Rationale of the Week | Bone Fracture Prevention Based on 2024 ADA Standards

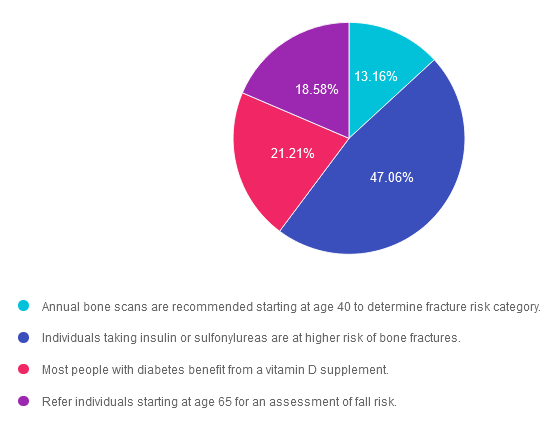
For last week’s practice question, we quizzed participants on bone fracture prevention based on ADA Standards. 47% of respondents chose the best answer. We want to clarify and share this important information, so you can pass it on to people living with diabetes and your colleagues, plus prepare for exam success!
Before we start though, if you don’t want any spoilers and haven’t tried the question yet, you can answer it below: Answer Question
Question: Since people with diabetes are at increased risk of fractures, the 2024 Standards have an increased focus on preventing bone fractures.
Which of the following is an accurate statement regarding diabetes and bone fractures?
Answer Choices:
- Annual bone scans are recommended starting at age 40 to determine fracture risk category.
- Individuals taking insulin or sulfonylureas are at higher risk of bone fractures.
- Most people with diabetes benefit from a vitamin D supplement.
- Refer individuals starting at age 65 for an assessment of fall risk.
Getting to the Best Answer
If you are thinking about taking the certification exam, this practice test question will set you up for success. Test writers anticipate possible answers based on the details in the question. They will wave those “juicy answers” right under your nose. Your job is to weed through the particulars, pluck out the most important elements and choose the BEST answer.
Answer 1 is incorrect. 13.16% chose this answer. “Annual bone scans are recommended starting at age 40 to determine fracture risk category.” This answer is tempting, but it doesn’t match the ADA Standards that recommend to, “Monitor bone mineral density using dual-energy X-ray absorptiometry of high-risk older adults with diabetes starting at age 65 and younger individuals with diabetes and multiple risk factors every 2–3 years.”
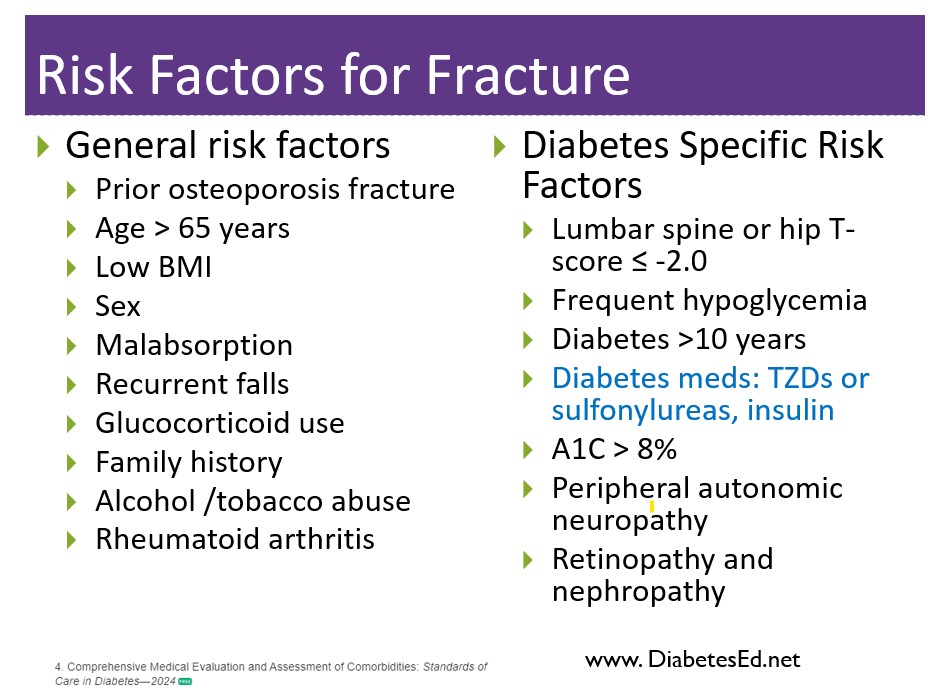
Answer 2 is correct. 47.06% of you chose this answer. “Individuals taking insulin or sulfonylureas are at higher risk of bone fractures.” Yes, this is the best answer. People taking medications that can cause hypoglycemia are at higher risk of falls. Clinicians need to consider the potential adverse impact on bone health when selecting pharmacological options to lower glucose levels in people with diabetes. Prioritizing medications with a proven safety profile for bones is recommended, particularly for those at elevated risk for fractures.
Answer 3 is incorrect. About 21.21% of respondents chose this. “Most people with diabetes benefit from a vitamin D supplement.” This answer is also tempting, but the ADA Standards of Care does not recommend vitamin therapy for “most people”. Vitamin therapy is based on an individual assessment of potential benefit.
Finally, Answer 4 is incorrect. 18.58% chose this answer. “Refer individuals starting at age 65 for an assessment of fall risk.” This answer is tempting, but the ADA recommends we individualize our approach and consider risk of falls and fractures on a ongoing basis. “Fracture risk should be assessed in older adults with diabetes as a part of routine care in diabetes clinical practice, according to risk factors and comorbidities”
We hope you appreciate this week’s rationale! Thank you so much for taking the time to answer our Question of the Week and participate in this fun learning activity!
