
Ready to get certified?
Free CDCES Coach App

Subscribe
eNewsletter
Download
Free Med Pocket Cards
Rationale of the Week | RD feels overwhelmed by all this sensor data. Best action?
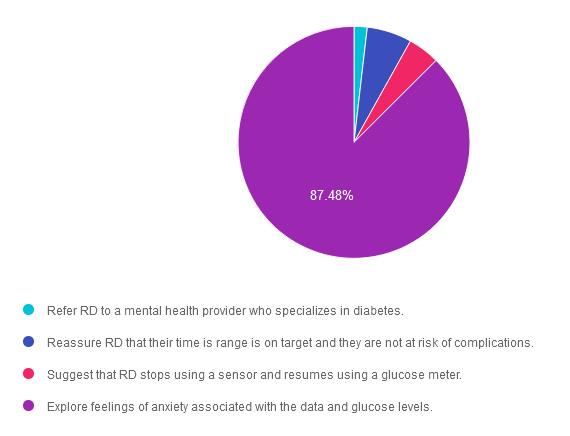
For last week’s practice question, we quizzed participants on actions to help address stress during data monitoring. 87% of respondents chose the best answer. We want to clarify and share this important information, so you can pass it on to people living with diabetes and your colleagues, plus prepare for exam success!
Before we start though, if you don’t want any spoilers and haven’t tried the question yet, you can answer it below: Answer Question

Question: RD is 82 years old, on basal insulin with bolus insulin at breakfast and dinner if need. RD just started using a sensor to track their daily blood sugars. After using the sensor for a few weeks, they share that they are feeling anxious and don’t know what to do with all this information. They even took extra bolus insulin yesterday to try and get blood sugars down. RD’s time in range is over 70%.
Which of the following is the most appropriate intervention?
Answer Choices:
- Refer RD to a mental health provider who specializes in diabetes.
- Reassure RD that their time is range is on target and they are not at risk of complications.
- Suggest that RD stops using a sensor and resumes using a glucose meter.
- Explore feelings of anxiety associated with the data and glucose levels.
Getting to the Best Answer
Answer 1 is incorrect. 1.83% chose this answer. “Refer RD to a mental health provider who specializes in diabetes.” RD is having an understandable response to the abundance of info provided by their new CGM and is experiencing diabetes distress. Based on the information provided, their anxiety doesn’t warrant a referral to a mental health specialist.
Answer 2 is incorrect. 6.26% of you chose this answer. “Reassure RD that their time is range is on target and they are not at risk of complications.” Although it is important to reassure RD that they have a time in range greater than 70%, it is important to acknowledge their feelings and explore strategies to address to diabetes distress.
Answer 3 is incorrect. About 4.43% of respondents chose this. “Suggest that RD stops using a sensor and resumes using a glucose meter.” Since RD has only been using the sensor for a few weeks, we wouldn’t want to suggest giving it up just yet. In addition, we want to learn more about what RD is experiencing and the issues that are increasing their anxiety and help with problem solving.
Finally, Answer 4 is correct. 87.48% chose this answer. “Explore feelings of anxiety associated with the data and glucose levels.” YES. GREAT JOB! This is the best person-centered answer that encourages RD to share their feelings so we can help with problem solving and evaluate the best approach for this individual.
We hope you appreciate this week’s rationale! Thank you so much for taking the time to answer our Question of the Week and participate in this fun learning activity!
Want to learn more about this question?
Unlock insights for managing diabetes distress with the experts!
Join us live on June 17 & 24, 2024 for our
ReVive 5 Diabetes Training Program:
The 2024 ADA Standards of Care now recommends annual screening for diabetes distress. If you are wondering how to screen for distress and tailor education based on the results, we encourage you to join this unique training program.
This two-session training provides the essential steps to address diabetes distress combined with an innovative approach to helping people make sense of their glucose data.
The first session is team-taught by experts in the field of diabetes distress and effective communication approaches. Dr. Larry Fisher kicks off the program by describing the difference between depression and distress and interpreting Diabetes Distress screening results. Dr. Susan Guzman uses a case study approach and step-by-step communication strategies to address responses from the Diabetes Distress screening tool. This session includes an abundance of evidence-based approaches that you can apply in your clinical setting.
Coach Beverly leads the second session. During this three-hour program, Beverly describes insulin dosing strategies, meter and sensor data interpretation, and common issues encountered by people using diabetes technology. Case studies include tools to help individuals discover what changes are needed to get glucose to target, coupled with the communication skills discussed in the first session. In conclusion, the team of instructors review a case study that pulls together all the ReVive 5 elements.
“ReVive 5” breathes new life into our relationship with diabetes, bringing a fresh perspective to both the person with diabetes and the provider.
Can’t join live? That’s okay. Your registration guarantees you access to the recorded version of the series, along with podcasts and resources for one full year.
Accredited Training Program:
- 15+ CEs – Includes the 7-hour ReVive 5 Training Program, Certificate, and 5 FREE bonus courses to supplement content.
- A comprehensive set of assessment tools, educational materials, log sheets, and resources.
Join us to gain the confidence and learn the skills needed to support people with diabetes to move forward in their self-management and discover the expert within.
Team of Experts:
ReVive 5 is taught by a team of 3 Interdisciplinary Experts:
- Lawrence Fisher, Ph.D., ABPP, Professor Emeritus, UCSF
- Susan Guzman, PhD
- Beverly Thomassian, RN, MPH, CDCES, BC-ADM
Speakers Interviews – Learn more about the ReVive 5 Team
Sign up for Diabetes Blog Bytes – we post weekly Blog Bytes that are informative and FREE! Every week we post one exam practice Question of the Week and Rationale of the Week. Sign up below!
Recent Blog Bytes
- February 2026 eNews
- Rationale of the Week | Best Response for Facilitating Positive Health Behavior Change?
- Question of the Week | Which Feature Most Strongly Supports a Diagnosis of HHS Rather Than DKA?
- Rationale of the Week | What Does J.C.’s Family History & Lab Work Reveal?
- Red Flags for Low Digital Literacy in Diabetes Care
Accreditation: Diabetes Education Services is an approved provider by the California Board of Registered Nursing, Provider 12640, and our CPEU courses have received Prior Approval* from the Commission of Dietetic Registration (CDR), Provider DI002. Since our CPEU courses received Prior approval* from the CDR, these CPEU courses satisfy the CE requirements for the CDCES /BC-ADM regardless of your profession!
The use of DES products does not guarantee the successful passage of the certification exam. CBDCE and ADCES do not endorse any preparatory or review materials for the CDCES or BC-ADM exams, except for those published by CBDCE & ADCES.
Rationale of the Week | Euglycemic DKA – What is Best Intervention?
