March 2023 eNews | Nutrition Month & Strategies to Address Food Insecurity
Happy National Nutrition Month

Join us in celebration of National Nutrition Month with the theme, “Fuel for the Future”.
In this newsletter, we explore food sustainability while providing multiple strategies to address food insecurity. About 20% of people living with diabetes don’t have adequate access to predictable and healthy food. As diabetes care and education specialists, we can take a leadership role in our healthcare communities and on an individual level to make sure people know how to access food and make their dollars stretch when purchasing groceries.
Our first article dives into healthy eating while keeping the environment in mind. We include lots of additional resources to explore and share with your community.
Bryanna, our Director of Operations, details how she helped to create a community refrigerator that offers fresh fruit, veggies, and dairy products for people living with food insecurity. The end result is heartwarming and nourishing.
Coach Beverly provides ideas on maximizing a person’s purchasing power by choosing lower-cost yet super-healthy foods. In addition, this article contains lots of resources on plant-based foods and recipes that are easy to prepare.
We also celebrate Registered Dietitian Nutritionists with a spotlight on our expert Virtual Conference speaker, Ashley LaBrier, MS, RD, CDCES. Did you know that people with diabetes who meet with an RD/RDN have a 0.3 to 2% drop in A1C levels? Dietitians are evidence-based, caring advocates and some of my favorite people.
We hope you enjoy our nutrition-inspired Questions and Rationales of the Week for the entire month of March!
Wishing you a nutritious month,
Coach Beverly and Bryanna
Featured Articles
- National Nutrition Month
- Start a Community Fridge
- Strategies to Address Food Insecurity
- Celebrating Dietitians
- Lilly Insulin Cap of $35
- Question of the Week
- Rationale of the Week
Upcoming Webinars
- Critical Assessment Webinar – March 28th
- Prep CDCES Prep FREE Webinar- March 30th
- Virtual DiabetesEd Training Conference – April 26th
- Upcoming Events – See complete calendar listing
FREE Resource Catalog
- Diabetes Cheat Sheets
- Diabetes Blog Bytes
- Medication PocketCards
- Start Your Certification Journey
- CDCES Coach App
- Free Webinars hosted by Coach Beverly
- Question of the Week

See Full Free Resource Catalog
Sign up for Diabetes Blog Bytes – we post one daily Blog Byte from Monday to Friday. And of course, Tuesday is our Question of the Week. It’s Informative and FREE! Sign up below!
The use of DES products does not guarantee the successful passage of the CDCES exam. CBDCE does not endorse any preparatory or review materials for the CDCES exam, except for those published by CBDCE.
National Nutrition Month – Tasty Ways to Keep it Sustainable
The Academy of Dietetics and Nutrition is kicking off National Nutrition Month with a new slogan, “Fuel for the Future”.
They are shining a light on considering food consumption through a lens of sustainability. What are some tasty ways to nourish ourselves during every phase of life and protect the environment?
Registered Dietitian Nutritionists are experts in addressing this question. But how can all diabetes care and education specialist help support healthy habits that are sustainable and celebrate the individual’s unique needs?
Strategies to eat with the environment in mind
Plant-Based Meals and Snacks
A great way to get started is to help people learn how to enjoy more plant-based meals and snacks and decrease meat intake. Both the American Diabetes Association and the American Academy of Endocrinologists highly recommend plant-based nutrition for people with diabetes. Not only are plant-based foods packed full of nutrients, protein, and fiber, they generally confer fewer calories and decrease inflammation. Another added bonus is that they have less impact on planetary health and are more sustainable.
Plant-based eating resources including recipes below. Feel free to copy and share!
- Plant-Based Eating Newsletter and Recipes »
- Plant-Based Cooking – Recipes »
- Plant-based diet may benefit patients with diabetes – Smart Brief
- Vegetarian Starter Kit » an easy-to-read and colorful handout for patients interested in learning more about a vegetarian diet. Published by the Physicians Committee for Responsible Medicine.
