination about her too. She had a wealth of technology and administrative experience. In short, she was the perfect person to become the first full-time employee of my small, but growing, business.
Lainey elevated our customer service by making sure our website platforms were user-friendly and easy to navigate. In addition, she had a certain technological magic that assured our platforms, and Online University was working right on the back-end. Her genuine concern, skills, knowledge, and attention to detail helped move our company to the next level.
Lainey loved calling customers to speak to them directly.
Even when people emailed with questions about the online university or our website, she would pick up the phone and make sure they had a complete understanding and a fantastic experience.
When Lainey first started, I asked her to believe that together, we were going to grow this little company called Diabetes Education Services.

Lainey was such a great sport. For the first year of working together, we were squeezed into a 10×10 bedroom with 2 desks, our products, a packing station, and my treadmill desk. In addition, my boys, who were 7 and 10 at the time, were frequent visitors. And then there were the two dogs and two cats, who contributed to the overall experience of working in a home-based- office.
Through all the commotion and chaos, Lainey was gracious and understanding. She provided helpful insights on parenting and had a lot of wisdom to share on canning, gardening, and jam making. She shared stories about her adventurous parents, who, with all the kids in tow, traveled extensively plus created a family band.
But it was when she spoke of her grandchildren, that her whole face and being beamed with joy. She would share funny and heartwarming stories about sleepovers with Grandma and their special outings together. Over time, I was fortunate enough to become friends with her daughter, son-in-law, grandchildren, sisters, and husband. My life is richer and better because of knowing Lainey and by extension, her wonderful family.
We worked hard together and had fun too!
In January 2012, Lainey and I conjured up a plan to do a virtual walk across the country to the Banting Museum (where insulin was discovered) in Ontario, Canada. We wanted to make it in time to celebrate World Diabetes Day on November 14th. We both got pedometers and started tracking our daily steps. The Banting Museum was 2,642 miles away. We set a goal of each of us walking at least 50 miles a week, for a combined total of 400 miles a month. We plotted our journey on maps, made virtual stops at all kinds of fun places, and shared our walking path on our Facebook posts and in our monthly newsletter.
We made it to Canada in time to virtually celebrate with the Banting Folk and we continued our U.S virtual tour back home. To this day, I am still walking at least 50 miles a week to continue this tradition that Lainey and I started over 8 years ago.
Finally, in early 2013, we broke ground on our new office. Lainey and I had so much fun picking out paint colors, countertops, and designing our product storage area and packing station.

Lainey is pictured here donning a hard hat in a photoshoot that I had to coax her into doing. She was shy and humble, but with a little encouragement, she was game for almost anything.
To this day, when I look around the beautiful office design and layout, I am reminded of all of Lainey’s ideas and contributions as we created our dream working space.
Early in 2015, Lainey announced that she and her husband Willie would be moving to a homestead near her parents, where she could plant a garden, raise goats, and reconnect with the land.
I didn’t want to see her go, but I was so appreciative of how much she had improved my business and set me up for ongoing success. And, of course, I was joyful that she was moving to live her dream. We agreed that she would continue to provide tech consulting services and help keep our Medication PocketCards up-to-date and posted on our website and CDCES Coach app. Just a few months ago, Lainey helped to design and publish our first Glucagon Emergency Medication PocketCard.
Sadly, Lainey unexpectedly passed away on September 12, 2020. She was young at heart, vibrant, and living her life just as she wanted, on her ranch near her family and connected to the earth, all the way through.
This post is my opportunity to share my profound sorrow and grief of losing such a wonderful human and dear friend way too soon. Many of you reading this might have met or talked to Lainey along the way, and I know that like me, you were blessed for having known her.
But even more important, this is my note of joy and celebration for having the great honor of working with, dreaming with, and loving Lainey Koski as a friend, colleague, role model, and teacher.
Thank you Lainey and know that your light shines on in all the lives you have touched, including mine!