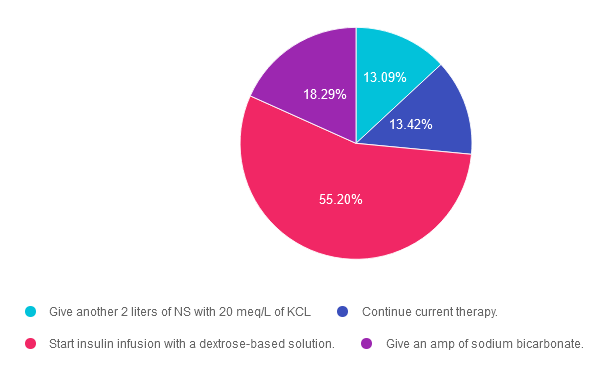
For last week’s practice question, we quizzed participants on what is the best intervention for euglycemic DKA. 55% of respondents chose the best answer. We want to clarify and share this important information, so you can pass it on to people living with diabetes and your colleagues, plus prepare for exam success!
Before we start though, if you don’t want any spoilers and haven’t tried the question yet, you can answer it below: Answer Question

Question: KT is a 54-year-old, who presents to the emergency room with nausea and vomiting. KT weighs 58kg, has been feeling very tired and has diabetes and hypertension.
Meds include: losartan, metformin, and empagliflozin.
Labs: Na 140, K 4.0, Chloride 99, Bicarb 15, Glucose 189, Anion Gap 26, pH 7.1 and positive urine ketones
After infusing 2 liters of normal saline, what would be the best intervention for KT?
Answer Choices:
- Give another 2 liters of NS with 20 meq/L of KCL
- Continue current therapy.
- Start insulin infusion with a dextrose-based solution.
- Give an amp of sodium bicarbonate.
Getting to the Best Answer
Answer 1 is incorrect. 13% chose this answer. “Give another 2 liters of NS with 20 meq/L of KCL.” Since KT has already received 2 liters of normal saline for fluid resuscitation, the next step is to provide a solution with glucose, and possibly potassium depending on KT’s electrolyte levels. Even with euglycemic DKA, KT has depleted their glycogen stores and the cells are in desperate need of glucose for two reasons; to stop burning fat for fuel and to replete glycogen stores.
Answer 2 is incorrect. 13.42% of you chose this answer. “Continue current therapy.” While this answer is tempting, it does not provide a clear plan of action for KT. The only therapy this is currently being provided is an IV of normal saline. Even though KT’s blood glucose is less than 200mg/dL, in order to stop ketosis, we need to start IV insulin along with 5-10% dextrose to preserve blood glucose and replace glycogen stores.
Answer 3 is correct. About 55.20% of respondents chose this. “Start insulin infusion with a dextrose-based solution.” YES! This is the best answer. The next step is to provide an IV solution with 5-10% glucose, and possibly potassium depending on KT’s electrolyte levels. Even with euglycemic DKA, KT has depleted their glycogen stores and the cells are in desperate need of glucose for two reasons; to stop burning fat for fuel and to replete glycogen stores. In addition, in order to stop ketosis, we need to start IV insulin at a few units an hour!
Finally, Answer 4 is incorrect. 18.29% chose this answer. “Give an amp of sodium bicarbonate.” Since KT is in acidosis, this is a tempting answer. However, the acidosis will usually be corrected with administration of IV fluids and insulin. If not, and the pH is still below 7.0, bicarb administration may be considered.
We hope you appreciate this week’s rationale! Thank you so much for taking the time to answer our Question of the Week and participate in this fun learning activity!
Want to learn more about this question?
Keynote Presentation on DKA & Euglycemic DKA at
16th Annual Conference
Expanding the Universe of Diabetes Care hosted by CA ADCES
May 3-4th at Universal City, CA

Beverly will be speaking on DKA and EDKA on Saturday – May 4, 2024 at 11:30 am
Below is Saturday’s schedule of topics and flyer for more information. We hope to see you there!
>>Register for the Conference
>>Flyer for Event
- Discover the secrets to a successful and sustainable Diabetes Education Program – Tony Song, MBA
- Exercise Success Part 3 & 4 – Jacqueline Thompson, MS, RD, CDCES, MES
- Dynamic Duo: Registered Dietitian & Pharmacist Co-Appointments in Diabetes Care – Christal Pham, PharmD, APh, CDCES, Melanie Barbee, MS, RDN, CDCES, DipACLM
- Advocacy Update: Breakdown the Barriers to Evidence-Based Diabetes Care – Teresa Martin MS RDN CDCES LD
- New criteria and treatment guidelines for DKA, Euglycemic DKA, and HHS – Beverly Thomassian, RN, MPH, CDCES, BC-ADM
- Exercise Success Part 4 – Jacqueline Thompson, MS, RD, CDCES, MES
- Diabetes Technology: Understanding the Differences in the Latest CGMs and Pumps – David Ahn, MD
Sign up for Diabetes Blog Bytes – we post weekly Blog Bytes that are informative and FREE! Every week we post one exam practice Question of the Week and Rationale of the Week. Sign up below!
Recent Blog Bytes
- February 2026 eNews
- Rationale of the Week | Best Response for Facilitating Positive Health Behavior Change?
- Question of the Week | Which Feature Most Strongly Supports a Diagnosis of HHS Rather Than DKA?
- Rationale of the Week | What Does J.C.’s Family History & Lab Work Reveal?
- Red Flags for Low Digital Literacy in Diabetes Care
Accreditation: Diabetes Education Services is an approved provider by the California Board of Registered Nursing, Provider 12640, and our CPEU courses have received Prior Approval* from the Commission of Dietetic Registration (CDR), Provider DI002. Since our CPEU courses received Prior approval* from the CDR, these CPEU courses satisfy the CE requirements for the CDCES /BC-ADM regardless of your profession!
The use of DES products does not guarantee the successful passage of the certification exam. CBDCE and ADCES do not endorse any preparatory or review materials for the CDCES or BC-ADM exams, except for those published by CBDCE & ADCES.
Rationale of the Week | ADA Standards for Gestational Diabetes
For last week’s practice question, we quizzed participants on ADA Standards for gestational diabetes. [%] of respondents chose the best answer. We want to clarify and share this important information, so you can pass it on to people living with diabetes and your colleagues, plus prepare for exam success!
Before we start though, if you don’t want any spoilers and haven’t tried the question yet, you can answer it below: Answer Question

Question: LS has type 1 diabetes and is here for the first visit after confirmation of pregnancy. LS has been using non-adjunctive continuous glucose monitoring (CGM) along with insulin pump therapy to manage diabetes. Previous visits have focused on preconception counseling and last A1c was 6.4%.
According to the 2024 ADA Standards of Care, what do we recommend regarding glucose monitoring during pregnancy?
Answer Choices:
- Recommend continued CGM use with the addition of post-prandial glucose monitoring.