Sustainable Eating and Decreasing Food Waste
About one-third of all food is tossed into the trash, filling up landfills and increasing methane gas release. Some strategies to decrease waste include finding creative ways to use leftovers rather than tossing them and composting uneaten foods. Encouraging people to buy foods in season and shop locally when possible can make a big impact on the environment while reducing food costs. Another idea is to start a container or backyard garden to grow food at home.
Resources on decreasing food waste and increasing sustainable eating:
- Sustainable Eating article by the Academy of Nutrition and Dietetics
- Food Dates Lead to Waste- Taste Before Tossing
- 5 tips for Sustainable Eating article by Harvard School of Public Health
- Sustainable Eating Resource Hub by Food Print
- Produce from Purchase to Plate – Steps to Reduce Food Waste article by the Academy of Nutrition and Dietetics
- Local Farmer’s Market Finder by Local Harvest – find Community Supported Agriculture farmers in your area.
To stretch dollars, use a grocery list and shop sales when purchasing food. See what foods are at home before purchasing more.
How many times have you returned from shopping, only to discover you already had that bag of carrots tucked away in the back of the refrigerator? But by taking an inventory of what we have and creating a list of what is needed, we can all reduce waste. When shopping, encourage people to start with the outside isles, which generally display healthier foods while avoiding the center and display isles. Incorporating favorite cultural foods into the shopping list and eating foods in various forms including fresh, frozen, canned, and dried, can add to the variety and affordability.
Practice gratitude for your body by giving it the fuel it needs.
Choosing foods that nourish our body and expressing gratitude for the labor and work that went into harvesting and preparing our food, can improve our relationship with food. Making meals at home, by ourselves or with people we live with, can create connections and joy. By learning cooking and meal preparation skills, people have the opportunity to try new foods and enjoy flavors from around the world. Taking time to enjoy our food by mindfully eating and creating long lasting memories with friends and family is a great place to get started on this journey to tasty and sustainable eating.
Happy Nutrition Month everyone and thank you for considering these small changes, which when added up, make a big difference.
Visit the CDR Website for more great ideas and to access a bounty of free resources.
Want to learn more about Medical Nutrition Therapy?
You are invited to join our Virtual Conference with our Nutrition expert speaker, Ashley LaBrier, MS, RD, CDCES, who will be providing a half-day presentation on this important topic!

Ashley LaBrier, MS, RD, CDES, is an innovator in the field of diabetes, nutrition, and technology. Ashley is a consultant and the Diabetes Education Program Coordinator at the Salinas Valley Medical Clinic’s Diabetes & Endocrine Center.
Ms. LaBrier is passionate about providing person-centered education to empower those who live with diabetes. Having been diagnosed with type 1 diabetes herself nearly 20 years ago, she combines her professional knowledge with personal experience and understanding.
Virtual DiabetesEd Training Conference

Whether you are new to diabetes or a seasoned expert, you’ll benefit from this virtual conference with the latest research plus critical content that you can immediately apply to your clinical practice.
If you are seeking a state-of-the-art review of current diabetes care, this course is for you. Our team has been fine-tuning this course for over fifteen years, and we know what you need. This program can also be a great addition to your CDCES or BC-ADM exam study plan.
Group discounts are available!*
Download Course Flyer | Download Schedule
All hours earned count toward your CDCES Accreditation Information
Sign up for Diabetes Blog Bytes – we post one daily Blog Byte from Monday to Friday. And of course, Tuesday is our Question of the Week. It’s Informative and FREE! Sign up below!
The use of DES products does not guarantee the successful passage of the CDCES exam. CBDCE does not endorse any preparatory or review materials for the CDCES exam, except for those published by CBDCE.
New Type 1 Diabetes Treatment Approved – More Expansive Screening Needed?
With the approval of Tzield (teplizumab-mzwv), an anti-CD3 monoclonal antibody, we can now offer children 8 years and older an opportunity to delay the progression to type 1 diabetes for up to two years or longer and improve beta cell function.
