
Subscribe
eNewsletter

Ready to get certified?
Free CDCES Coach App
Download
Free Med Pocket Cards
Virtual DiabetesEd Specialist Conference | April 15-17, 2021

Whether you are new to diabetes or a seasoned expert, you’ll benefit from this virtual conference with the latest research plus critical content that you can immediately apply to your clinical practice.
Entire Program Fee: $399
Dates: April 15-17, 2021
Live Webinar Schedule: All webinars start and end times are in Pacific Standard Time
Coach Beverly Thomassian, RN, MPH, BC-ADM, CDCES

Author, Nurse, Educator, Clinician and Innovator, Beverly has specialized in diabetes management for over twenty years. As president and founder of Diabetes Educational Services, Beverly is dedicated to optimizing diabetes care and improving the lives of those with diabetes.
Diana Isaacs, PharmD, BCPS, BC-ADM, BCACP, CDCES

We are thrilled to welcome our newest speaker, Diana Isaacs, who will be joining our Virtual and Live Courses!
Dr. Isaacs was named 2020 AADE Diabetes Educator of the Year for her educational platform promoting the use of CGM for people with diabetes and other innovations. Dr. Isaacs was awarded the Ohio Pharmacists Association Under 40 Award in 2019. Dr. Isaacs has served in leadership roles for several pharmacies and diabetes organizations. She has numerous diabetes publications and research projects with a focus on medications, CGM and diabetes technology.
As the CGM Program Coordinator and clinical pharmacist specialist in the Cleveland Clinic Diabetes Center, Dr. Isaacs brings a wealth of clinical knowledge combined with extensive research experience to this program.
Diabetes Meds and Insulin Toolkit – with Dr. Diana Isaacs | 4.0 CEs
April 15 10:30 am – 12:30 BREAK and 1:15 – 3:15 PST
*Topics include:
Technology Toolkit with CV Management Update – Dr. Diana Isaacs | 4.0 CEs –
April 16 with 8:30—12:30 am
Ashley LaBrier, MS, RD, CDCES

Ashley is an educator, dietitian, and the Diabetes Education Program Coordinator at the Salinas Valley Medical Clinic’s Diabetes & Endocrine Center. Her work with people living with diabetes focuses on the value of healthy nutrition and movement to improve well-being.
Ashley is passionate about providing person-centered education to empower those who live with diabetes. Having been diagnosed with type 1 diabetes herself nearly 20 years ago, she combines her professional knowledge with personal experience and understanding.
April 17 with Ashley LaBrier, MS, RD, CDCES
8:30 am — 12:30 pm PST
*Dates and times subject to change. Course start and end time are for Pacific Standard Timezone.
Bonus Courses – Course registration includes FREE enrollment into our Level 2 Standard of Care Course Series including:
Team of expert faculty includes:
In addition to informative lectures, we also use group activities and case studies to highlight the essential knowledge, skills, and strategies needed to succeed in diabetes education today!
Prepare for CDCES or BC-ADM certification or earn hours for renewal.
Your registrations include access to all the Online Sessions plus Bonus Courses through December 31st, 2021.
This virtual program includes:
3 day live webinar courses from April 15th-17th (20 CEs) + enrollment in our Bonus Bundle (14.0+ CEs) from now through December 2021.
View full Conference Schedule and Faculty.
Sign up for Diabetes Blog Bytes – we post one daily Blog Byte from Monday to Friday. And of course, Tuesday is our Question of the Week. It’s Informative and FREE! Sign up below!
[yikes-mailchimp form=”1″]Accreditation: Diabetes Education Services is an approved provider by the California Board of Registered Nursing, Provider 12640, and Commission on Dietetic Registration (CDR), Provider DI002. Since these programs are approved by the CDR it satisfies the CE requirements for the CDCES regardless of your profession.*
The use of DES products does not guarantee the successful passage of the CDCES exam. CBDCE does not endorse any preparatory or review materials for the CDCES exam, except for those published by CBDCE.