- LS can continue use of non-adjunctive CGM device approved for use during pregnancy.
- Recommend continued CGM with the addition of scheduled blood glucose monitoring.
- Recommend LS move to blood glucose monitoring and check fasting, pre-prandial and post-prandial glucose values.

Getting to the Best Answer
Answer 1 is incorrect. [%] chose this answer. “Recommend continued CGM use with the addition of post-prandial glucose monitoring.” Choice A is not the best answer. The 2024 ADA Standards of Care do recommend CGM use for individuals with type 1 diabetes during pregnancy but simply monitoring post-prandial glucose is insufficient. Keep reading below.
Answer 2 is incorrect. [%] of you chose this answer. “LS can continue use of non-adjunctive CGM device approved for use during pregnancy.” Choice B is not correct. We can continue use of CGM devices during pregnancy, but blood glucose monitoring is recommended in addition to CGM.
Answer 3 is correct. About [%] of respondents chose this. “Recommend continued CGM with the addition of scheduled blood glucose monitoring.” Answer C is correct. The 2024 Standards of Care recommends CGM for individuals with type 1 diabetes during pregnancy but also recommends that it not replace pre-prandial and post-prandial blood glucose monitoring. Fasting, pre-prandial and post-prandial blood glucose monitoring is recommended for individuals with diabetes in pregnancy.
Finally, Answer 4 is incorrect. [%] chose this answer. “Recommend LS move to blood glucose monitoring and check fasting, pre-prandial and post-prandial glucose values.” Response D is not the best answer. We will recommend LS add blood glucose monitoring, but LS does not need to transition off CGM therapy.
We hope you appreciate this week’s rationale! Thank you so much for taking the time to answer our Question of the Week and participate in this fun learning activity!
Want to learn more about this question?
Join us live on June 11th at 11:30 am PST for our
Pregnancy & Diabetes
Level 2 Standards of Care Intensive
Pregnancy with diabetes is confronted with a variety of issues that require special attention, education, & understanding. This course reviews those special needs while focusing on Gestational Diabetes & Pre-Existing Diabetes. Included are the most recent diagnostic criteria, management goals, & prevention of complications during pregnancy. This is a helpful review for Certification Exams & those who want more information on people who are pregnant & live with diabetes.
Objectives:
- List three issues that affect pregnancy with diabetes.
- Describe the unique attributes of pre-existing diabetes in pregnancy & gestational diabetes.
- State the diagnostic criteria & management goals for gestational diabetes.
- Potential short-term & long-term complications of fetal exposure to hypoglycemia.
- Prevention measures to keep mother & baby healthy.
Learning Outcome:
Participants will gain knowledge of special considerations, individualized goals, and standards for people experiencing diabetes during pregnancy to improve outcomes.
Target Audience:
This course is a knowledge-based activity designed for individuals or groups of diabetes professionals, including RNs, RDs/RDNs, Pharmacists, Nurse Practitioners, Clinical Nurse Specialists, Physician Assistants, and other healthcare providers interested in staying up to date on current practices of care for people with prediabetes, diabetes, and other related conditions. The practice areas for RDs/RDNs for CDR reporting are healthcare, preventative care, wellness, and, lifestyle along with, education and research.
CDR Performance Indicators:
- 9.6.7
- 9.6.8
- 10.3.1
Instructor: Beverly Thomassian RN, MPH, CDCES, BC-ADM is a working diabetes specialist and a nationally recognized diabetes expert.
Sign up for Diabetes Blog Bytes – we post weekly Blog Bytes that are informative and FREE! Every week we post one exam practice Question of the Week and Rationale of the Week. Sign up below!
Recent Blog Bytes
- February 2026 eNews
- Rationale of the Week | Best Response for Facilitating Positive Health Behavior Change?
- Question of the Week | Which Feature Most Strongly Supports a Diagnosis of HHS Rather Than DKA?
- Rationale of the Week | What Does J.C.’s Family History & Lab Work Reveal?
- Red Flags for Low Digital Literacy in Diabetes Care
Accreditation: Diabetes Education Services is an approved provider by the California Board of Registered Nursing, Provider 12640, and our CPEU courses have received Prior Approval* from the Commission of Dietetic Registration (CDR), Provider DI002. Since our CPEU courses received Prior approval* from the CDR, these CPEU courses satisfy the CE requirements for the CDCES /BC-ADM regardless of your profession!
The use of DES products does not guarantee the successful passage of the certification exam. CBDCE and ADCES do not endorse any preparatory or review materials for the CDCES or BC-ADM exams, except for those published by CBDCE & ADCES.
Rationale of the Week | JR is out of lispro (Humalog) insulin and is panicking.
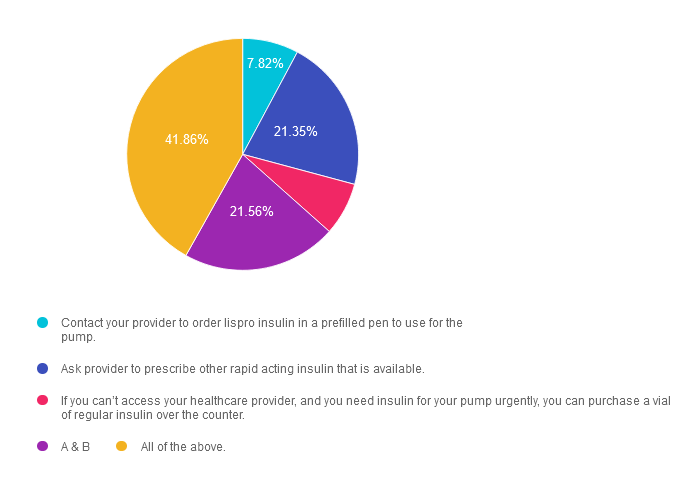
For last week’s practice question, we quizzed participants on JR is out of lispro (Humalog) insulin and is panicking. 42% of respondents chose the best answer. We want to clarify and share this important information, so you can pass it on to people living with diabetes and your colleagues, plus prepare for exam success!
Before we start though, if you don’t want any spoilers and haven’t tried the question yet, you can answer it below: Answer Question.

Question: JR is a 19-year-old, living with type 1 diabetes. They use lispro (Humalog) insulin in their insulin pump. They just heard from their pharmacy that lispro is in short supply and they don’t know when they will be getting in the next shipment. JR tells you they are almost done with their current lispro vial and is panicking, asking what they should do.
Answer Choices:
- Contact your provider to order lispro insulin in a prefilled pen to use for the pump.
- Ask provider to prescribe other rapid acting insulin that is available.
- If you can’t access your healthcare provider, and you need insulin for your pump urgently, you can purchase a vial of regular insulin over the counter.
- A & B
- All of the above.