Learn more about Bone Fracture Prevention and ADA Standards
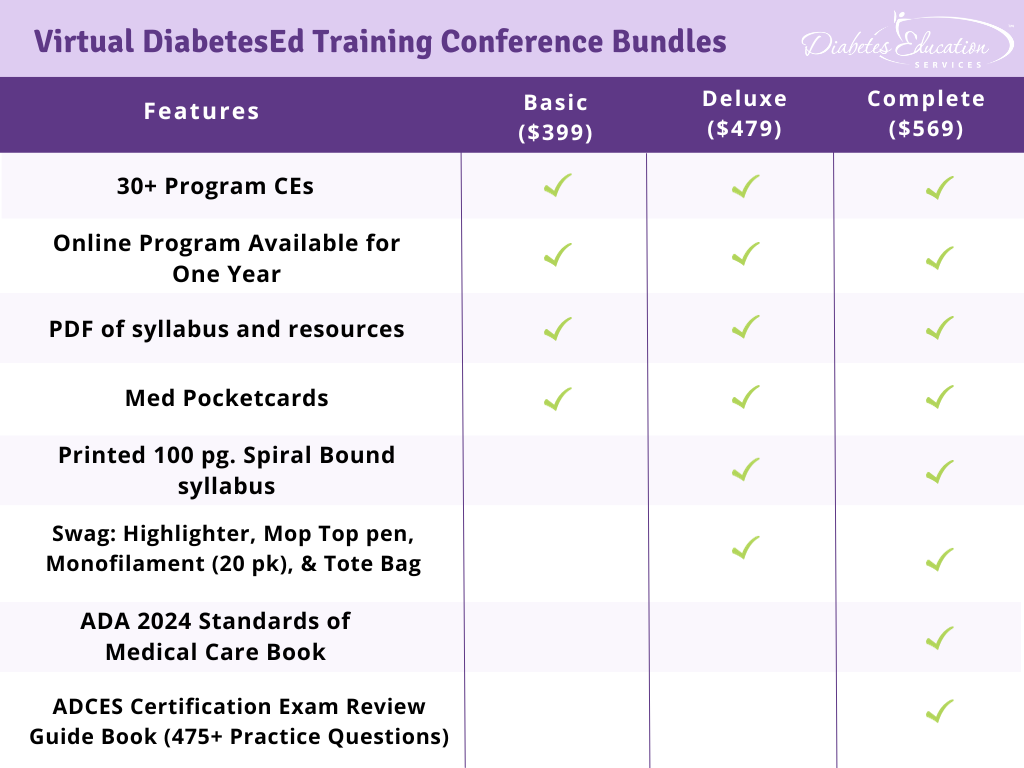
Virtual DiabetesEd Training Conference – Join us Live on April 17th – 19th 2024 at 11:30 AM PST

Join Coach Beverly and Team for two and a half days of knowledge-sharing, fun, and “aha” moments for our Virtual DiabetesEd Training Conference April 17th – 19th, 2024.
Attendees will leave this conference with new tools and a refreshed understanding of the latest advances in person-centered diabetes care. Our team highlights the ADA Standards of Care, medications, behavior change, technology, medical nutrition therapy, and more!
Our instructors co-teach the content to keep things fresh and lively.
Friend Discount: 3 or more only $449 per person. Email us at [email protected] with the name and email of each registrant to get the discount!
Program Details
- Dates: April 17-19th, 2024
- Registration Fee: $399-$569 (see more about reg. options below)
- Friend Discount: For 3 or more people, each person saves $50 off their registration. Email us at [email protected] with the name and email of each registrant to get the discount!
- CEs: 30+ CEs | 18 units for Virtual Conference plus 10+ Bonus CEs. CEs can be applied toward CDCES’s initial application or renewal.
- Speakers: View Conference Faculty
Registration Options
Sign up for Diabetes Blog Bytes – we post one daily Blog Byte from Monday to Friday. And of course, Tuesday is our Question of the Week. It’s Informative and FREE! Sign up below!
Accreditation: Diabetes Education Services is an approved provider by the California Board of Registered Nursing, Provider 12640, and our CPEU courses have received Prior Approval* from the Commission of Dietetic Registration (CDR), Provider DI002. Since our CPEU courses received Prior approval* from the CDR, these CPEU courses satisfy the CE requirements for the CDCES /BC-ADM regardless of your profession!
The use of DES products does not guarantee the successful passage of the certification exam. CBDCE and ADCES do not endorse any preparatory or review materials for the CDCES or BC-ADM exams, except for those published by CBDCE & ADCES.
Rationale of the Week | Best Intervention to address Elevated LDL?

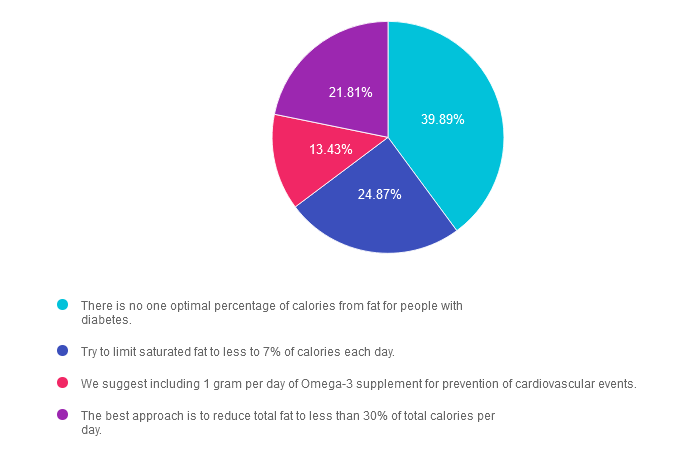
For last week’s practice question, we quizzed participants on the best intervention to address elevated LDL. 40% of respondents chose the best answer. We want to clarify and share this important information, so you can pass it on to people living with diabetes and your colleagues, plus prepare for exam success!
Before we start though, if you don’t want any spoilers and haven’t tried the question yet, you can answer it below: Answer Question
Question:
MK is 67 years old and is concerned about cardiovascular disease risk and diabetes. Their last lab result showed an A1C of 6.8%, HDL of 38 and LDL of 132. MK started reading food labels and is concerned about their total fat intake each day and wants to make diet changes to reduce CVD risk.
According to the 2024 ADA Standards of Care, which evidence-based statement is most accurate when counseling MK about their fat intake?
Answer Choices:
- There is no one optimal percentage of calories from fat for people with diabetes.
- Try to limit saturated fat to less to 7% of calories each day.