Dawn Desoto RD, CDCES, celebrates the winter season with a collection of recipes that nourish and provide comfort.
Yield 2 servings

Directions
Simply pour all ingredients into a small saucepan, whisk to combine ingredients. Heat until hot to the touch but not boiling – about 4 minutes. Enjoy warm.

Directions
Combine is a small saucepan and whisk until the consistency is smooth and silky. Pour into mugs. Give thanks. Enjoy.

Directions
Toss whole mushrooms, olive oil, and salt and pepper to taste in a bowl. Spread on a baking dish and roast at 425 degrees F, stirring a few times, until tender and browned for 30 to 35 minutes. Cook thinly sliced garlic cloves and smoked paprika in butter until soft, toss with the mushrooms. Sprinkle with chopped parsley and salt. Enjoy.

Instructions
We hope you enjoy these delicious recipes!
Written by Dawn DeSoto RD, CDCES, our resident Nutrition Content Writer
Sign up for Diabetes Blog Bytes – we post one daily Blog Byte from Monday to Friday. And of course, Tuesday is our Question of the Week. It’s Informative and FREE! Sign up below!
[yikes-mailchimp form=”1″]Accreditation: Diabetes Education Services is an approved provider by the California Board of Registered Nursing, Provider 12640, and Commission on Dietetic Registration (CDR), Provider DI002. Since these programs are approved by the CDR it satisfies the CE requirements for the CDCES regardless of your profession.*
The use of DES products does not guarantee the successful passage of the CDCES exam. CBDCE does not endorse any preparatory or review materials for the CDCES exam, except for those published by CBDCE.