Getting to the Best Answer
Answer 1 is incorrect. 7.8% chose this answer. “Contact your provider to order lispro insulin in a prefilled pen to use for the pump.” This answer is correct, but it is not the BEST answer. Since insulin pens are more readily available and it is the same insulin formulation and concentration, JR can use the insulin from a lispro insulin pen in their pump. However, there is a better answer, so, keep reading.
Answer 2 is incorrect. 21.35% of you chose this answer. “Ask provider to prescribe other rapid acting insulin that is available.” This answer is correct, but it is not the BEST answer. There are other rapid acting insulins such as NovoLog (insulin aspart) or the biosimilar insulin Admelog (insulin lispro injection) made by other manufacturers that are more readily available with the same insulin concentration. However, there is a better answer, so, keep reading.
Answer 3 is incorrect. About 7.4% of respondents chose this. “If you can’t access your healthcare provider, and you need insulin for your pump urgently, you can purchase a vial of regular insulin over the counter.” This answer is correct, but it is not the BEST answer. Regular insulin is available for purchase over-the-counter without the need for a prescription and is FDA approved for used in an insulin pump. However, there is a better answer, so, keep reading.
Answer 4 is incorrect. 21.6% chose this answer. “A & B”
Finally, Answer 5 is correct. 41.9% chose this answer. “All of the above.” YES, this is the best answer, all 3 options are correct. Of course, we encourage individuals to consult with their healthcare provider, since everyone responds differently to switching insulins. We wanted to raise awareness with this question, since many individuals with diabetes who use insulin lispro and Humalog vials for their insulin pumps have encountered shortages. We can reassure them that there are several options to get them by until lispro and Humalog insulin are back on the shelf. For more info, you can download our Insulin PocketCards.
We hope you appreciate this week’s rationale! Thank you so much for taking the time to answer our Question of the Week and participate in this important learning activity!
Want to Learn more about recognizing and addressing Diabetes Distress?
Join us live on May 22nd & May 29th, 2024 for our
ReViVE 5 Diabetes Training Program:
Unlocking Hidden Barriers to Diabetes Management
“ReVive 5” breathes new life into our relationship with diabetes, bringing a fresh perspective to both the person with diabetes and the provider.
The ReVive 5 program is built on sound research from the Embark Trial and will revolutionize your approach to diabetes self-management education.
We have reassembled the Embark training team and created a resource binder of fantastic tools that we are excited to share with you in our ReVive 5 Diabetes Training Program. You are invited to join us to learn a step-wise, proven approach to addressing hidden barriers to diabetes self-management and glucose management.
You don’t need to be mental health expert or diabetes technology wiz to join this training or to integrate these new strategies into your daily practice.
ReVive 5 uses an integrated, evidence-based approach that provides health care professionals with a realistic 5-step approach to addressing the whole person, starting with emotional distress and incorporating a unique, but integrated approach to problem-solving glucose management difficulties.
Intended Audience: This library of critical information is designed for individuals or groups of diabetes specialists, including RNs, RDs, Pharmacists, Nurse Practitioners, Clinical Nurse Specialists, Physician Assistants, and other health care providers interested in staying up to date on current practices of care for people with diabetes and preparing for the CDCES or BC-ADM Certification Exams.
Can’t join live? That’s okay. Your registration guarantees you access to the recorded version of the series, along with podcasts and resources for one full year.
Accredited Training Program:
- 15+ CEs – Includes the 7-hour ReVive 5 Training Program, Certificate, and 5 FREE bonus courses to supplement content.
- A comprehensive set of assessment tools, educational materials, log sheets, and resources.
Join us to gain the confidence and learn the skills needed to support people with diabetes to move forward in their self-management and discover the expert within.
Team of Experts:
ReVive 5 is taught by a team of 3 Interdisciplinary Experts:
- Lawrence Fisher, Ph.D., ABPP, Professor Emeritus, UCSF
- Susan Guzman, PhD
- Beverly Thomassian, RN, MPH, CDCES, BC-ADM
Speakers Interviews – Learn more about the ReVive 5 Team
Sign up for Diabetes Blog Bytes – we post weekly Blog Bytes that are informative and FREE! Every week we post one exam practice Question of the Week and Rationale of the Week. Sign up below!
Recent Blog Bytes
- February 2026 eNews
- Rationale of the Week | Best Response for Facilitating Positive Health Behavior Change?
- Question of the Week | Which Feature Most Strongly Supports a Diagnosis of HHS Rather Than DKA?
- Rationale of the Week | What Does J.C.’s Family History & Lab Work Reveal?
- Red Flags for Low Digital Literacy in Diabetes Care
Accreditation: Diabetes Education Services is an approved provider by the California Board of Registered Nursing, Provider 12640, and our CPEU courses have received Prior Approval* from the Commission of Dietetic Registration (CDR), Provider DI002. Since our CPEU courses received Prior approval* from the CDR, these CPEU courses satisfy the CE requirements for the CDCES /BC-ADM regardless of your profession!
The use of DES products does not guarantee the successful passage of the certification exam. CBDCE and ADCES do not endorse any preparatory or review materials for the CDCES or BC-ADM exams, except for those published by CBDCE & ADCES.
Rationale of the Week | Why are CGM readings higher than BG readings?
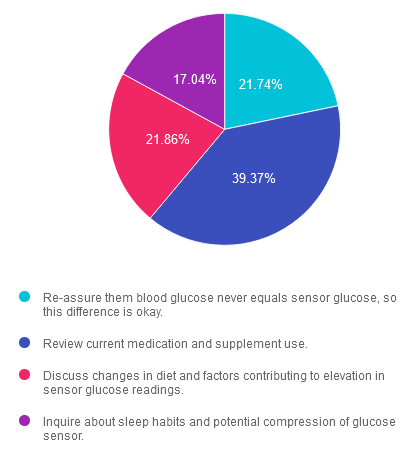
For last week’s practice question, we quizzed participants on why CGM readings are higher than BG readings. 39% of respondents chose the best answer. We want to clarify and share this important information, so you can pass it on to people living with diabetes and your colleagues, plus prepare for exam success!
Before we start though, if you don’t want any spoilers and haven’t tried the question yet, you can answer it below: Answer Question

Question: KS has type 1 diabetes, takes degludec and lispro for their diabetes medications and was recently prescribed CGM therapy to support glucose monitoring. At their visit they report sensor readings have been consistently higher than blood glucose readings.
What would be an important follow-up question to evaluate the potential cause of this difference?
Answer Choices:
- Re-assure them blood glucose never equals sensor glucose, so this difference is okay.
- Review current medication and supplement use.
- Discuss changes in diet and factors contributing to elevation in sensor glucose readings.
- Inquire about sleep habits and potential compression of glucose sensor
Getting to the Best Answer
Answer 1 is incorrect. 21.74% chose this answer. “Re-assure them blood glucose never equals sensor glucose, so this difference is okay.” This answer is incorrect. Although it is true that sensor glucose does not equal blood glucose, there may be other factors contributing to consistent elevation in glucose trends. We would want to probe into other potential considerations before jumping to the conclusion that it is only the difference in measurement.