- We suggest including 1 gram per day of Omega-3 supplement for prevention of cardiovascular events.
- The best approach is to reduce total fat to less than 30% of total calories per day.
Getting to the Best Answer
If you are thinking about taking the certification exam, this practice test question will set you up for success. Test writers anticipate possible answers based on the details in the question. They will wave those “juicy answers” right under your nose. Your job is to weed through the particulars, pluck out the most important elements and choose the BEST answer.
Answer 1 is correct. GREAT JOB! 39.89% chose this answer, “There is no one optimal percentage of calories from fat for people with diabetes.” The Standards of Care 2024 states, “There is no optimal percentage of calories from fat for people with diabetes or at risk for diabetes, and macronutrient distribution should be individualized.” In addition, there is no optimal percentage of calories from fat or saturated fat for people with diabetes and CVD prevention goals; however, they recommend to “limit” daily saturated fat consumption. The type of fat consumed is more important than the total amount of fat from calories.
Answer 2 is incorrect. 24.87% of you chose this answer. “Try to limit saturated fat to less to 7% of calories each day.” The standards of care do not have a recommended limit for saturated fat consumption but suggest that “people with diabetes or at risk for diabetes follow recommended guidelines for the general population.” The Dietary Guidelines for Americans 2020-2025 recommends less than 10% of calories from saturated fat. Even if considering tighter American Heart Association recommendations, they allow 5-6% of calories from saturated fat. Some eating patterns, such as the TLC diet from 2005, the DASH diet, or the Mediterranean diet, may include food choices where saturated fat is less than 7% of calories, but this is not a general population guideline.
Answer 3 is incorrect. About 13.43% of respondents chose this. “We suggest including 1 gram per day of Omega-3 supplement for prevention of cardiovascular events.” There is no recommendation for omega-3 supplementation in all persons with diabetes. Current evidence within the standard of care states that 1 gram of Omega 3 supplementation showed no benefit in preventing cardiovascular disease; however, within the REDUCE-IT trial, supplementation of pure EPA at 4 grams each day did lower cardiovascular events.
Answer 4 is incorrect. 21.81% chose this answer. “The best approach is to reduce total fat to less than 30% of total calories per day.” There is no specific recommendation for total fat amount to limit in a meal plan. The standards of care state, “The type of fat consumed is more important than the total.” They recommend following a Mediterranean-like eating pattern, which includes foods like fatty fish, nuts, and seeds and is rich in polyunsaturated and monounsaturated fats.
We hope you appreciate this week’s rationale! Thank you so much for taking the time to answer our Question of the Week and participate in this fun learning activity!
Want to learn more about nutrition and the ADA Standards?
Level 3 | DiabetesEd Certification Boot Camp
with Coach Beverly, RN, MPH, CDCES &
Christine Craig, MS, RDN, CDCES
Airs live on February 13th – March 19th, 2024, at 11:30 am PT

Class Topics & Webinar Dates:
- February 13, 2024 – Boot Camp 1: Diabetes | Not Just Hyperglycemia | 1.75 CEs
- February 15, 2024 – Boot Camp 2: Standards of Care & Cardiovascular Goals | 1.8 CEs
- February 20, 2024 – Boot Camp 3: Meds for Type 2 | What you need to know | 1.75 CEs
- February 22, 2024 – Boot Camp 4: Insulin Therapy | From Basal/Bolus to Pattern Management | 1.75 CEs
- February 27, 2024 – Boot Camp 5: Insulin Intensive & Risk Reduction | Monitoring, Sick Days, Lower Extremities | 1.75 CEs
- February 29, 2024 – Boot Camp 6: Medical Nutrition Therapy | 1.75 CEs
- March 12, 2024 – Boot Camp 7: Microvascular Complications & Exercise | Screen, Prevent, Treat | 1.75 CEs
- March 14, 2024 – Boot Camp 8: Coping & Behavior Change | 1.75 CEs
- March 19, 2024 – Boot Camp 9: Test-Taking Coach Session (48 Questions) | No CE
Intended Audience: This library of critical information is designed for individuals or groups of diabetes specialists, including RNs, RDs, Pharmacists, Nurse Practitioners, Clinical Nurse Specialists, Physician Assistants, and other health care providers interested in staying up to date on current practices of care for people with diabetes and preparing for the BC-ADM or the CDCES certification Exam.
Can’t make it live? No worries. We will send post the recorded version to the Online University within 24 hours of the broadcast
Instructors: Beverly Thomassian RN, MPH, CDCES, has been Board Certified in Advanced Diabetes Management for over 15 years. She is an Associate Clinical Professor at UCSF, a working educator, and a nationally recognized diabetes expert.
Christine Craig, MS, RD, CDCES, winner of the 2023 Impact on Diabetes Award, is a leader in the field of nutrition, technology, and diabetes care. Her years of expertise combined with her person-centered approach and work ethic, make her a perfect speaker for this nutrition and activity focused content.
Sign up for Diabetes Blog Bytes – we post one daily Blog Byte from Monday to Friday. And of course, Tuesday is our Question of the Week. It’s Informative and FREE! Sign up below!
Accreditation: Diabetes Education Services is an approved provider by the California Board of Registered Nursing, Provider 12640, and our CPEU courses have received Prior Approval* from the Commission of Dietetic Registration (CDR), Provider DI002. Since our CPEU courses received Prior approval* from the CDR, these CPEU courses satisfy the CE requirements for the CDCES /BC-ADM regardless of your profession!
The use of DES products does not guarantee the successful passage of the certification exam. CBDCE and ADCES do not endorse any preparatory or review materials for the CDCES or BC-ADM exams, except for those published by CBDCE & ADCES.
Rationale of the Week | Best treatment for Hospital and Heart failure?

For last week’s practice question, we quizzed participants on the best treatment for hospitals & heart failure. 73% of respondents chose the best answer. We want to clarify and share this important information, so you can pass it on to people living with diabetes and your colleagues, plus prepare for exam success!
Before we start though, if you don’t want any spoilers and haven’t tried the question yet, you can answer it below: Answer Question
Question: JR has newly discovered type 2 diabetes and is admitted to the hospital with heart failure. Their A1C is 7.9% with negative ketones and a GFR greater than 90 mg/g.
According to the 2024 ADA Standards of Care, which of the following is a recommended intervention during JR’s hospital stay?
Answer Choices:
- Assess for immune mediated diabetes markers, starting with GAD.
- Utilize a mild insulin sliding scale to minimize risk of worsening heart failure.
- Initiate a SGLT-2 during hospitalization and continue upon discharge.
- Encourage a sleep study evaluation to determine if JR also has sleep apnea.
Getting to the Best Answer
If you are thinking about taking the certification exam, this practice test question will set you up for success. Test writers anticipate possible answers based on the details in the question. They will wave those “juicy answers” right under your nose. Your job is to weed through the particulars, pluck out the most important elements and choose the BEST answer.
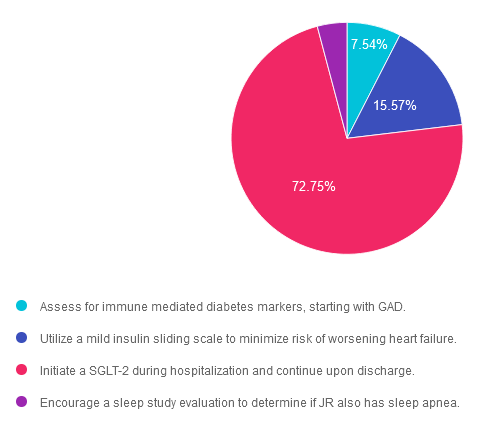
Answer 1 is incorrect. 7.54% chose this answer. “Assess for immune mediated diabetes markers, starting with GAD.” Given that JR’s A1C is 7.9% and their ketones are negative, it seems unlikely they might have undiscovered immune mediated diabetes. The most pressing issue in addition to their diabetes is addressing the CHF.
Answer 2 is incorrect. 15.57% of you chose this answer. “Utilize a mild insulin sliding scale to minimize risk of worsening heart failure.” Based on the ADA Standards of care, insulin sliding scale as the only treatment approach is not recommended. In addition, insulin therapy doesn’t aggravate heart failure.
Answer 3 is correct. About 72.75% of respondents chose this. “Initiate a SGLT-2 during hospitalization and continue upon discharge.” YES, this is the best answer. Given that JR has diabetes and heart failure, using a SGLT-2 will lower their blood sugar plus provide a “glucoretic” effect, which will promote diuresis.
Finally, Answer 4 is incorrect. 4.14% chose this answer. “Encourage a sleep study evaluation to determine if JR also has sleep apnea.” From the information provided, there is no indication that JR is experiencing sleep apnea. The most pressing issues are the CHF and new diabetes diagnosis.
We hope you appreciate this week’s rationale! Thank you so much for taking the time to answer our Question of the Week and participate in this fun learning activity!
Want to learn more about this question?
Enroll in our ADA Standards of Care Update
Airs live today, February 1st, 2024, at 11:30 am PT
Objectives:
- A review of changes & updates to the annual ADA Standards of Medical Care in Diabetes.
- Identification of key elements of the position statement.
- Discussion of how diabetes educators can apply this information in their clinical setting.
Intended Audience: This course is a knowledge-based activity designed for individuals or groups of diabetes professionals, including RNs, RDs, Pharmacists, Nurse Practitioners, Clinical Nurse Specialists, Physician Assistants, and other healthcare providers interested in staying up to date on current practices of care for people with prediabetes, diabetes, and other related conditions.
Can’t make it live? No worries. We will send post the recorded version to the Online University within 24 hours of the broadcast
Instructor: Beverly Thomassian RN, MPH, CDCES, has been Board Certified in Advanced Diabetes Management for over 20 years. She is an Associate Clinical Professor at UCSF, a working educator, and a nationally recognized diabetes expert. She has a Master’s Degree in Public Health from UCLA, with a focus on behavioral health and education.
Sign up for Diabetes Blog Bytes – we post one daily Blog Byte from Monday to Friday. And of course, Tuesday is our Question of the Week. It’s Informative and FREE! Sign up below!
Accreditation: Diabetes Education Services is an approved provider by the California Board of Registered Nursing, Provider 12640, and our CPEU courses have received Prior Approval* from the Commission of Dietetic Registration (CDR), Provider DI002. Since our CPEU courses received Prior approval* from the CDR, these CPEU courses satisfy the CE requirements for the CDCES /BC-ADM regardless of your profession!
The use of DES products does not guarantee the successful passage of the certification exam. CBDCE and ADCES do not endorse any preparatory or review materials for the CDCES or BC-ADM exams, except for those published by CBDCE & ADCES.
Rationale of the Week | Best action to determine if JR “really” has diabetes based on ADA Standards.

For last week’s practice question, we quizzed participants on determining if someone has diabetes based on ADA Standards. 49% of respondents chose the best answer. We want to clarify and share this important information, so you can pass it on to people living with diabetes and your colleagues, plus prepare for exam success!
Before we start though, if you don’t want any spoilers and haven’t tried the question yet, you can answer it below: Answer Question
Question: JR is 47 years old and who just got lab results from their annual physical. Their fasting plasma glucose result was 129 mg/dL. The provider is worried that JR might have diabetes and sent them to back to the lab to check their A1C, which came back 6.4%.
According to the 2024 ADA Standards, to most accurately assess if JR has diabetes, which of the following follow-up actions is recommended?
Answer Choices:
- Recheck the A1C in 3 months.
- Order a meter for JR, so they can check fasting and post-prandial glucose for one month.
- Evaluate JR for immune mediated diabetes antibodies.
- Recheck the fasting blood glucose.
Getting to the Best Answer
If you are thinking about taking the certification exam, this practice test question will set you up for success. Test writers anticipate possible answers based on the details in the question. They will wave those “juicy answers” right under your nose. Your job is to weed through the particulars, pluck out the most important elements and choose the BEST answer.