Not having our basic needs met, like limited access to food, has a dramatic impact on our mental health.
The pandemic has significantly impacted our mental health due to the trauma, social isolation, and economic instability which has led to an increase in food insecurity.
Since the start of the pandemic, the number of families experiencing food insecurity has increased dramatically, from 8.1% to 10.0% from March to June 2020.
As Diabetes Care & Education Specialists, we realize how important access to healthy, nutritious foods are for diabetes self-care and mental health. Addressing food insecurity and providing resources to fill in gaps, can be a lifeline and improve mental health for people living with diabetes.
A recent study led by Jason M. Nagata, MD, MSc, who works in the Division of Adolescent and Young Adult Medicine, Department of Pediatrics, at UCSF dove into the correlation between food insecurity and mental health.
“Food insecurity is associated with diets high in low-cost, energy-dense packaged foods, but low in fruits and vegetables, which may lead to chronic medical conditions such as diabetes and hypertension, both of which are known to be associated with a higher risk for severe COVID-19 illness” the study states.
The study highlights how different populations are more at risk of experiencing food insecurity with lower-income, single individuals or large families, people of color, those recently unemployed, and people younger in age being the most affected.
Food access disparities that disproportionately affect people of color and low-income individuals and families have been an ongoing public health concern, even before the pandemic.
The study by Dr. Nagata and team cites the term “food apartheid” which activist Dara Cooper describes as the “blatantly discriminatory corporate-controlled food system that results in [communities of color] suffering from some of the highest rates of heart disease and diabetes of all time.”
Food shortages due to border closures, essential workers falling ill, school closures that provided meals to over 35 million children pre-pandemic, and the overall economic crisis, have exasperated food insecurity.
“Food insecurity may lead to poor mental health through chronic stress, stigmatization, and perceived powerlessness. Conversely, people experiencing poor mental health symptoms may be less able to work, generate income, or manage financial resources, which could exacerbate food insecurity.”
The study used cross-sectional data from the U.S. Census Household Pulse Survey that was collected and analyzed in 2020 across 63,674 participants. Those who experienced food insufficiency in the past 7 days were more likely to experience mental health outcomes such as anxiety, worry, anhedonia, and depression.
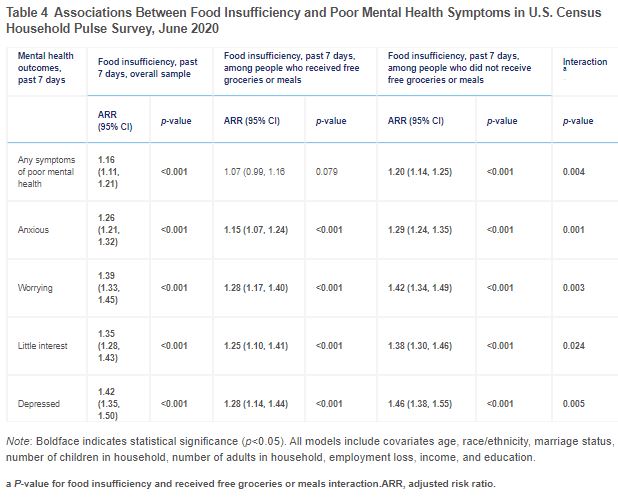
The study concludes that assistance programs that provide free meals, financial assistance, paid sick leave, mental health resources, and stimulus funding can help decrease the cycle of food insecurity and improve mental health outcomes.
To read more, click here to view the study.
Click here to read more about food apartheid.
Written by Bryanna, our Director of Operations & Customer Happiness
The National CLAS Standards website (https://thinkculturalhealth.hhs.gov) offers a number of resources and materials that can be used to improve the quality of care delivery to non–English-speaking patients
The ADA provides a list of mental health providers who have received additional education in diabetes at the ADA Mental Health Provider Directory (professional.diabetes.org/mhp_listing).
This course is an essential review for anyone in the field of diabetes. This course summarizes the 2021 updates to the American Diabetes Association’s Standards of Medical Care in Diabetes and provides critical teaching points and content for health care professionals involved in diabetes care and education.
Earn 2.0 CEs and get ready to lead the charge to implement best care practices for the New Year.
Topics Include:
Sign up for Diabetes Blog Bytes – we post one daily Blog Byte from Monday to Friday. And of course, Tuesday is our Question of the Week. It’s Informative and FREE! Sign up below!
[yikes-mailchimp form=”1″]
Accreditation: Diabetes Education Services is an approved provider by the California Board of Registered Nursing, Provider 12640, and Commission on Dietetic Registration (CDR), Provider DI002. Since these programs are approved by the CDR it satisfies the CE requirements for the CDCES regardless of your profession.*
The use of DES products does not guarantee the successful passage of the CDCES exam. CBDCE does not endorse any preparatory or review materials for the CDCES exam, except for those published by CBDCE.
Humans are hard-wired to seek comfort and relief in moments of stress.
Biologically, this is called homeostasis, which means maintaining a steady state of balance.

With the ongoing trauma of the pandemic, many of us are seeking comfort and a way to occupy our minds. Many people have adopted new hobbies to keep themselves busy, with sourdough bread baking being a popular choice. Bread products are comfort for many of us. I have not made bread as many others have, but I have been craving bread products and eating more bread, potatoes, and ice cream.
“Anything that challenges our state of balance, or any situation of lack, is deemed a stressor. This could be hunger, an uncomfortable position, feeling cold, or feeling afraid or insecure,” Dr. Eva Selhub, resiliency expert explains.
This feeling triggers an automatic reaction to leave or alleviate the uncomfortable situation, like putting on something warm if you are cold, or overeating when you are feeling insecure.
“By addressing the problem, the brain’s reward centers are stimulated along with the release of neurotransmitters like dopamine and serotonin”, continues Dr. Selhub.
At the same time, the stress hormone cortisol goes down. Solving a discomfort, then, gives us a sense of euphoria and ease. Also, carbohydrates especially lead to the increase of serotonin, the happiness hormone, which gives us the sense of feeling better.
According to Julie Ohana, a culinary art therapist, (culinary art therapy helps people communicate and manage stress through cooking), “there is a big reason people have been stress baking. When times are turned upside down we look for ways to cope”, she says. “The heart of the explanation is that cooking and baking bring comfort. The process helps aid the baker and the finished product helps comfort the person or people receiving the delicious outcome. Having control over something right now is important since so much in the world is unknown and out of our hands. When I am in the kitchen, I know what I can expect. For many, the act of baking is also calming because baking is a form of mindfulness. When we are inundated by the news and scary information, it’s important that we all take time away from the scary stuff and reset our minds and thoughts.”