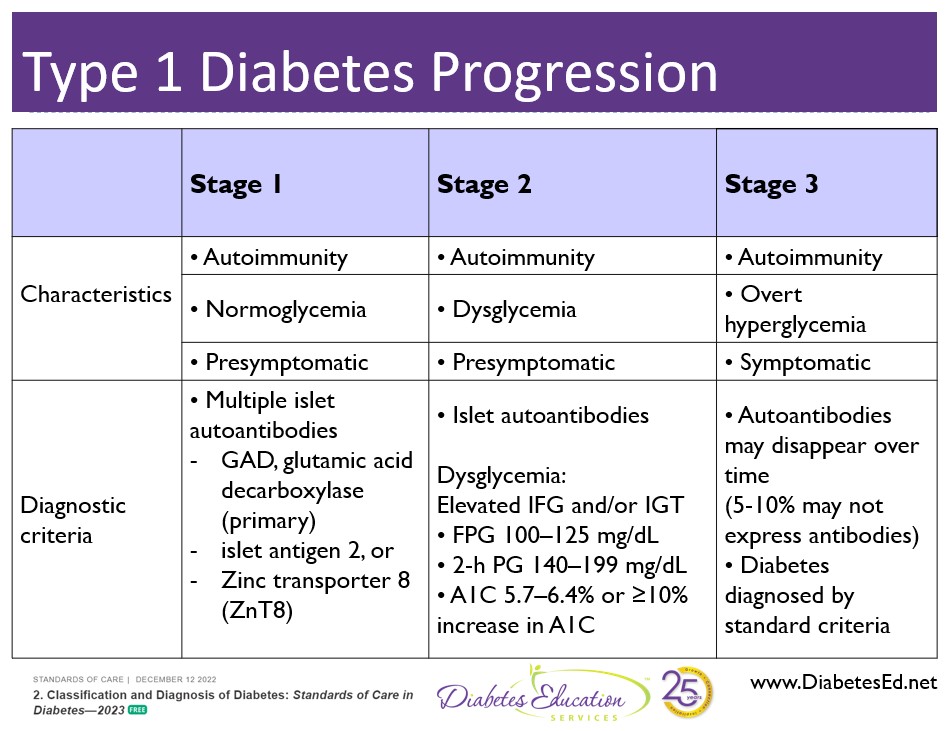
Teplizumab is the first disease-modifying therapy that impedes the progression of type 1 diabetes by binding to the surface of T cells to dampen the unwanted immune system response. It can delay the onset of symptomatic stage 3 type 1 diabetes in adults and children 8 years and older with stage 2 type 1 diabetes (see staging chart).
It is administered by intravenous infusion once daily for 14 consecutive days and is expected to cost in the region of $200,000 for the course of treatment.
Teplizumab is indicated for the individual in stage 2 type 1 diabetes, or for those with two or more islet autoantibodies and abnormal glycemia but still asymptomatic. People with stage 2 type 1 diabetes, have a nearly 100% lifetime risk of progression to clinical (stage 3) type 1 diabetes and a 75% risk of developing the condition within 5 years.
Results from a landmark clinical type 1 prevention trial conducted by TrialNet showed that with a two-week course of teplizumab:
- 72% of people in the control group developed clinical diabetes, compared to only 43% of the teplizumab group.
- The median time for people in the control group to develop clinical diabetes (stage 3) was just over 24 months, while those in the treatment group had an average of 48 months before progressing to clinical diabetes (stage 3).
Insulin production in response to glucose was impaired in the participants before they enrolled in the trial. In participants given an inactive placebo, insulin production declined through the first six months of the study. But in those treated with teplizumab, insulin production improved after treatment.
These results suggest that a single course of Teplizumab may provide long-lasting improvement in beta cell function. This, in turn, could delay or even prevent the development of type 1 diabetes in high-risk individuals.
More Screening for Type 1 Needed?