Answer 2 is correct. 39.37% of you chose this answer. “Review current medication and supplement use.” This answer is correct. Interfering substances such as acetaminophen and ascorbic acid (vitamin C) can contribute to higher glucose readings than actual glucose. The interfering substance depends upon the CGM manufacturer. The 2024 ADA Standards of Care reports the importance of reviewing medications and supplements used by persons with diabetes to identify possible interfering substances. They also recommend blood glucose monitoring if there is a concern of inaccurate data. Visit Section 7 of the 2024 Standards of Care to review the table of CGM manufacturers and potential interring substances.
Answer 3 is incorrect. About 21.86% of respondents chose this. “Discuss changes in diet and factors contributing to elevation in sensor glucose readings.” This answer is incorrect. Although sensor glucose and blood glucose values are more likely to significantly differ after a meal, KS reports consistent elevation in sensor glucose values. Diet factors contributing to elevated sensor glucose readings would likely contribute to elevated blood glucose readings too; we may just see a delay. Diet factors alone would not explain the consistent difference in elevation.
Finally, Answer 4 is incorrect. 17.04% chose this answer. “Inquire about sleep habits and potential compression of glucose sensor.” This answer is incorrect. Compression of the sensor during sleep can contribute to false sensor glucose readings, but we most often see sudden decreases (low) in glucose values. This is suspected to be due to local changes in blood flow/concentration of the interstitial glucose caused by direct pressure on the sensor. Screening for compression lows is important when reviewing CGM data but does not provide the best answer for consistently elevated glucose trends.
We hope you appreciate this week’s rationale! Thank you so much for taking the time to answer our Question of the Week and participate in this fun learning activity!
Want to learn more about this question?
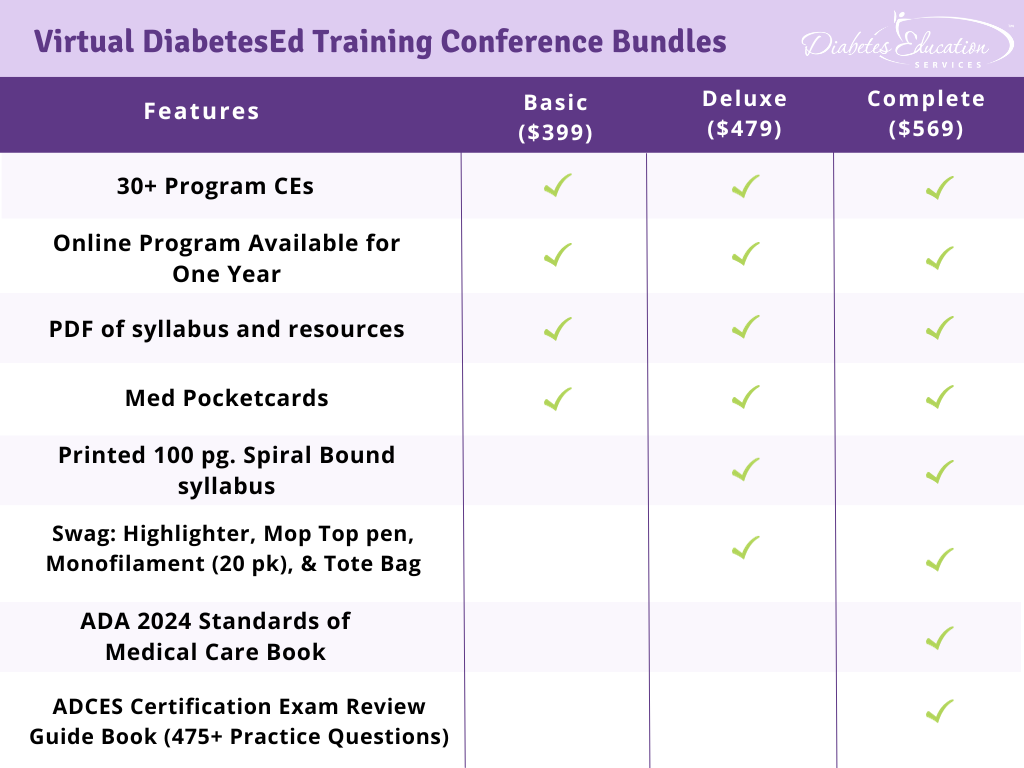
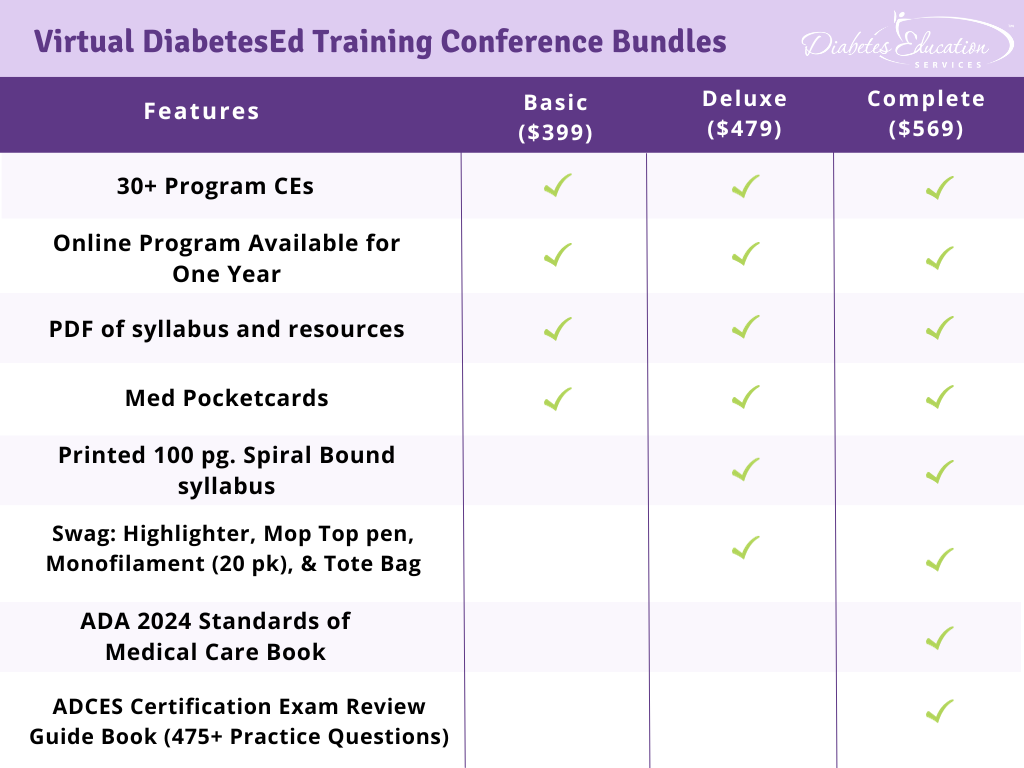
Virtual DiabetesEd Training Conference – Join us Live on April 17th – 19th 2024 at 11:30 AM PST

Join Coach Beverly and Team for two and a half days of knowledge-sharing, fun, and “aha” moments for our Virtual DiabetesEd Training Conference April 17th – 19th, 2024.