Cooking sourdough bread and binge eating carbohydrates might be physiologically and psychologically comforting for some, but for our clients living with diabetes, carbohydrate cravings and binge eating can play havoc on blood sugar control, weight management, and emotional health. I had a client confide in me that when a friend brought her a warm loaf of sourdough bread she ate the whole loaf in one sitting.
TW: Mention of eating disorders below
Binge eating disorder (BED) is a severe, life-threatening, but treatable eating disorder. It is characterized by periods of uncontrolled, impulsive, or continuous eating beyond the point of comfortably full. BED is one of the newest eating disorders formally recognized in the DSM-5. Bulemia is characterized by recurrent binge eating with purging. Anorexia is centered around an obsessive fear of weight gain and involves self-starvation and often excessive weight loss. Eating disorders affect 9% of the population. 28.8 million Americans will have an eating disorder in their lifetime. Eating disorders are among the deadliest mental illness, secondary only to opioid overdose. The global economic cost of eating disorders is $64.7 billion annually. (1)
Hotline calls to the National Eating Disorders Association are up 70-80% since the beginning of the pandemic. “The risk of eating disorders is going to increase whenever there are higher levels of stress,” Lauren Smolar, Senior Director for the National Association of Eating Disorders tells us.
A survey in the International Journal of Eating Disorders in July found 62% of people in the US with anorexia experienced a worsening of symptoms as the pandemic hit. Nearly a third of Americans with binge eating disorder reported an increase in episodes. (2)
Women with T1D have nearly 2.5 times the risk of developing an eating disorder compared to those without diabetes with bulemia is the most common eating disorder in women with T1D. (3) Among women with type 2 diabetes, BED is more common. “Diabulemia” is an eating disorder characterized by intentionally withholding insulin to result in weight loss. Diabulemia is shockingly common; as many as a third of women with T1D report insulin restriction.
Overeating sourdough bread or other foods in the pandemic may be a red flag to us as Diabetes Care and Education Specialists to screen for possible eating disorders. In my career as a dietitian and CDCES, I have seen a lot of people who struggle with eating disorders. With compassion, we can help our clients understand the psychology of why they are binge eating.
There are a number of virtual support groups and free resources currently being offered at nationaleatingdisorder.org. On this site, there is a five-minute quiz to help determine whether our clients might need professional support.
For me, comfort foods include foods with a variety of textures, flavors, and nutrients! This recipe is a favorite of mine.

Ingredients
Instructions
This article is written by our resident nutrition expert, Dawn DeSoto, RD, CDCES
Citations