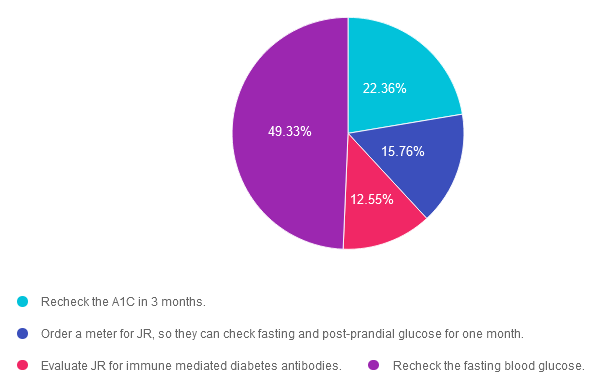
Answer 1 is incorrect. 22.36% chose this answer. Recheck the A1C in 3 months. According to ADA Standard 2 on Diagnosis and Classification of Diabetes, “if an individual has discordant results from two different tests, then the test result that is above the diagnostic cut point should be repeated, with careful consideration of factors that may affect measured A1C or glucose levels.” Since JR’s fasting BG test result meets the diagnostic threshold of equal to or greater than 126 mg/dL, we would need to repeat the fasting test, to see if the second lab would confirm diagnosis. We would also consider factors (hemoglobinopathies, lab issues) that might be affecting the accuracy of the A1C result.
Answer 2 is incorrect. 15.76% of you chose this answer. Order a meter for JR, so they can check fasting and post-prandial glucose for one month. Since home glucose meters have limited accuracy, they are not recommended for diagnosis of diabetes. In addition “if an individual has discordant results from two different tests, then the test result that is above the diagnostic cut point should be repeated, with careful consideration of factors that may affect measured A1C or glucose levels.” Since JR’s fasting BG test result meets the diagnostic threshold of equal to or greater than 126 mg/dL, we would need to repeat the fasting test, to see if the second lab would confirm diagnosis. We would also consider factors (hemoglobinopathies, lab issues) that might be affecting the accuracy of the A1C result.
Answer 3 is incorrect. About 12.55% of respondents chose this. Evaluate JR for immune mediated diabetes antibodies. In this case study, JR does not present with risk factors or symptoms of immune mediated type 1 diabetes or LADA. However, since their fasting blood sugar meets the diagnostic threshold for diabetes, we need to redraw JR’s fasting blood glucose, to confirm (or dispute) diagnosis.
Finally, Answer 4 is correct. 49.33% chose this answer. Recheck the fasting blood glucose. YES – GREAT JOB, According to ADA Standard 2 on Diagnosis and Classification of Diabetes, “if an individual has discordant results from two different tests, then the test result that is above the diagnostic cut point should be repeated, with careful consideration of factors that may affect measured A1C or glucose levels.” Since JR’s fasting BG test result meets the diagnostic threshold of equal to or greater than 126 mg/dL, we would need to repeat the fasting test, to see if the second lab would confirm diagnosis. We would also consider factors (hemoglobinopathies, lab issues) that might be affecting the accuracy of the A1C result.
On the other hand, if an individual has discordant results from two different tests, then the test result that is above the diagnostic cut point should be repeated, with careful consideration of factors that may affect measured A1C or glucose levels. The diagnosis is made based on the confirmatory screening test. For example, if an individual meets the diabetes criterion of A1C (two results ?6.5% [?48 mmol/mol]) but not FPG (<126 mg/dL [<7.0 mmol/L]), that person should nevertheless be considered to have diabetes.We hope you appreciate this week’s rationale!
Thank you so much for taking the time to answer our Question of the Week and participate in this fun learning activity!
Sign up for Diabetes Blog Bytes – we post one daily Blog Byte from Monday to Friday. And of course, Tuesday is our Question of the Week. It’s Informative and FREE! Sign up below!
Accreditation: Diabetes Education Services is an approved provider by the California Board of Registered Nursing, Provider 12640, and our CPEU courses have received Prior Approval* from the Commission of Dietetic Registration (CDR), Provider DI002. Since our CPEU courses received Prior approval* from the CDR, these CPEU courses satisfy the CE requirements for the CDCES /BC-ADM regardless of your profession!
The use of DES products does not guarantee the successful passage of the certification exam. CBDCE and ADCES do not endorse any preparatory or review materials for the CDCES or BC-ADM exams, except for those published by CBDCE & ADCES.
Rationale of the Week | Best Hypoglycemia Treatment according to 2024 ADA Standards?

For last week’s practice question, we quizzed participants on best approach to treat hypoglycemia according to 2024 ADA Standards. 51% of respondents chose the best answer. We want to clarify and share this important information, so you can pass it on to people living with diabetes and your colleagues, plus prepare for exam success!
Before we start though, if you don’t want any spoilers and haven’t tried the question yet, you can answer it below: Answer Question
Question: The 2024 ADA Standards of Care includes expanded content on the prevention and treatment of hypoglycemia.
Based on the updated guidelines for the treatment of hypoglycemia, which of the following is true?
Answer Choices:
- If blood glucose is less than 70 mg/dL, treat with a combination of fast acting glucose and protein to sustain blood glucose levels.
- Avoid use of glucagon emergency treatment for those with type 2 diabetes to prevent rebound hyperglycemia.
- In community settings, check blood sugar to verify hypoglycemia before providing glucagon emergency treatment.
- If individual has one or more episode of clinically significant hypoglycemia, consider short-term relaxation of glucose goals.
Getting to the Best Answer
If you are thinking about taking the certification exam, this practice test question will set you up for success. Test writers anticipate possible answers based on the details in the question. They will wave those “juicy answers” right under your nose. Your job is to weed through the particulars, pluck out the most important elements and choose the BEST answer.