Attendees will leave this conference with new tools and a refreshed understanding of the latest advances in person-centered diabetes care. Our team highlights the ADA Standards of Care, medications, behavior change, technology, medical nutrition therapy, and more!
Our instructors co-teach the content to keep things fresh and lively.
Friend Discount: 3 or more only $449 per person. Email us at [email protected] with the name and email of each registrant to get the discount!
Program Details
- Dates: April 17-19th, 2024
- Registration Fee: $399-$569 (see more about reg. options below)
- Friend Discount: For 3 or more people, each person saves $50 off their registration. Email us at [email protected] with the name and email of each registrant to get the discount!
- CEs: 30+ CEs | 18 units for Virtual Conference plus 10+ Bonus CEs. CEs can be applied toward CDCES’s initial application or renewal.
- Speakers: View Conference Faculty
Registration Options
Sign up for Diabetes Blog Bytes – we post weekly Blog Bytes that are informative and FREE! Every week we post one exam practice Question of the Week and Rationale of the Week. Sign up below!
Recent Blog Bytes
- February 2026 eNews
- Rationale of the Week | Best Response for Facilitating Positive Health Behavior Change?
- Question of the Week | Which Feature Most Strongly Supports a Diagnosis of HHS Rather Than DKA?
- Rationale of the Week | What Does J.C.’s Family History & Lab Work Reveal?
- Red Flags for Low Digital Literacy in Diabetes Care
Accreditation: Diabetes Education Services is an approved provider by the California Board of Registered Nursing, Provider 12640, and our CPEU courses have received Prior Approval* from the Commission of Dietetic Registration (CDR), Provider DI002. Since our CPEU courses received Prior approval* from the CDR, these CPEU courses satisfy the CE requirements for the CDCES /BC-ADM regardless of your profession!
The use of DES products does not guarantee the successful passage of the certification exam. CBDCE and ADCES do not endorse any preparatory or review materials for the CDCES or BC-ADM exams, except for those published by CBDCE & ADCES.
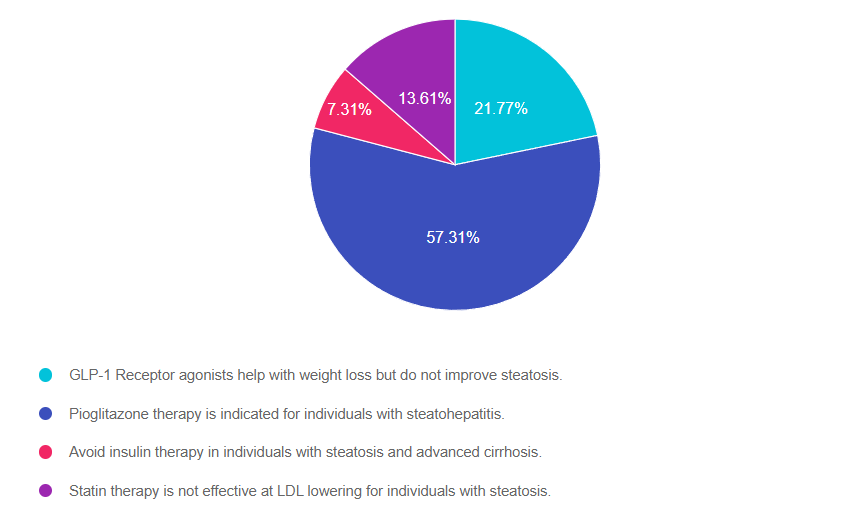
Rationale of the Week | Which statement is accurate regarding treatment of steatosis?
For last week’s practice question, we quizzed participants on steatosis treatment according to ADA. 57% of respondents chose the best answer. We want to clarify and share this important information, so you can pass it on to people living with diabetes and your colleagues, plus prepare for exam success!
Before we start though, if you don’t want any spoilers and haven’t tried the question yet, you can answer it below: Answer Question

Question: Up to 70% of people with diabetes have steatosis. Those at higher risk of moving to steatohepatitis include individuals with prediabetes and diabetes who also have cardiometabolic risk factors.
According to ADA Standards, which of the following is an accurate statement regarding treatment of liver disease in diabetes?
Answer Choices:
- GLP-1 Receptor agonists help with weight loss but do not improve steatosis.
- Pioglitazone therapy is indicated for individuals with steatohepatitis.
- Avoid insulin therapy in individuals with steatosis and advanced cirrhosis.
- Statin therapy is not effective at LDL lowering for individuals with steatosis.
Common Native Plants in the U.S.
Getting to the Best Answer
Answer 1 is incorrect. 21.77% chose this answer. “GLP-1 Receptor agonists help with weight loss but do not improve steatosis.” This juicy answer is tempting, but it is not the best answer. GLP-! RA’s, lower blood glucose levels and they also promote significant weight loss. This results in less glucose toxicity and a decrease in hepatic fat storage. Plus, they decrease the risk of cardiovascular disease which is co-associated with steatosis. See our Meds for Liver Disease Blog for more info.
Answer 2 is correct. 57.31% of you chose this answer. “Pioglitazone therapy is indicated for individuals with steatohepatitis.” Yes, this is the best answer. Pioglitazone (Actos) reduces blood glucose, and several studies demonstrate it is an effective treatment for steatosis and steatohepatitis. It also reduces the progression of fibrosis and cardiovascular risk. Since pioglitazone can cause fluid retention and weight gain, avoid using it in those with heart failure. See our Meds for Liver Disease Blog for more info.
Answer 3 is incorrect. About 7.31% of respondents chose this. “Avoid insulin therapy in individuals with steatosis and advanced cirrhosis.” With advanced cirrhosis, many of the oral medications may not be safe to use. The ADA recommends using insulin therapy, since it is safe and effective for people experiencing cirrhosis. Since people with cirrhosis are at higher risk of hypoglycemia, close monitoring of glucose levels is recommended. See our Meds for Liver Disease Blog for more info.
Finally, Answer 4 is incorrect. 13.61% chose this answer. “Statin therapy is not effective at LDL lowering for individuals with steatosis.” Lipid-lowering and antihypertensive meds need to be prescribed in people with steatosis as indicated. Statins are safe in individuals with steatohepatitis but avoid their use in those with decompensated cirrhosis. See our Meds for Liver Disease Blog for more info.