Whether you are new to diabetes or a seasoned expert, you’ll benefit from this virtual conference with the latest research plus critical content that you can immediately apply to your clinical practice.
Entire Program Fee: $399
Program Flyer: Download
Dates: Recorded & Ready for Viewing!
Live Webinar Schedule: All webinars start and end times are in Pacific Standard Time
Program Schedule & Expert Bios
What is the Diabetes Educator Course?
If you are interested in taking the CDCES or BC-ADM exam or are seeking a state of the art review of current diabetes care, this course is for you. Our team of expert faculty has been fine-tuning this course for over fifteen years, and we know what you need. In addition to informative lectures, we also use group activities and case studies to highlight the essential knowledge, skills, and strategies needed to succeed in diabetes education today!
In this course, the same speakers will cover the same content as outlined in the Live Seminar. For more details see our Virtual DiabetesEd Specialist Conference Schedule and Faculty.
Prepare for CDCES or BC-ADM certification or earn hours for renewal.
Come join our Virtual DiabetesEd Specialist Program.
Your registrations include access to all the Online Sessions plus Bonus Courses through December 31st, 2021.
This virtual program includes:
3 day live webinar courses from April 15th-17th (20 CEs) + enrollment in our Bonus Bundle (14.0+ CEs) from now through December 2021.
View full Conference Schedule and Faculty.
Sign up for Diabetes Blog Bytes – we post one daily Blog Byte from Monday to Friday. And of course, Tuesday is our Question of the Week. It’s Informative and FREE! Sign up below!
[yikes-mailchimp form=”1″]Accreditation: Diabetes Education Services is an approved provider by the California Board of Registered Nursing, Provider 12640, and Commission on Dietetic Registration (CDR), Provider DI002. Since these programs are approved by the CDR it satisfies the CE requirements for the CDCES regardless of your profession.*
The use of DES products does not guarantee the successful passage of the CDCES exam. CBDCE does not endorse any preparatory or review materials for the CDCES exam, except for those published by CBDCE.
Roughly 22% of adults report having gained weight during the COVID-19 pandemic. (1)
COVID-19 has created a perfect storm for gaining unwanted weight. Insomnia, loneliness, depression, anxiety, decreased physical activity, and disruptions in our daily routines have increased chronic stress in our lives which can increase levels of the stress hormone cortisol. Cortisol is associated with increased food cravings and weight gain. (2)

Lately, I have been intrigued by the idea that the addition of umami could possibly help us achieve weight loss and increase our enjoyment of foods at the same time. Research shows foods with umami flavors tend to reduce people’s appetite without cutting their satisfaction with the meal. (5)
Umami is that rich, deep, indescribable flavor of lusciousness found in foods like Parmesan cheese, cured pork products, grilled or roasted meats, sausage, and soups and stews that have been slow-cooked for a long period of time. It occurs when glutamate breaks down into L-glutamate via fermentation, braising, or ripening. Glutamate alone, however, cannot produce the full flavor of umami. Instead, it arises from the combination of glutamate and ribonucleotides, molecules that serve as the building blocks for DNA and RNA. Interesting to me is that glutamate is also abundant in human breast milk; in fact, human milk contains as much glutamate as most savory broths.
In 2000 scientists at the University of Miami identified the first umami receptor on the taste buds lining the surface of our tongues. Mushrooms, especially dried shiitake mushrooms, are rich in umami. Umami-rich ingredients can be found in cooking ingredients/condiments. Naturally brewed soy sauce, Marmite, anchovy relish, miso, tomato puree, fish sauce, and Worcestershire sauce are all great sources of umami. Recently, many seasoning products have been developed with umami as the goal – such as Takii Umami Powder-Magic Shiitake Mushroom Seasoning, Trader Joe’s Mushroom & Company Multipurpose UMAMI Seasoning Blend, and Taste No 5 Umami Paste.

Umami was named more than a century ago by Kikunae Ikeda a chemist at Tokyo University. As Dr. Ikeda savored a simple bowl of broth, he pondered the nature of deliciousness. How was it a lightly simmered mixture of water, dried fish flakes, and a little bit of dried seaweed that could be so mouthwatering?
Dashi, the broth that set Ikeda on his quest in 1907, maintains an essential place in Japanese cuisine to this day. Over the course of a year, Dr. Ikeda boiled kombu, the dried seaweed, down into a tarry resin and stripped out salts and other organic compounds one by one. In the end, Dr. Ikeda harvested a single ounce of crystals strongly resembling the flavor of his bowl of dashi-a flavor that he called umami (roughly translated from the Japanese word for “delicious”).
The crystals producing the umami flavor turned out to be the amino acid glutamate. Hoping to provide cooks easy access to umami, he learned how to produce it in industrial quantities and patented the notorious flavor enhancer monosodium glutamate (MSG).
MSG was popular in the American food supply for decades. However, since 1968 the chemical has received bad publicity despite dozens of studies concluding that MSG is safe and the purported negative health claims found to have little supporting evidence. (6) Currently, MSG is popular in processed foods such as canned soups, frozen dinners, cold cuts, dressings, and Doritos. MSG can help reduce sodium in dishes without compromising flavor because of umami. MSG contains 1/3 the amount of sodium as table salt.
Since the pandemic, I have been cooking more and experimenting with creating physically nourishing and emotionally satisfying meals. Consciously including umami has been an exciting part of this experiment.