The ability to halt the progression of stage 2 type 1 diabetes from progressing to symptomatic stage 3 diabetes brings the prospect of more wide spread screening for type 1 into sharper focus. Currently, 40-50% of new type 1 diabetes is diagnosed when the individual is admitted to the hospital in a life-threatening hyperglycemic crisis or DKA. Studies suggest, identifying children at risk of future type 1 could avert DKA presentation, saving hundreds of thousands of dollars in hospital costs and allowing for early CD3 monoclonal antibody intervention.
Based on data from Trialnet, even though type 1 diabetes runs in families, 85 – 90% of people don’t have a first-degree relative with type 1 diabetes. That means, broader screening initiatives will be needed to identify those at risk for type 1 and eligible for the benefits of Teplizumab therapy.
Universal genetic or antibody screening in the future?
The Juvenile Diabetes Research Foundation is working toward a two-pronged screening approach.
This includes testing infants at birth with a genetic risk score combined with antibody screening. With this approach, providers can monitor kids with high genetic risk scores – based on human leukocyte antigen haplotypes, and provide education to family members regarding signs of hyperglycemia. In addition, antibody screening can help identify the stage of autoimmunity and help guide treatment action.
Researchers now have solid proof that immunotherapy can slow the progression of type 1 diabetes. This offers hope to conduct additional studies to extend the benefits of teplizumab, while continuing to test other immune therapies. Keep posted!
Virtual DiabetesEd Training Conference

Whether you are new to diabetes or a seasoned expert, you’ll benefit from this virtual conference with the latest research plus critical content that you can immediately apply to your clinical practice.
If you are seeking a state-of-the-art review of current diabetes care, this course is for you. Our team has been fine-tuning this course for over fifteen years, and we know what you need. This program can also be a great addition to your CDCES or BC-ADM exam study plan.
Group discounts are available!*
Download Course Flyer | Download Schedule
All hours earned count toward your CDCES Accreditation Information
Sign up for Diabetes Blog Bytes – we post one daily Blog Byte from Monday to Friday. And of course, Tuesday is our Question of the Week. It’s Informative and FREE! Sign up below!
The use of DES products does not guarantee the successful passage of the CDCES exam. CBDCE does not endorse any preparatory or review materials for the CDCES exam, except for those published by CBDCE.
February 2023 eNews | Insulin $35 Cap, New SGLT-2i, Scholarships & Sale
Happy February
February is the month we celebrate love.
In my opinion, love is at the center of providing diabetes care and education. We open our hearts as we carefully listen to people share their stories about living with diabetes. We celebrate successes and grieve losses alongside the individuals we serve every day. We speak our hearts when we advocate for evidence-based care that enhances well-being and improves outcomes.
In celebration of the compassionate contributions of diabetes care and education specialists, we are excited to announce our “Spreading the Love” Sale during the week of Valentine’s Day.
This month, we are delighted to share our updated Diabetes Education Services logos, celebrating 25 years of growth, connection, and inspiration. Keep your eyes open for website and online communications that include our freshened-up logo coupled with a 25.
For this month’s newsletter, we highlight the new Medicare $35 Insulin cap, discuss how treatments to delay type 1 diabetes might lead to childhood screening, announce a new SGLT-2i and of course test your knowledge with our Question and Rationale of the Week.
Lastly, we are offering two “Making a Difference” Scholarships, which provide a pair of deserving recipients with free registration for our Virtual DiabetesEd Training Course in late April.
It has been a complete joy to serve our community and provide meaningful courses, newsletters, blogs, cheat sheets, and content that makes a real difference in people’s lives since 1998. Who knows what we will come up with in the next 25 years?
With gratitude for our amazing community,
Coach Beverly and Bryanna
Featured Articles
- Insulin Cap of $35 for Medicare
- New “Savvy” SGLT-2i approved.
- Type 1 Diabetes Delay
- Making a Difference Scholarship for Virtual Conference
- Question of the Week
- Rationale of the Week
Upcoming Webinars
- ADA Standards Update – Feb 2nd at 11:30am PST
- Level 3 Boot Camp Series
- Upcoming Events – See complete calendar listing
- Virtual DiabetesEd Training Conference – April 26th
- BC-ADM Prep Webinar- Feb 20th
Want to learn more about Diabetes Care?
Virtual DiabetesEd Training Conference | Earn 30+ CEs

Whether you are new to diabetes or a seasoned expert, you’ll benefit from this virtual conference with the latest research plus critical content that you can immediately apply to your clinical practice.
If you are seeking a state-of-the-art review of current diabetes care, this course is for you. Our team has been fine-tuning this course for over fifteen years, and we know what you need. This program can also be a great addition to your CDCES or BC-ADM exam study plan.
Group discounts are available!*
Download Course Flyer | Download Schedule
All hours earned count toward your CDCES Accreditation Information
Sign up for Diabetes Blog Bytes – we post one daily Blog Byte from Monday to Friday. And of course, Tuesday is our Question of the Week. It’s Informative and FREE! Sign up below!
The use of DES products does not guarantee the successful passage of the CDCES exam. CBDCE does not endorse any preparatory or review materials for the CDCES exam, except for those published by CBDCE.
January 2023 eNews | 3 Important Diabetes Standards Updates
Happy 2023
Every year, Coach Beverly excitedly waits for the release of the new ADA Standards of Care. She loves scanning through the pages of content to discover updates and advances that lead to improved diabetes care. She then translates this new information into her presentations, updates her Cheat Sheets, and refreshes web content to reflect the latest guidelines.
Coach Beverly has discovered three real gems that she is excited to share with all of you.
In this first newsletter of 2023, we feature the new blood pressure and lipid guidelines based on ADA Standard 10. Plus, we explore changes to the Medication Algorithm for Type 2 Diabetes as featured in Standard 9, with a discussion on starting insulin versus an incretin mimetic.
We have updated our images for Question and Rationale of the Week and we invite you to test your knowledge below and review the rationale for the best answer.
Our Cheat Sheets are updated to reflect the 2023 Standards, so you can download these helpful references and study tools. The ever-popular Medications and Glucagon 2023 PocketCards are back from the printer and ready for purchase.
January marks the month we kick off our Level 1 Series. In February, we present our annual ADA Standards of Care update webinar and Level 3 Boot Camp Course Series.
For our 25-year celebration, we have several special events planned that we will be rolling out in the Spring. Stay tuned for an exciting 2023.
With gratitude for our amazing community,
Coach Beverly and Bryanna
Featured Articles
- New Blood Pressure Target & Interventions
- New Lipid Goals
- Insulin or Incretin Mimetics?
- Updated FREE Cheat Sheets
- Question of the Week
- Rationale of the Week
Upcoming Webinars
- Level 1 Series
- ADA Standards Update
- Level 3 Boot Camp Series
- Upcoming Events – See complete calendar listing
Want to learn more about this question? Enroll in our upcoming
Level 1 | Diabetes Fundamentals 2023 Updates | 9+ CEs
This bundle is specifically designed for healthcare professionals who want to learn more about diabetes fundamentals for their clinical practice or for those who are studying for the Certified Diabetes Care and Education Specialist (CDCES) exam.
Intended Audience: This library of critical information is designed for individuals or groups of diabetes specialists, including RNs, RDs, Pharmacists, Nurse Practitioners, Clinical Nurse Specialists, Physician Assistants, and other health care providers interested in staying up to date on current practices of care for people with diabetes and preparing for the CDCES Certification Exam.
2023 Webinar Updates
- January 10, 2023 – Class 1 – Getting to the Nitty Gritty 1.5 CEs
- January 12, 2023 – Class 2 – Nutrition and Exercise 1.5 CEs
- January 17, 2023 – Class 3 – Meds Overview for Type 2 – 1.5 CEs
- January 19, 2023 – Class 4 – Insulin Therapy & Pattern Management 1.5 CEs
- January 24, 2023 – Class 5 – Goals of Care – 1.5 CEs
- January 26, 2023 – Class 6 – Hypoglycemia, Sick Days, Monitoring, Foot Care 1.5 CEs
All hours earned count toward your CDCES Accreditation Information
Sign up for Diabetes Blog Bytes – we post one daily Blog Byte from Monday to Friday. And of course, Tuesday is our Question of the Week. It’s Informative and FREE! Sign up below!
The use of DES products does not guarantee the successful passage of the CDCES exam. CBDCE does not endorse any preparatory or review materials for the CDCES exam, except for those published by CBDCE.
December 2022 eNews | Improved Insulin PocketCard and a Little Tenderness
December Greetings

We decided to get a little personal and share some tenderness, alongside our newsy pieces, for this month’s newsletter.
For Coach Beverly, three words come to mind when she considers her family and business this year: reopening, celebration, and reflection. In her article, Beverly shares insights on the evolution of her company and her family over the past 24 years, including a historical photo of her first-ever Medication PocketCard.
Bryanna shares news on her two recent adoptees, Biscuit and Muffin. They are each adorable in their own way, and Bryanna hopes that they will eventually bring out the best in each other.
We welcome Andrew, a nursing student and new team member to our Diabetes Education Services family.
On the news front, we made significant changes to the timing section of our Insulin Medication PocketCards. We have also added Rezvoglar to the Lantus biosimilar list.
You’re invited to take the Question of the Week and read about the ADA/EASD consensus report with our Rationale of the week.
Finally, we want to turn the spotlight on you! We are forever grateful for your willingness to support and believe in a young Diabetes Specialist who had the vision to create a company that uplifts people with diabetes through a blend of science and compassion.
To thank you, our amazing community of diabetes educators and advocates, we will be celebrating our 25th Anniversary throughout 2023 with special events and giveaways. We can’t wait!
In celebration,
Coach Beverly and Bryanna
Featured Articles
- Insulin PocketCard Update
- Coach Bev Reflects
- Meet Biscuit and Muffin
- Welcome Andrew
- Question of the Week
- Rationale of Week
- Meds for Type 2 Webinar
- Upcoming Events – See complete calendar listing
FREE Resources
December Live Webinar Schedule
Join us for our Live Webinar 2023 Updates!
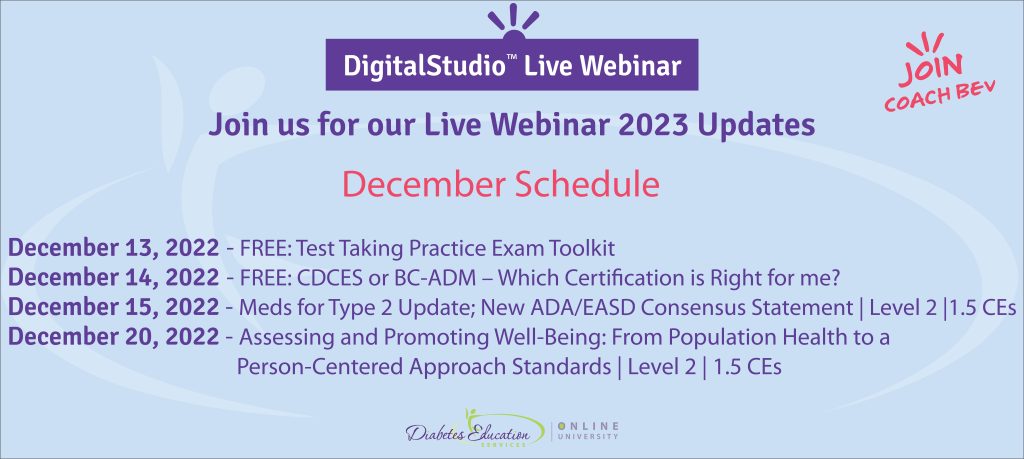
December 13, 2022 – FREE: Test Taking Practice Exam Toolkit
December 14, 2022 – FREE: CDCES or BC-ADM – Which Certification is Right for me?December 15, 2022 – New ADA/EASD Meds Consensus Update| Level 2 |1.5 CE’s
December 20, 2022 – Assessing Well-Being: A Person-Centered Approach | 1.5 CEs
Sign up for Diabetes Blog Bytes – we post one daily Blog Byte from Monday to Friday. And of course, Tuesday is our Question of the Week. It’s Informative and FREE! Sign up below!
The use of DES products does not guarantee the successful passage of the CDCES exam. CBDCE does not endorse any preparatory or review materials for the CDCES exam, except for those published by CBDCE.
Coach Bev Reflects and Prepares for an Exciting 2023

Three words come to mind when I consider my family and business this year: reopening, celebration, and reflection.
From the start, my wonderful husband and boys have been amazing Diabetes Education Services cheerleaders. They are not only enthusiastic supporters, they roll up their sleeves and help package orders, stuff PocketCards, and run errands for emergency supplies. Both of my boys worked at my company throughout high school and contributed so much in terms of new ideas and products.
As I wrap up my year, I wanted to share a little about me and my family with all of you.
I am thrilled that life has opened up again. It has been so fun to go to football games to watch my high school senior, Jackson leads the marching band as drum major. Our troupe started dancing again and we were invited to perform at a local art museum for a fundraiser. Our family traveled and traipsed all around Scotland and visited family in London. Plus, for the first time in over 2 years, I taught two diabetes seminars LIVE and in person. There is nothing like the deep and profound connection made with others in a shared community.
My oldest son Robert is moving beautifully into adulthood as he studies finance and navigates college life and internships. My younger son, Jackson, loves chemistry and is busy writing essays about his goals and life experiences for college. I have so enjoyed reviewing these essays and learning new details about this wonderfully curious human. My husband continues his work as a critical care pharmacist and hopes to start a residency program at our local community hospital in the future.
Celebration and Reflection:
Diabetes Education Services Marks 25 years in 2023
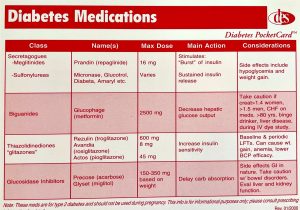
I started Diabetes Education Services in May of 1998, just after the world wide web was introduced and sending messages through something called “email” was possible. At first, my one-person company only offered live courses at hospitals and meeting sites around the country. To engage new customers, I created a 2-sided Medication Post Card (see image), that we would mail out for free in exchange for an email address. My whole family helped me stuff envelopes and handwrite addresses in an effort to grow our community.
My administrative space consisted of a 10×12 foot room in our home, where I juggled writing my monthly newsletter and updating slides, all while raising two busy toddlers. In 2010, I took a leap of faith and decided to try offering courses online. In addition, I hired an amazing marketing team to redo my website and make sure it accurately reflected our company values and message of inclusion and kindness.
Fast forward to today. We have since grown our business to include an amazing team of employees and a newsletter that reaches over 37,000 online subscribers. Our Online University includes over 50 CE courses that we update yearly, plus we offer a CDCES Coach app, blogs, an 8-sided PocketCard, keynote presentations, and more. Our working space has expanded to a studio just steps from my home. This spacious office has room to store all our books and teaching tools plus offers lots of natural light, a view of my pond with abundant bird visitors, and an upstairs recording studio.
2023 is a Year of Gratitude
The truth is, we couldn’t have done any of this without YOU, our community. I am forever grateful for your willingness to support and believe in a young Diabetes Specialist who had the vision to create a company that uplifted people with diabetes through a blend of science and compassion.
To thank our amazing community of diabetes educators and advocates, we will be celebrating our 25th Anniversary throughout the year. Stay tuned. We can’t wait to see what the future holds!
FREE Resource Catalog
- Diabetes Cheat Sheets
- Diabetes Blog Bytes
- Medication PocketCards
- Start Your Certification Journey
- CDCES Coach App
- Free Webinars hosted by Coach Beverly
- Question of the Week

See Full Free Resource Catalog
Sign up for Diabetes Blog Bytes – we post one daily Blog Byte from Monday to Friday. And of course, Tuesday is our Question of the Week. It’s Informative and FREE! Sign up below!