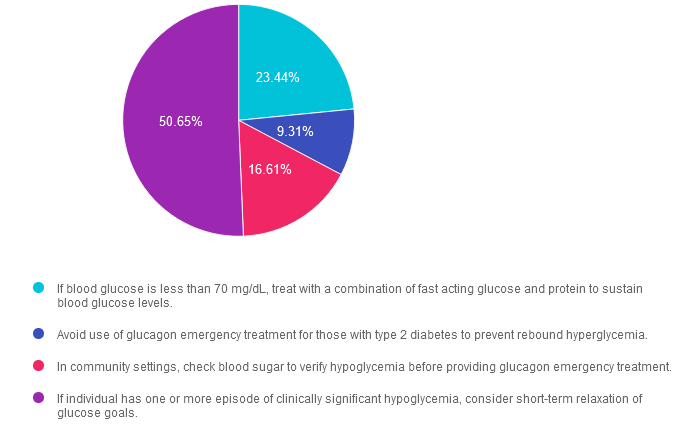
Answer 1 is incorrect. 23.44% chose this answer. “If blood glucose is less than 70 mg/dL, treat with a combination of fast acting glucose and protein to sustain blood glucose levels.” Part of this answer is correct. We need to treat a blood glucose of less than 70 with mg/dL with 15gms of carbohydrate. However, there is no recommendation to add protein to the carbohydrate treatment. As a matter of fact, adding protein (which if often combined with fat) can slow the absorption of the carbohydrate and delay glucose improvement. In addition, for people with beta cell function, the ingestion of protein can stimulate insulin production.
Answer 2 is incorrect. 9.31% of you chose this answer. “Avoid use of glucagon emergency treatment for those with type 2 diabetes to prevent rebound hyperglycemia.” The new standards recommend that all people using insulin therapy have access and training on glucagon rescue medications. See our Glucagon Pocketcards.
Answer 3 is incorrect. 16.61% of respondents chose this. “In community settings, check blood sugar to verify hypoglycemia before providing glucagon emergency treatment.” In the community or home setting, there may be limited access to glucose monitors and the public may not know how to check blood sugars, which could lead to delayed treatment for this emergency situation. For this reason, if a person has diabetes and is experiencing an episode of severe hypoglycemia, it is recommended to provide a glucagon rescue medication and activate the emergency response system if warranted. See our Glucagon Pocketcards.
Finally, Answer 4 is correct. 50.65% chose this answer. “If individual has one or more episode of clinically significant hypoglycemia, consider short-term relaxation of glucose goals.” YES, this is the BEST answer. If a person has an episode of clinically significant hypoglycemia, it is an indication that they may be taking too much insulin or diabetes medication. In addition, experiencing hypoglycemia puts individuals at a higher risk for another episode of significant hypoglycemia. Relaxing glucose goals and up-adjusting them can help the person re-set their “glucose thermostat” in a safer range with the ultimate goal of preventing future hypoglycemia.
We hope you appreciate this week’s rationale! Thank you so much for taking the time to answer our Question of the Week and participate in this fun learning activity!
Sign up for Diabetes Blog Bytes – we post one daily Blog Byte from Monday to Friday. And of course, Tuesday is our Question of the Week. It’s Informative and FREE! Sign up below!
Accreditation: Diabetes Education Services is an approved provider by the California Board of Registered Nursing, Provider 12640, and our CPEU courses have received Prior Approval* from the Commission of Dietetic Registration (CDR), Provider DI002. Since our CPEU courses received Prior approval* from the CDR, these CPEU courses satisfy the CE requirements for the CDCES /BC-ADM regardless of your profession!
The use of DES products does not guarantee the successful passage of the certification exam. CBDCE and ADCES do not endorse any preparatory or review materials for the CDCES or BC-ADM exams, except for those published by CBDCE & ADCES.
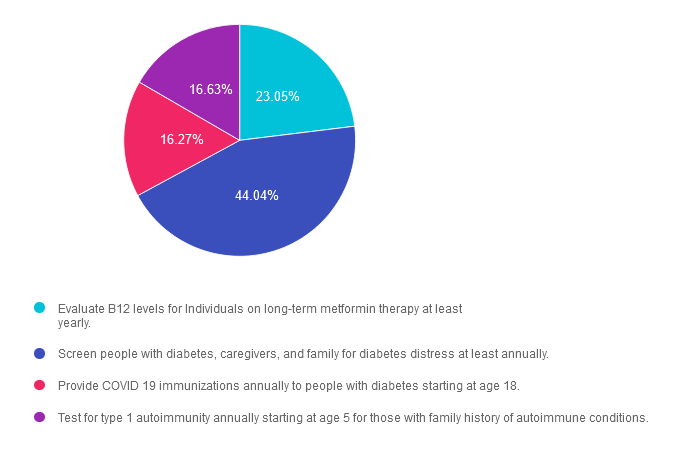
Rationale of the Week | Which is an Accurate 2024 ADA Standard?

For last week’s practice question, we quizzed participants on 2024 ADA Standards. 44% of respondents chose the best answer. We want to clarify and share this important information, so you can pass it on to people living with diabetes and your colleagues, plus prepare for exam success!
Before we start though, if you don’t want any spoilers and haven’t tried the question yet, you can answer it below: Answer Question
Question:
The new ADA 2024 Standards of Care include dozens of updates to diabetes clinical practice.
Which of the following statements has actually been added to the ADA 2024 Standards of Care?
Answer Choices:
- Evaluate B12 levels for Individuals on long-term metformin therapy at least yearly.
- Screen people with diabetes, caregivers, and family for diabetes distress at least annually.
- Provide COVID 19 immunizations annually to people with diabetes starting at age 18.
- Test for type 1 autoimmunity annually starting at age 5 for those with family history of autoimmune conditions.
Getting to the Best Answer
If you are thinking about taking the certification exam, this practice test question will set you up for success. Test writers anticipate possible answers based on the details in the question. They will wave those “juicy answers” right under your nose. Your job is to weed through the particulars, pluck out the most important elements and choose the BEST answer.
Answer 1 is incorrect. 23.05% chose this answer. “Evaluate B12 levels for Individuals on long-term metformin therapy at least yearly.” This juicy answer is very tempting. It is true the metformin can be associated with lower B12 levels. However, the ADA does not recommend checking B12 levels annually for people taking this biguanide. Instead, they suggest regularly monitoring B12 levels in people on metformin therapy who have signs of B12 deficiency such as neuropathy or anemia.
Answer 2 is correct. 44.04% of you chose this answer. “Screen people with diabetes, caregivers, and family for diabetes distress at least annually.” Yes, this is the BEST answer! Many individuals with diabetes experience unrecognized and undertreated diabetes distress, which can lead to decreased engagement in self-management activities and worsen outcomes. We address diabetes distress and discuss strategies to address this common emotional response to diabetes in our ReVive 5 Training Program.
Answer 3 is incorrect. About 16.27% of respondents chose this. “Provide COVID 19 immunizations annually to people with diabetes starting at age 18.” The ADA recommends starting COVID 19 immunizations in people with diabetes starting at 6 months and follow-up with boosters as recommended,
Finally, Answer 4 is incorrect. 16.63% chose this answer. “Test for type 1 autoimmunity annually starting at age 5 for those with family history of autoimmune conditions.” Autoimmune testing is recommended for those with immediate family members with type 1 diabetes and other risk factors. There is no age cut-off nor is there a recommendation for annual testing.
We hope you appreciate this week’s rationale! Thank you so much for taking the time to answer our Question of the Week and participate in this fun learning activity!
Want to learn more about this question?
Enroll in our ADA Standards of Care Update
Airs live on February 1st, 2024, at 11:30 am PT
Objectives:
- A review of changes & updates to the annual ADA Standards of Medical Care in Diabetes.
- Identification of key elements of the position statement.
- Discussion of how diabetes educators can apply this information in their clinical setting.
Intended Audience: This course is a knowledge-based activity designed for individuals or groups of diabetes professionals, including RNs, RDs, Pharmacists, Nurse Practitioners, Clinical Nurse Specialists, Physician Assistants, and other healthcare providers interested in staying up to date on current practices of care for people with prediabetes, diabetes, and other related conditions.
Can’t make it live? No worries. We will send post the recorded version to the Online University within 24 hours of the broadcast
Instructor: Beverly Thomassian RN, MPH, CDCES, has been Board Certified in Advanced Diabetes Management for over 20 years. She is an Associate Clinical Professor at UCSF, a working educator, and a nationally recognized diabetes expert. She has a Master’s Degree in Public Health from UCLA, with a focus on behavioral health and education.
Sign up for Diabetes Blog Bytes – we post one daily Blog Byte from Monday to Friday. And of course, Tuesday is our Question of the Week. It’s Informative and FREE! Sign up below!
The use of DES products does not guarantee the successful passage of the CDCES exam. CBDCE does not endorse any preparatory or review materials for the CDCES exam, except for those published by CBDCE.
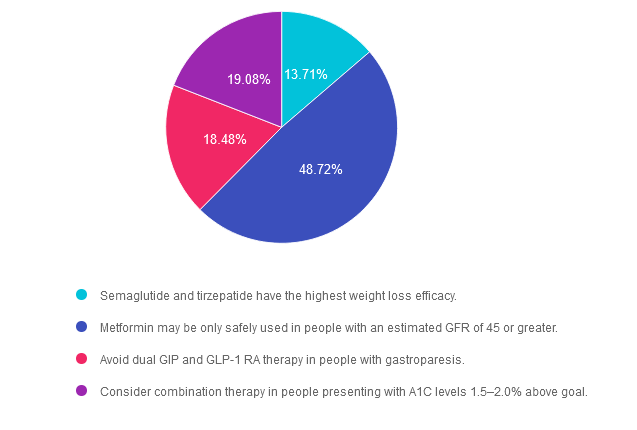
Rationale of the Week | New ADA 2024 Standards – Meds for Type 2 Diabetes

For last week’s practice question, we quizzed participants on the new ADA Standards for type 2 diabetes medication. 49% of respondents chose the best answer. We want to clarify and share this important information, so you can pass it on to people living with diabetes and your colleagues, plus prepare for exam success!
Before we start though, if you don’t want any spoilers and haven’t tried the question yet, you can answer it below: Answer Question
Based on the newly released 2024 American Diabetes Association (ADA) Standards of Care, which of the following statements is NOT accurate regarding treatment for hyperglycemia?
Answer Choices:
- Semaglutide and tirzepatide have the highest weight loss efficacy.
- Metformin may be only safely used in people with an estimated GFR of 45 or greater.
- Avoid dual GIP and GLP-1 RA therapy in people with gastroparesis.
- Consider combination therapy in people presenting with A1C levels 1.5–2.0% above goal.
Getting to the Best Answer
If you are thinking about taking the certification exam, this practice test question will set you up for success. Test writers anticipate possible answers based on the details in the question. They will wave those “juicy answers” right under your nose. Your job is to weed through the particulars, pluck out the most important elements and choose the BEST answer.
Answer 1 is incorrect. 13.71% chose this answer. “Semaglutide and tirzepatide have the highest weight loss efficacy.” This statement is accurate. These two incretin mimetics not only substantially lower A1C levels, they also are associated with the highest percentage of weight loss of all the diabetes medications. See Diabetes Med PocketCards for more information.
Answer 2 is correct. 48.72% of you chose this answer. “Metformin may be only safely used in people with an estimated GFR of 45 or greater.” YES, great job! This answer is FALSE (making it the best answer). If a person with diabetes is taking metformin and their GFR drops below 30, then we stop the medication. However, we can start or continue metformin therapy if the GFR is 45 or greater. In addition, metformin doesn’t harm the kidneys, it actually protects them by lowering blood glucose levels. See Diabetes Med PocketCards for more information.
Answer 3 is incorrect. About 18.48% of respondents chose this. “Avoid dual GIP and GLP-1 RA therapy in people with gastroparesis.” This answer is also accurate. Tirzepatide (Mounjaro) can substantially slow gastric emptying which could exacerbate gastroparesis. For that reason, it is not a recommended therapy for people with gastroparesis.
Finally, Answer 4 is incorrect. 19.08% chose this answer. “Consider combination therapy in people presenting with A1C levels 1.5–2.0% above goal.” This answer is also accurate. The ADA Standards of Care recommend more intensive pharmacologic intervention for those with substantially elevated A1C to improve and prolong pancreatic function.
We hope you appreciate this week’s rationale! Thank you so much for taking the time to answer our Question of the Week and participate in this fun learning activity!
Want to learn more about this question?