Directions: Toss 2 pounds whole mixed mushrooms, 1 ½ tablespoons olive oil, and salt and pepper to taste in a bowl. Spread on a baking dish and roast at 425 degrees F, stirring a few times, until tender and browned for 30 to 35 minutes. Cook 3 thinly sliced garlic cloves and ½ tsp smoked paprika in butter until soft, toss with the mushrooms. Sprinkle with chopped parsley and salt. Enjoy.
This article is written by our resident nutrition expert, Dawn DeSoto, RD, CDCES
Citations
-Zachary Z, Brianna F, Brianna L, et al. Self-quarantine and weight gain related risk factors during the COVID-19 pandemic. Obes Res Clin Prat. 2020;14(3):210-216.
-Chao AM, Jastreboff AM, White MA, Grilo CM, Shinha R. Stress, cortisol, and other appetite-related hormones: Prospective prediction of 6-month changes in food cravings and weight. Obesity (Silver Spring). 2017 Apr:2594):713-720
-CDC November 19, 2004/53(45);1066-1068. Prevalence of Overweight and Obesity Among Adults with Diagnosed Diabetes-United States, 1988-1994 and 1999-2002
-Menke A, Casagrande S, Geiss L, Cowie CC. Prevalence of the Trends in Diabetes Among Adults in United States, 1988-2012. JAMA. 2015 Sep 8; 314(10):1021-9
-Masic U, Yeomans MR. Umami flavor enhances appetite but also increases satiety. The American Journal of Clinical Nutrition, Volume 100, Issue 2, August 2014, Pages 532-538.
-Zanfirescu A, Ungurianu A, Tsatsakis AM, Nitulescu GM, Kouretas D, Veskoukis A, Tsoukalas D, Engin AB, Aschner M, Margina D. A Review of the Alleged Health Hazards of Monosodium Glutamate. Compehensive Reviews in Food Science and Food Safety. 2019 May 8/18(4):1111-1134
This series is designed for health care professionals who are interested in getting started in diabetes education and for those actively working toward becoming a Certified Diabetes Care and Education Specialist. Each course in this series provides the critical building blocks and foundation for those entering the diabetes field. Plus, they prepare you to advance to our Level 2 Standards of Care Intensive Courses.
Join us for our 2021 Live Webinar Updates. All courses air at 11:30 a.m. (PST)

Instructor: Beverly Thomassian RN, MPH, CDCES, has been Board Certified in Advanced Diabetes Management for over 20 years. She is an Associate Clinical Professor at UCSF and Touro University and a nationally recognized diabetes expert.
Sign up for Diabetes Blog Bytes – we post one daily Blog Byte from Monday to Friday. And of course, Tuesday is our Question of the Week. It’s Informative and FREE! Sign up below!
[yikes-mailchimp form=”1″]
Accreditation: Diabetes Education Services is an approved provider by the California Board of Registered Nursing, Provider 12640, and Commission on Dietetic Registration (CDR), Provider DI002. Since these programs are approved by the CDR it satisfies the CE requirements for the CDCES regardless of your profession.*
The use of DES products does not guarantee the successful passage of the CDCES exam. CBDCE does not endorse any preparatory or review materials for the CDCES exam, except for those published by CBDCE.
The Winter Solstice, on December 21, marked the shortest day in the Northern Hemisphere. People in New York got just over 9 hours 15 minutes of sun, while those in Anchorage Alaska got fewer than 5.5 hours.