The use of DES products does not guarantee the successful passage of the CDCES exam. CBDCE does not endorse any preparatory or review materials for the CDCES exam, except for those published by CBDCE.
October 2022 eNews | Why I Transformed my Approach to Diabetes Care

October Greetings
A few years ago, I drastically changed my approach to diabetes self-management education as a result of participating in the Embark Trial Research Team.
To my surprise, the innovative coaching techniques I learned and applied in the Embark study upped my game and improved my skills. With this new approach, I feel a deeper sense of connection and experience more success when providing care to people with diabetes.
The good news is that we are ready to share these techniques with you. We have reassembled the Embark Instructional team to provide the evidence-based tools and the step-by-step approach in our ReVive 5 Diabetes Training Program.
We distilled the most important skills and content from the Embark study and packaged it into our four-session ReVive 5 Program.
ReVive 5 Training Program – First session FREE
Our first ReVive 5 class of the four-session series starts November 1st. Good news! As part of our opening launch celebration, we are inviting you to join the first training session for FREE.
For this newsletter, we feature interviews from the Embark Training and Research Team. Enjoy the wisdom of these two amazing pioneers in the field of Diabetes Distress. Plus, Coach Beverly shares the impact of the trial on her approach.
If you feel like a challenge, take a moment to check out our Question and Rationale of the Week. We are excited to announce our New and Improved Online University is up and running. You are invited to stop by, kick off your shoes and get comfy.
In recognition of Indigenous Peoples’ Day, we are honored to share the poem, “Remember” by Poet Laureate, Joy Harjo.
Thank you for caring and advocating on behalf of people living with diabetes. With gratitude,
Beverly, Bryanna, and Amanda
Featured Articles
- Why Coach Bev Transformed Her Approach to DSME
- Do you Have to be a Mental Health Expert to Provide Diabetes Care?
- Biggest Lessons from Addressing Diabetes Distress
- Question of the Week
- Rationale of the Week
Upcoming Webinars
- ReVive 5 Diabetes Training
- FREE ReVive Session 1
- New, Improved DiabetesEd Online University
- Free Resources
- “Remember” by Poet Laureate, Joy Harjo
- Free Resources
Want to learn more about this question? Join our NEW
ReVive 5 Diabetes Training Program

Whether you are a novice or an expert in providing diabetes care, we invite you to attend this exciting training program that provides the essential steps to address diabetes distress combined with an innovative approach to glucose management that will revolutionize your practice.
“ReVive 5” breathes new life into our relationship with diabetes, bringing a fresh perspective to both the person with diabetes and the provider.
By releasing old habits that no longer serve us, we have the opportunity to create a new life tool kit toolkit in partnership with the person living with diabetes.
The ReVive 5 program is built on international research study results and will revolutionize your approach to diabetes self-management education.
Join our Team of Experts
Team of Experts:
ReVive 5 is taught by a team of 3 Interdisciplinary Experts:
- Lawrence Fisher, Ph.D., ABPP, Professor Emeritus, UCSF
- Susan Guzman, PhD
- Beverly Thomassian, RN, MPH, CDCES, BC-ADM
Training Program Includes:
- 14.0 CEs – Includes the 4 Session ReVive Training Program, Certificate and 5 FREE bonus courses to supplement content
(Four 1.5 hour training sessions (6.0 CEs) plus Five bonus courses worth 9.0 CEs) - Quarterly 1 hour follow-up sessions with an expert -dates to be announced
- A comprehensive set of assessment tools, educational materials, log sheets and resources.
Don’t worry if you can’t make it live. Your registration guarantees access to the recorded version in the Online University.
All hours earned count toward your CDCES Accreditation Information
Sign up for Diabetes Blog Bytes – we post one daily Blog Byte from Monday to Friday. And of course, Tuesday is our Question of the Week. It’s Informative and FREE! Sign up below!
The use of DES products does not guarantee the successful passage of the CDCES exam. CBDCE does not endorse any preparatory or review materials for the CDCES exam, except for those published by CBDCE.