We hope you appreciate this week’s rationale! Thank you so much for taking the time to answer our Question of the Week and participate in this fun learning activity!
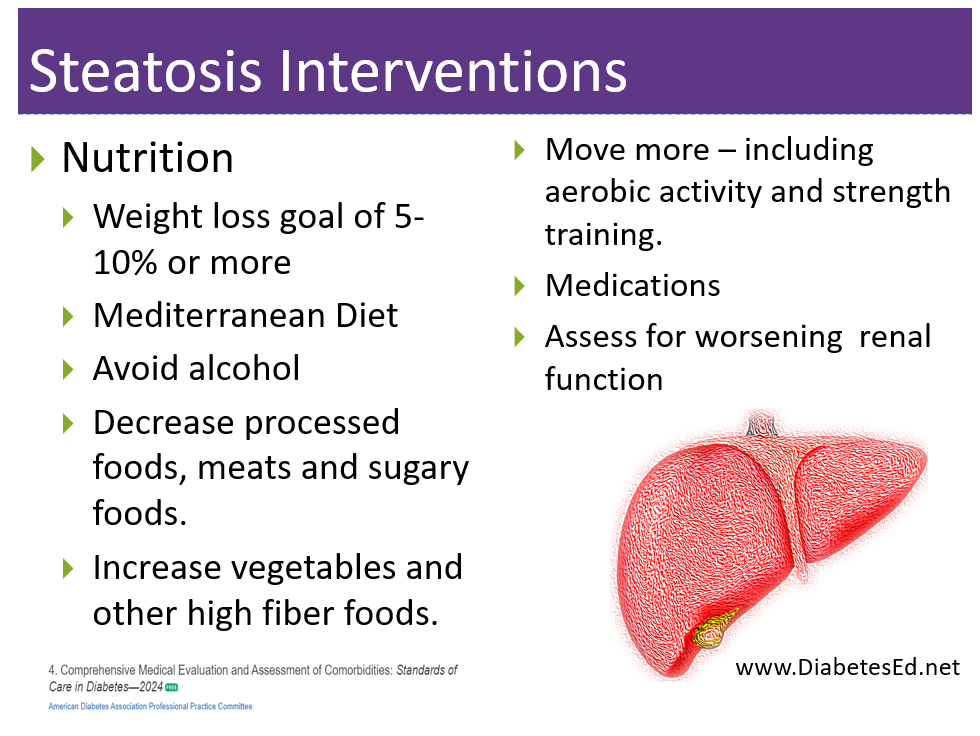
Want to learn more about this question?
Join us live on March 27th, 2024 for our
Critical Assessment in Diabetes Care | Fine-Tuning Diabetes Detective Skills
Level 2 | Standards of Care Intensive
This course integrates the American Diabetes Association’s (ADA) Standard of Care on elements of a comprehensive medical assessment (Standard 4) of the individual living with prediabetes, diabetes, or hyperglycemia. Through case studies & real-life situations, we discover often hidden causes of hyperglycemia & other complications, such as liver disease, sleep apnea, pancreatitis, autoimmune diseases, fractures, & more. We delve into therapy for complicated situations & discuss management strategies for other conditions associated with hyperglycemia such as Cystic Fibrosis, & Transplants.
Objectives:
- Identify common yet often underdiagnosed complications associated with type 1 & type 2 diabetes.
- State strategies to identify previously undiscovered diabetes complications during assessments.
- Discuss links between hyperglycemia & other conditions including transplant, cystic fibrosis, & liver disease.
Intended Audience: These courses are knowledge-based activities designed for individual or groups of diabetes educators, including RNs, RDs, Pharmacists, Nurse Practitioners, Clinical Nurse Specialists, Physician Assistants, and other health care providers interested in enhancing their diabetes assessment skills and preparing for certification.
Instructor: Beverly Thomassian RN, MPH, CDCES, BC-ADM is a working diabetes specialist and a nationally recognized diabetes expert.
Sign up for Diabetes Blog Bytes – we post weekly Blog Bytes that are informative and FREE! Every week we post one exam practice Question of the Week and Rationale of the Week. Sign up below!
Recent Blog Bytes
- February 2026 eNews
- Rationale of the Week | Best Response for Facilitating Positive Health Behavior Change?
- Question of the Week | Which Feature Most Strongly Supports a Diagnosis of HHS Rather Than DKA?
- Rationale of the Week | What Does J.C.’s Family History & Lab Work Reveal?
- Red Flags for Low Digital Literacy in Diabetes Care
Accreditation: Diabetes Education Services is an approved provider by the California Board of Registered Nursing, Provider 12640, and our CPEU courses have received Prior Approval* from the Commission of Dietetic Registration (CDR), Provider DI002. Since our CPEU courses received Prior approval* from the CDR, these CPEU courses satisfy the CE requirements for the CDCES /BC-ADM regardless of your profession!
The use of DES products does not guarantee the successful passage of the certification exam. CBDCE and ADCES do not endorse any preparatory or review materials for the CDCES or BC-ADM exams, except for those published by CBDCE & ADCES.
Rationale of the Week | How to Increase Participation in DSMES?
For last week’s practice question, we quizzed participants on how to Increase participation in DSMES. 75% of respondents chose the best answer. We want to clarify and share this important information, so you can pass it on to people living with diabetes and your colleagues, plus prepare for exam success!
Before we start though, if you don’t want any spoilers and haven’t tried the question yet, you can answer it below: Answer Question

Question: Studies indicate that only 53% of individuals eligible for Diabetes Self-Management Education and Support (DSMES) through their health insurance receive it.
Answer Choices:
- Adjust DSMES charges for Medicare enrollees based on ability to pay.
- Increase access to telehealth delivery of care and other digital health solutions.
- Provide DSMES in non-hospital workplace settings to increase access for employees.
- Incentivize participation through use of giveaways and positive reinforcement.
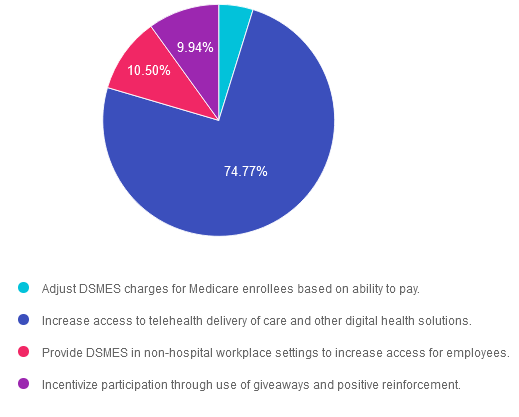
Getting to the Best Answer
Answer 1 is incorrect. 4.79% chose this answer. “Adjust DSMES charges for Medicare enrollees based on ability to pay.” To ensure parity, Medicare guidelines specifically state that all DSME participants must be billed at the same rate. Billing at a lower rate or offering DSME for reduced rates or free for some, but not for all, is prohibited.