Lack of light can contribute to depression. The idea that people are more susceptible to depression in the winter months wasn’t picked up until the 1980’s when South African psychiatrist Norman Rosenthal moved to the US and noticed a change in his mood during the New York winters. Dr. Rosenthal, Dr. Al Lewy, and Dr. Thomas Wehr investigated and identified Seasonal Affective Disorder (SAD). In 1987 it was included in DSM.(1)
This winter 2020 is an extra dark one. A recent study showed that depression symptom prevalence was more than 3-fold higher during the COVID-19 pandemic than before. During the pandemic, many people are making a lower-income or have no income, have depleted their savings, and have more exposure to stressors, which were all associated with a greater risk of depression. (2)
Studies show that people with diabetes are more susceptible to depression. Depression is three times as prevalent in people with diabetes when assessed by self-report. The combination of diabetes and depression present a major clinical challenge as the outcomes of both conditions are worsened in the presence of the other. Quality of life is worse, diabetes self-management is impaired, the incidence of complications is increased, and life expectancy is reduced. (3)
Refer to mental health providers as needed. As I am writing this blog my sister texted me that she is feeling very sad, unmotivated, and just wants to sleep. Diabetes Education Services has resources to help us screen our clients for depression in the Psychological Care Assessment Resource Page.
Can food, in particular a golden spice, help those of us without the more serious clinical depression cope this winter with milder winter blues?
Turmeric is a plant with a very long history of medicinal use, dating back 4000 years. In parts of Southeast Asia, turmeric is used not only as a principal spice but also as a component in religious ceremonies.
Turmeric, derived from the root of Curcuma longa, a flowering plant of the ginger family, is a gold-colored spice commonly used in the Indian subcontinent, not only for health care but also for the preservation of food and as a yellow dye for textiles. Curcumin, which gives the yellow color to turmeric, was first isolated almost two centuries ago, and its structure as diferuloylmethane was determined in 1910.
Since the time of Ayurveda (1900 BCE) numerous therapeutic activities have been assigned to turmeric for a wide variety of diseases and conditions. Extensive research within the last half-century has proven that most of these activities, once associated with turmeric, are due to curcumin. Curcumin has been shown to exhibit antioxidant, anti-inflammatory, antiviral, antibacterial, antifungal, and anticancer activities. (4)
“Curcumin can influence several mechanisms in the body; in particular, it is a powerful natural anti-inflammatory and antioxidant. This has relevance to depression because people with depression have greater inflammation and oxidative stress, which can affect all major organs of the body, including the brain”, reports Adrian Lopresti, PhD., a clinical psychologist and researcher at the School of Psychology and Exercise Science at Murdoch University. (5)
Due to curcumin’s anti-inflammatory effect, a 2013 review of studies suggests that curcumin can decrease the level of glucose in the blood, as well as other diabetes-related complications. (6) 500-1000 mg of curcumin per day has been found to promote the anti-inflammatory effect. (7) 1 teaspoon of fresh turmeric has about 200 mg of curcuminoids. Curcumin’s bioavailability can be enhanced by 2000% by combining it with black pepper (piperine is the major active component). (8)
Try turmeric tea or add turmeric to scrambled eggs, to rice as it is cooking, to stews. You can also try my favorite before bed treat, Golden Milk.