ADA Standards of Care Course 2024
Airs Live February 1, 2024 at 11:30 AM PT
Topics:
- A review of changes & updates to the annual ADA Standards of Medical Care in Diabetes.
- Identification of key elements of the position statement.
- Discussion of how diabetes educators can apply this information in their clinical setting
This course, updated annually, is an essential review for anyone in the field of diabetes. Join Coach Beverly as she summarizes the annual updates to the American Diabetes Association’s (ADA) Standards of Medical Care in Diabetes & provides critical teaching points & content for healthcare professionals involved in diabetes care & education.
Can’t make it live? No worries. We will send post the recorded version to the Online University within 24 hours of the broadcast
Instructor: Beverly Thomassian RN, MPH, CDCES, has been Board Certified in Advanced Diabetes Management for over 20 years. She is an Associate Clinical Professor at UCSF, a working educator, and a nationally recognized diabetes expert. She has a Master’s Degree in Public Health from UCLA, with a focus on behavioral health and education.
Sign up for Diabetes Blog Bytes – we post one daily Blog Byte from Monday to Friday. And of course, Tuesday is our Question of the Week. It’s Informative and FREE! Sign up below!
Accreditation: Diabetes Education Services is an approved provider by the California Board of Registered Nursing, Provider 12640, and our CPEU courses have received Prior Approval* from the Commission of Dietetic Registration (CDR), Provider DI002. Since our CPEU courses received Prior approval* from the CDR, these CPEU courses satisfy the CE requirements for the CDCES /BC-ADM regardless of your profession!
The use of DES products does not guarantee the successful passage of the certification exam. CBDCE and ADCES do not endorse any preparatory or review materials for the CDCES or BC-ADM exams, except for those published by CBDCE & ADCES.
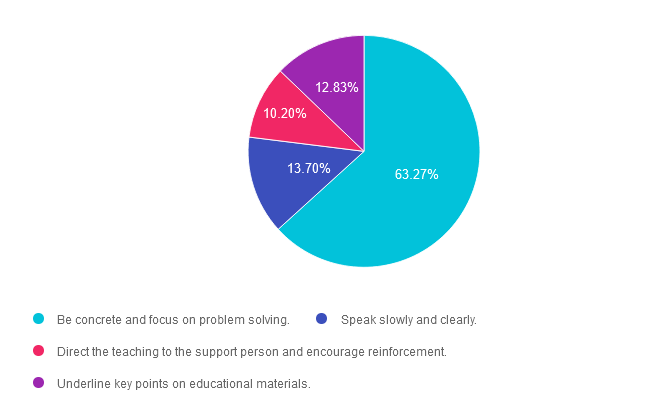
Rationale of the Week | Best approach with Low Literacy?

For last week’s practice question, we quizzed participants on what is the best approach for people with low literacy skills. 63% of respondents chose the best answer. We want to clarify and share this important information, so you can pass it on to people living with diabetes and your colleagues, plus prepare for exam success!
Before we start though, if you don’t want any spoilers and haven’t tried the question yet, you can answer it below: Answer Question
Question: Which of the following strategies is most effective when working with someone with low literacy skills?
Answer Choices:
- Be concrete and focus on problem solving.
- Speak slowly and clearly.
- Direct the teaching to the support person and encourage reinforcement.
- Underline key points on educational materials.
Getting to the Best Answer
If you are thinking about taking the certification exam, this practice test question will set you up for success. Test writers anticipate possible answers based on the details in the question. They will wave those “juicy answers” right under your nose. Your job is to weed through the particulars, pluck out the most important elements and choose the BEST answer.
Answer 1 is correct. 63.27% chose this answer. “Be concrete and focus on problem solving.” Yes, this is the best answer. Since a person with low literacy can’t take notes or read information later, they will need to commit new information to memory. By providing concrete examples and engaging in collaborative problem solving, a person with low literacy can more effectively retain the information.
Answer 2 is incorrect. 13.70% of you chose this answer. “Speak slowly and clearly.” Just because a person hast low literacy doesn’t mean they have an intellectual disability. Maybe they didn’t have a chance to complete their education or experienced some other impediment to learning how to read and write. We can use a usual conversational pace and annunciation with this individual.
Answer 3 is incorrect. About 10.20% of respondents chose this. “Direct the teaching to the support person and encourage reinforcement.” A general rule of effective communication is to direct the teaching and education to the person with diabetes, while including the support person.
Finally, Answer 4 is incorrect. 12.83% chose this answer. “Underline key points on educational materials.” Since people with low literacy have limited ability to read and write, using print materials with words would not be an effective method to provide education. Use of pictures and infographics, videos, podcasts or other educational strategies that don’t require literacy, would be excellent alternatives.
We hope you appreciate this week’s rationale! Thank you so much for taking the time to answer our Question of the Week and participate in this fun learning activity!
Want to learn more about this question?
ADA Standards of Care
Join us live on February 1, 2024, at 11:30 am PST
Topics:
- A review of changes & updates to the annual ADA Standards of Medical Care in Diabetes.
- Identification of key elements of the position statement.
- Discussion of how diabetes educators can apply this information in their clinical setting.
This course, updated annually, is an essential review for anyone in the field of diabetes. Join Coach Beverly as she summarizes the annual updates to the American Diabetes Association’s (ADA) Standards of Medical Care in Diabetes & provides critical teaching points & content for healthcare professionals involved in diabetes care & education.
Can’t make it live? No worries. We will send post the recorded version to the Online University within 24 hours of the broadcast
Instructor: Beverly Thomassian RN, MPH, CDCES, has been Board Certified in Advanced Diabetes Management for over 20 years. She is an Associate Clinical Professor at UCSF, a working educator, and a nationally recognized diabetes expert. She has a Master’s Degree in Public Health from UCLA, with a focus on behavioral health and education.
All hours earned count toward your CDCES Accreditation Information
Sign up for Diabetes Blog Bytes – we post one daily Blog Byte from Monday to Friday. And of course, Tuesday is our Question of the Week. It’s Informative and FREE! Sign up below!
The use of DES products does not guarantee the successful passage of the CDCES exam. CBDCE does not endorse any preparatory or review materials for the CDCES exam, except for those published by CBDCE.