Answer 2 is correct. 74.77% of you chose this answer. “Increase access to telehealth delivery of care and other digital health solutions.” YES, GREAT JOB! To promote equity and outreach to rural and under resourced communities, the ADA encourages leveraging technology platforms and telehealth to deliver DSMES.
Answer 3 is incorrect. About 10.5% of respondents chose this. “Provide DSMES in non-hospital workplace settings to increase access for employees.” This is a tempting answer, but unfortunately it is not accurate. The location where DSMES is delivered must have prior approval as a Medicare recognized site in order to be able to bill for services. Of course, providing onsite worksite wellness and lifestyle coaching is beneficial, but it would not be a billable service unless the facility has a recognized DSMES program and an approved site.
Finally, Answer 4 is incorrect. 9.94% chose this answer. “Incentivize participation through use of giveaways and positive reinforcement.” Although this is another tempting answer and could help improve DSMES participation in real-life, the ADA Standards don’t include this strategy as a means to boost enrollment.
We hope you appreciate this week’s rationale! Thank you so much for taking the time to answer our Question of the Week and participate in this fun learning activity!
Want to learn more about this question?
Virtual DiabetesEd Training Conference – Join us Live on April 17th – 19th 2024 at 11:30 AM PST

Join Coach Beverly and Team for two and a half days of knowledge-sharing, fun, and “aha” moments for our Virtual DiabetesEd Training Conference April 17th – 19th, 2024.
Attendees will leave this conference with new tools and a refreshed understanding of the latest advances in person-centered diabetes care. Our team highlights the ADA Standards of Care, medications, behavior change, technology, medical nutrition therapy, and more!
Our instructors co-teach the content to keep things fresh and lively.
Friend Discount: 3 or more only $449 per person. Email us at [email protected] with the name and email of each registrant to get the discount!
Program Details
- Dates: April 17-19th, 2024
- Registration Fee: $399-$569 (see more about reg. options below)
- Friend Discount: For 3 or more people, each person saves $50 off their registration. Email us at [email protected] with the name and email of each registrant to get the discount!
- CEs: 30+ CEs | 18 units for Virtual Conference plus 10+ Bonus CEs. CEs can be applied toward CDCES’s initial application or renewal.
- Speakers: View Conference Faculty
Registration Options
Sign up for Diabetes Blog Bytes – we post weekly Blog Bytes that are informative and FREE! Every week we post one exam practice Question of the Week and Rationale of the Week. Sign up below!
Recent Blog Bytes
- February 2026 eNews
- Rationale of the Week | Best Response for Facilitating Positive Health Behavior Change?
- Question of the Week | Which Feature Most Strongly Supports a Diagnosis of HHS Rather Than DKA?
- Rationale of the Week | What Does J.C.’s Family History & Lab Work Reveal?
- Red Flags for Low Digital Literacy in Diabetes Care
Accreditation: Diabetes Education Services is an approved provider by the California Board of Registered Nursing, Provider 12640, and our CPEU courses have received Prior Approval* from the Commission of Dietetic Registration (CDR), Provider DI002. Since our CPEU courses received Prior approval* from the CDR, these CPEU courses satisfy the CE requirements for the CDCES /BC-ADM regardless of your profession!
The use of DES products does not guarantee the successful passage of the certification exam. CBDCE and ADCES do not endorse any preparatory or review materials for the CDCES or BC-ADM exams, except for those published by CBDCE & ADCES.
Rationale of the Week | Assessing for Food Insecurity with Diabetes
For last week’s practice question, we quizzed participants on assessing food insecurity with diabetes. 60% of respondents chose the best answer. We want to clarify and share this important information, so you can pass it on to people living with diabetes and your colleagues, plus prepare for exam success!
Before we start though, if you don’t want any spoilers and haven’t tried the question yet, you can answer it below: Answer Question

Question: Food insecurity affects 16% of adults with diabetes compared with 9% of adults without diabetes.
Based on the ADA standards of care, which is the most accurate statement regarding food insecurity and people with diabetes?
Answer Choices:
- Food insecurity is defined as uncertain availability of nutritionally adequate food at least once a week.
- Conduct food insecurity screening and income assessment once every 3-5 years.
- Any health care team member can screen for food insecurity using The Hunger Vital Sign.
- People with food insecurity are less likely to experience hyperglycemia due to decreased caloric intake.
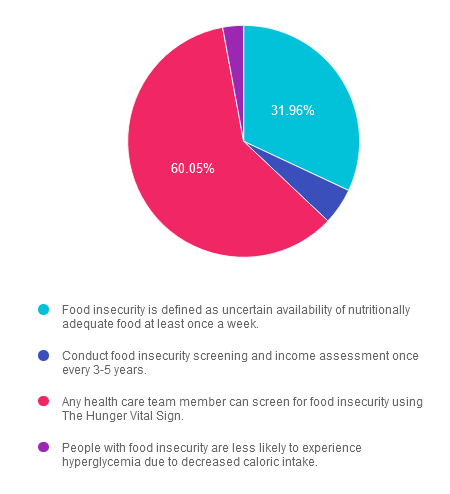
Getting to the Best Answer
Answer 1 is incorrect. 31.96% chose this answer. “Food insecurity is defined as uncertain availability of nutritionally adequate food at least once a week.” Although this answer is partially correct, the last part, “at least once a week” makes this answer incorrect. According to the USDA food insecurity is defined as, “the limited or uncertain availability of nutritionally adequate and safe foods, or limited or uncertain ability to acquire acceptable foods in socially acceptable ways.” It doesn’t include a time span or frequency.
Answer 2 is incorrect. 5.08% of you chose this answer. “Conduct food insecurity screening and income assessment once every 3-5 years.” This answer also has elements of accuracy, but flails at the end. The ADA Standards recommend conducting food insecurity screenings on a yearly basis and helping individuals access needed resources.
Answer 3 is correct. Great Job! About 60.05% of respondents chose this. “Any health care team member can screen for food insecurity using The Hunger Vital Sign.”
The Hunger Vital Sign identifies households as being at risk for food insecurity if they answer that either or both of the following two statements is ‘often true’ or ‘sometimes true’ (vs. ‘never true’):
“ Within the past 12 months we worried whether our food would run out before we got money to buy more.”
“ Within the past 12 months the food we bought just didn’t last and we didn’t have money to get more.”
Finally, Answer 4 is incorrect. 2.91% chose this answer. “People with food insecurity are less likely to experience hyperglycemia due to decreased caloric intake.” There is no scientific evidence to support this answer and people with food insecurity can experience periods of adequate food intake interspersed with inadequate food intake.
We hope you appreciate this week’s rationale! Thank you so much for taking the time to answer our Question of the Week and participate in this fun learning activity!