Directions
Simply pour all ingredients into a small saucepan, whisk to combine ingredients. Heat until hot to the touch but not boiling – about 4 minutes. Enjoy warm.
Written by Dawn DeSoto RD, CDCES, our resident Nutrition Content Writer
References

We are updating this course to reflect the 2021 ADA Standards of Care. This presentation will include the latest information on Social Determinants of health, assessment strategies and approaches. We will explore the psychosocial issues that can discourage individuals from adopting healthier behaviors and provides strategies to identify and overcome these barriers.
Life studies are used to apply theory to real life situations. A great course for anyone in the field of diabetes education or for those looking for a new perspective on assessment and coping strategies.
Topics include:
This course is included in: Level 2 – Standards of Care Intensive. Purchase this course individually for $29 or the entire bundle and save 70%.
Enroll in our entire Level 2 – Standards of Care Intensive to join us for the below for Live Webinar Updates. All courses air at 11:30 a.m. (PST)
Sign up for Diabetes Blog Bytes – we post one daily Blog Byte from Monday to Friday. And of course, Tuesday is our Question of the Week. It’s Informative and FREE! Sign up below!
[yikes-mailchimp form=”1″]Accreditation: Diabetes Education Services is an approved provider by the California Board of Registered Nursing, Provider 12640, and Commission on Dietetic Registration (CDR), Provider DI002. Since these programs are approved by the CDR it satisfies the CE requirements for the CDCES regardless of your profession.*
The use of DES products does not guarantee the successful passage of the CDCES exam. CBDCE does not endorse any preparatory or review materials for the CDCES exam, except for those published by CBDCE.
I have been eating chocolate daily for years. I crave chocolate. I love chocolate.
I am not alone. About 7.3 million tons of retail chocolate confectionery were consumed globally in 2015/2016! (1)
My family holiday tradition is the gifting of See’s chocolates, but as I attempt to decrease my sugar intake, I have made a commitment to eat less chocolate.
Chocolate is made from tropical Theobroma cacao tree seeds. Its earliest use dates back to the Olmec civilization in Mesoamerica. The word cacao originated from the Mayan word, “Ka’Kau.” Ancient Aztecs considered Cacao the “Food of the Gods.” Cacao was a pillar of the Mayan, Aztec, and Nahua communities, economies, and religions as a sacred medicine.
In Mayan and Aztecan culture, cacao is a sacred crop and has historically been used for ceremonial practices, known as “Cacao Ceremony” or as offerings to the Gods.

Cacao and cocoa are both milled and processed from the cocoa bean, but cacao is processed at a low temperature and considered raw. Cacao contains antioxidants, vitamins, minerals, and protein.
Cocoa is the term used to refer to the heated form of cacao. Cocoa undergoes a higher temperature during the processing and some of the nutrients are lost, although it still retains antioxidants.
Cacao is stronger flavored than cocoa. Dutch-process cocoa is cocoa that has been treated with an alkalizing agent to modify its color and give it a milder taste. Dutch cocoa forms the basis for much of modern chocolate.
In the 1980s phenylethylamine (PEA) was discovered in chocolate. PEA acts as a CNS stimulant and increases the brain’s production of norepinephrine and dopamine-producing the euphoric effect often associated with a “runner’s high.” Cacao also helps to boost anandamide, a fatty acid neurotransmitter, which is also known as the “bliss molecule.” And cacao contains theobromine which has an effect like that of caffeine in the nervous system.
No wonder why so many of us love chocolate!
Recently, there have been studies that found that cocoa flavonoids including epicatechin have an anti-diabetic effect by enhancing insulin secretion, improving insulin sensitivity in peripheral tissues, exerting a lipid-lowering effect, and preventing the inflammatory and oxidative damages of the disease. (2)(3)(4)
Chocolate is often heavily sweetened as in See’s candy, but there are many chocolate bars that contain more cacao or cocoa and less sugar. Lately, I have purchased cacao powder and have been making a hot drink with coconut milk, monk sugar, and spices.
My daughter and I are going to start a new tradition this holiday season. We are not going to gift See’s candy, but instead, we are going to gift cacao.
1 TB Cacao powder has

Sugar Free Mexican Drinking Chocolate
Combine is a small saucepan and whisk until the consistency is smooth and silky. Pour into mugs. Give thanks. Enjoy.
References: