Ready to get certified?
Free CDCES Coach App

Subscribe
eNewsletter
Download
Free Med Pocket Cards
Question of the Week | Individual vs. Group DSMES

After the initial assessment JM is scheduled for an individual visit instead of a group DSMES class.
According to Medicare guidelines, which of the following would NOT justify providing individual DSMES instead of group DSMES?
- When scheduling, JM requested an individual appointment
- The referral for DSMES stated JM has a language barrier
- A group DSMES class is not available within the next 3 months
- JM was referred for training on starting insulin therapy
Prepare for the CDCES Exam
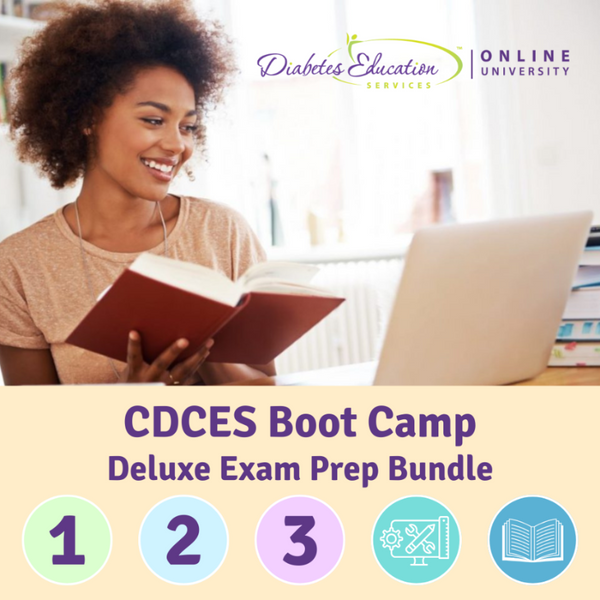
Course credits through AMA PRA Category 1 Credits™, ACPE, ANCC, and CDR!
Get exam-ready with confidence.
Our CDCES Boot Camp Online Prep Bundle is a comprehensive, high-impact program built specifically for healthcare professionals preparing for the Certified Diabetes Care and Education Specialist (CDCES) exam who want to level-up their clinical knowledge and skills.
✔ Learn at your pace with expert-led, exam-focused content
✔ Everything you need—organized, practical, and in one place
✔ Perfect for self-directed learners who want complete, person-centered content for clinical practice and exam prep.
✔ Build knowledge, sharpen test-taking skills, and prepare with confidence—on your schedule.
Focused. Flexible. Proven.
Basic & e-Deluxe CDCES Boot Camp Bundle Includes:
- Levels 1, 2, and 3 of our Online University
- 30+ expert-led courses
- 50 CE/CPEUs
- 400+ online practice questions
- Handouts, podcast, video and one year access—all in one streamlined platform.
Prepare for the BC-ADM Exam

Course credits through AMA PRA Category 1 Credits™, ACPE, ANCC, and CDR!
Get exam-ready with confidence.
Our comprehensive BC-ADM Online Study Programs are specifically designed for healthcare professionals who are studying for the Board Certified in Advanced Diabetes Management (BC-ADM) exam.
✔ Learn at your pace with expert-led, exam-focused content
✔ Everything you need—organized, practical, and in one place
✔ Perfect for self-directed learners who want complete, person-centered content for clinical practice and exam prep.
✔ Build knowledge, sharpen test-taking skills, and prepare with confidence—on your schedule.
Focused. Flexible. Proven.
Basic & e-Deluxe BC-ADM Boot Camp Bundle include:
- Levels 2, 3, and 4 of our Online University
- 30+ expert-led courses
- 50 CE/CPEUs
- 400+ online practice questions
- Handouts, podcast, video and one year access—all in one streamlined platform.
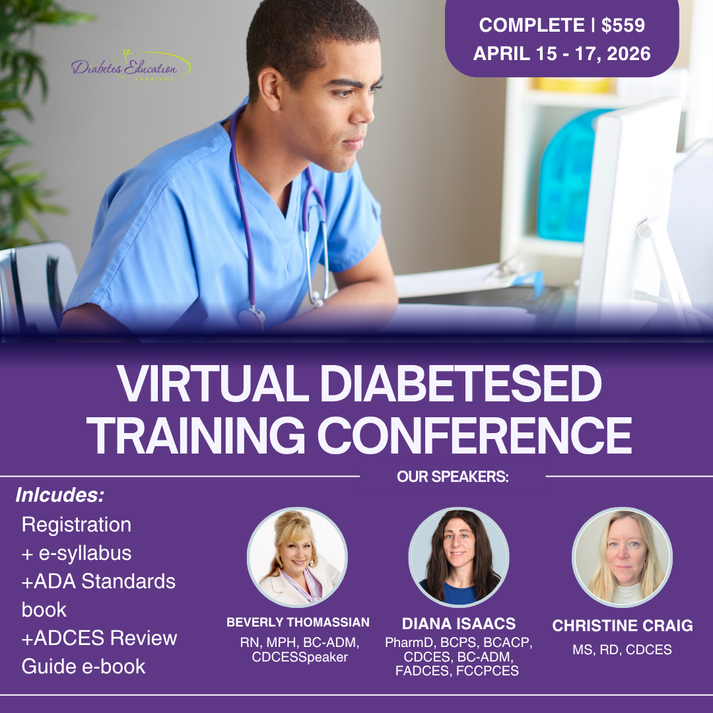
Virtual DiabetesEd Training Conference
April 15th-17th, 2026
Gain fresh insights, practical tools, and a deeper understanding of the latest in person-centered diabetes care. Our expert team brings the ADA Standards of Care to life—covering medications, behavior change, technology, and more!
Registration Options at a Glance
- 📜 Essentials: Includes registration and electronic syllabus.
- 🌟 Deluxe: Includes registration, electronic syllabus, and the ADA Standards Book for deeper study.
- 🏆 Complete: Best value! Includes everything listed above, plus the ADCES Review Guide of over 400 practice questions for exam prep.
Registration Fee includes
- 🎤 3 days of engaging, expert-led education
- 📘 100-page electronic syllabus +
- 🎓 12 FREE bonus online courses ($375 value) to boost your prep
Question of the Week | TIR (Time of Range) of 89% – What Is Your Concern?

JZ is proud of their Time of Range of 89%. You notice their time below range is 7%. JZ uses a rapid-acting insulin pen 4–6 times daily to keep glucose in target range and occasionally increases the glargine dose when evening glucose is elevated.
What is your primary concern?
- Is JZ consistently rotating injection sites to prevent lipohypertrophy?
- What is JZ’s rationale for adjusting the glargine dose?
- How is JZ feeling about their frequency of hypoglycemia?
- Does JZ adjust insulin for physical activity?
Learn More From The Experts:
Coach Beverly Thomassian, Dr. Diana Isaacs, & Christine Craig
Virtual DiabetesEd Training Conference
April 15th-17th, 2026
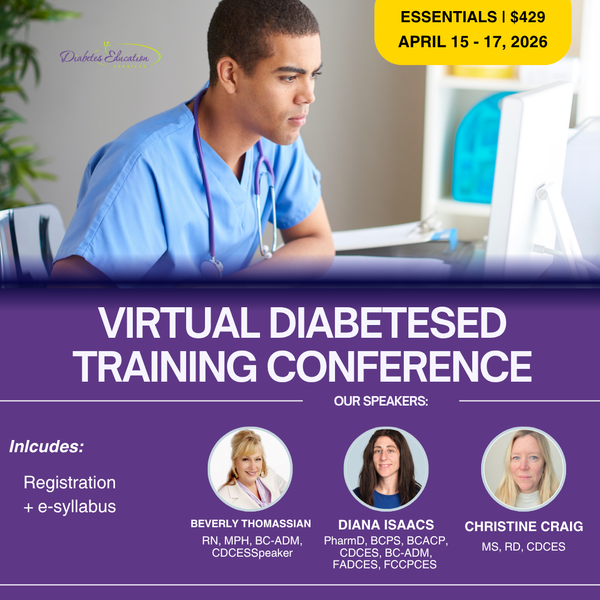
Gain fresh insights, practical tools, and a deeper understanding of the latest in person-centered diabetes care. Our expert team brings the ADA Standards of Care to life—covering medications, behavior change, technology, and more!
If you’re preparing for the CDCES or BC-ADM exam, this conference, paired with a handful of free bonus courses, serves as the ideal study companion! Plus, this content counts toward the ADA Standards requirements for CDCES Renewal.
With interactive co-teaching, we keep sessions engaging, relevant, and fun.
Let’s learn and grow together!
Course credits through AMA PRA Category 1 Credits™, ACPE, ANCC, and CDR!
Program Objectives:
Upon completion of this activity, participants should be able to:
- Describe the current ADA Standards for diagnosis, goals, and person-centered diabetes management across the lifespan.
- Demonstrate insulin pattern management and dosing strategies in clinical scenarios.
- Implement timely screening and risk reduction strategies for microvascular and cardiovascular complications.
- Incorporate behavior change techniques and medical nutrition therapy to support people with diabetes self-management and lifestyle adjustment.
Question of the Week | What Not to Say to Overwhelmed Individual

Maria, a 52‑year‑old woman with type 2 diabetes for 8 years, attends a follow‑up visit. Her A1C has risen from 7.8% to 9.2% over the past year. She reports feeling “overwhelmed” and says she didn’t want to start the medication her clinician recommended at the last visit. She explains, “I’m scared of side effects, and I feel like needing medication means I failed.”
Which of the following responses is the least appropriate (i.e., the WRONG thing to say) to Maria?
- “It sounds like you’re feeling overwhelmed. Can you tell me more about what worries you most about starting this medication?”
- “Many people feel this way. Let’s look at your options together so you can make a choice that works for you.”
- “I understand that this is challenging and overwhelming. However, if you don’t start this medication, you are choosing to risk complications like kidney disease or blindness.”
- “It’s completely understandable to have concerns. Would it help if we reviewed what the medication does, talk about the pro’s and the con’s, and about what alternatives exist?”
Learn More From The Experts:
William H. Polonsky, PhD, CDCES, and Susan Guzman, PhD
ENGAGING THE DISENGAGED | Live in San Diego at Marina Village
April 18th, 2026 from 9 AM to 4 PM PST!

In this course, William H. Polonsky, PhD, CDCES, and Susan Guzman, PhD, examine the powerful role of psychosocial factors in diabetes self-management. Through innovative strategies, participants will learn how to recognize and address common barriers to effective self-care and cardiometabolic medication initiation and maintenance, while fostering respectful, stigma-free clinical encounters.
Through a collaborative and person-centered approach, the course emphasizes communication strategies that enhance motivation, build confidence, and reinforce the value of self-management. Participants will develop skills in diabetes-focused action planning, addressing medication hesitancy, and providing ongoing support and resources to sustain behavior change over time. The goal is to help clinicians make diabetes care more doable, meaningful, and effective for people living with diabetes.
Question of the Week | Which Feature Most Strongly Supports a Diagnosis of HHS Rather Than DKA?

A 32-year-old with newly discovered diabetes is brought to the emergency department with polyuria and lethargy. They have been sleeping more than usual.
Initial labs show:
- Plasma glucose: 680 mg/dL
- Potassium 3.7 mEq/L
- Serum osmolality: 335 mOsm/kg
Based on the following labs, which feature most strongly supports a diagnosis of hyperosmolar hyperglycemic state (HHS) rather than diabetes ketoacidosis (DKA)?
- Markedly elevated plasma glucose
- Absence of significant metabolic acidosis
- Out of range potassium level
- Elevated effective serum osmolality
Learn More About DKA & HHS
With Level 2 | Hyperglycemic Crises (DKA, HHS & EDKA) & Our CDCES Boot Camp!
Question of the Week | Best Response for Facilitating Positive Health Behavior Change?

KC has type 2 diabetes, diagnosed 5 years ago. They report low physical activity, frequent sugar-sweetened beverage intake, and high stress related to work. Last A1c was 8.2%. KC reports previous advice to “exercise more and drink less soda,” but reports making minimal changes. They express interest in improving health but feels overwhelmed by where to start.
Which of the following responses best aligns with the 2026 ADA Standards of Care recommendations for facilitating positive health behavior change?
- Advise KC to stop sugary drinks and record physical activity minutes daily.
- Ask KC, “What makes improving your health important to you right now?”
- Focus the visit on intensifying glucose lowering medications first and revisit lifestyle changes at the next appointment.
- Recommend KC find social support for activity at the local gym and work with KC to set goals to avoid sugar-sweetened beverages.
Learn More About 2026 ADA Standards
With Our Upcoming Courses & Spreading the Love Sale!
Prepare for the CDCES Exam: Get Ready for Success!
Course credits through AMA PRA Category 1 Credits™, ACPE, ANCC, and CDR!
Get exam-ready with confidence.
Our CDCES Boot Camp Online Prep Bundle is a comprehensive, high-impact program built specifically for healthcare professionals preparing for the Certified Diabetes Care and Education Specialist (CDCES) exam who want to level-up their clinical knowledge and skills.
✔ Learn at your pace with expert-led, exam-focused content
✔ Everything you need—organized, practical, and in one place
✔ Perfect for self-directed learners who want complete, person-centered content for clinical practice and exam prep.
✔ Build knowledge, sharpen test-taking skills, and prepare with confidence—on your schedule.
Focused. Flexible. Proven.
Basic & e-Deluxe CDCES Boot Camp Bundle Includes:
- Levels 1, 2, and 3 of our Online University
- 30+ expert-led courses
- 50 CE/CPEUs
- 400+ online practice questions
- Handouts, podcast, video and one year access—all in one streamlined platform.
Spreading the Love Sale
Save 15% on Certification Boot Camps & Trainings
Use the Code "LOVE15" for 15% Off at Checkout!
CDCES Boot Camp | 50+ CEs
Starting: $449 | Starting Sale Price: $381.65
BC-ADM Boot Camp | 50+ CEs
Starting: $459 | Starting Sale Price: $390.15
Dual-Cert Boot Camp | 60+ CEs
Starting: $519 | Starting Sale Price: $441.15
Virtual Training | 30+ CEs
Starting: $429 | Starting Sale Price: $364.65
Sale Ends on February 16th, 2026!

Question of the Week | What Does J.C.’s Family History & Lab Work Reveal?

J.C. is a ten-year-old female with a family history of type 1 diabetes. Her 7-year-old brother was diagnosed with type 1 diabetes two years ago. J.C. has no complaints and reports feeling well. She enjoys playing sports, including basketball and soccer. Her current BMI is 22.1 (93rd percentile for age). She denies any polydipsia, polyuria, or polyphagia. Her lab work demonstrates a fasting blood sugar of 71 mg/dL, an A1c of 5.0%, normal kidney function, and normal electrolytes. Her diabetes autoantibody panel shows positive glutamic acid decarboxylase (GAD) and islet antigen 2 (IA-2) antibodies, negative zinc transporter 8 (ZnT8) antibodies, and negative insulin antibodies.
What does her lab work reveal?
- Stage 1 Type 1 diabetes
- Stage 2 Type 1 diabetes
- Stage 3 Type 1 diabetes
- Type 2 diabetes
Learn More About Type 1 Staging & Stds
With Our CDCES Boot Camp Bundle | Includes Level(s) 1-3!
Welcome to our selection of comprehensive CDCES Boot Camp Online Prep Bundles that are specifically designed for healthcare professionals who are studying for the Certified Diabetes Care and Education Specialist (CDCES) exam.
Course credits through AMA PRA Category 1 Credits™, ACPE, ANCC, and CDR!
We offer a selection of prep bundles to meet everyone’s needs! See the descriptions below to review what is included in each option.
CDCES Boot Camp | Basic Exam Prep Bundle: This option is perfect for someone who wants just the Online Courses and materials all in one place, our Online University. This bundle includes Levels 1, 2, and 3 & Toolkits which equates to over 30 courses, 50 CEs/CPEUs, and 400+ online practice questions.
CDCES Boot Camp | e-Deluxe Exam Prep Bundle: This bundle has all of the courses from the Basic Bundle, along with the ADCES Certification Review Guide Practice Questions e-book with 400+ practice questions.
Question of the Week | What to Assess When Looking for PAD?

Peripheral Artery Disease (PAD) is significantly underdiagnosed. While PAD affects around 8.5 million Americans and prevalence rises with age (up to 20% over 60), only 10-20% are clinically diagnosed, highlighting a major gap in awareness and screening.
According to the ADA Standards, what needs to be included in the initial screening for PAD?
- History of leg fatigue and calf pain when walking.
- Lower extremity pain that is worse at night and restless legs.
- Leg cramps coupled and frequent unexplained bruising.
- Onychomycosis and unusual callus formation.
Level 2 | Standard 12: Lower Extremity Assessment
Join us live on March 12th, 2026 at 11:30 AM PST!
Question of the Week | CS’s A1C Climbs After Experiencing Distress

CS is a 42-year-old with type 1 diabetes for just over 18 years. In the past year, their A1C changed from 7.4% to 9.1%, and weight increased by 20 pounds. Review of CGM data suggests missed insulin boluses more than 7 times per week, and discussion with CS reveals missed clinic visits due to feeling “burned out”. They score in the moderate range on the Diabetes Distress Scale.
Based on the ADA 2026 Standards of Care, which of the following is the most appropriate next step?
- Partner with CS to reduce missed boluses and reassess in 3 months.
- Simplify regimen to support current state of diabetes distress.
- Refer to a qualified behavioral health professional for evaluation and treatment.
- Recommend referral to MNT for a structured weight-loss program.
Level 2 | ADA Standards of Care Complete Review
2026 Recording Available On-Demand
Level 2 | Improving Care and Promoting Health
Join us live on February 10th, 2026 at 11:30 AM PST!