Rationale of the Week | What is the difference between CDCES vs. BC-ADM?
Rationale of the Week | Euglycemic ketosis – How to best detect?

For last week’s practice question, we quizzed participants on how to best detect euglycemic ketosis. 53% of respondents chose the best answer. We want to clarify and share this important information, so you can pass it on to people living with diabetes and your colleagues, plus prepare for exam success!
Before we start though, if you don’t want any spoilers and haven’t tried the question yet, you can answer it below: Answer Question
Question:
According to recent research by the ADA/EASD, about 10% of people admitted to the hospital in diabetes crisis have euglycemic diabetes ketoacidosis.
Since blood sugars are at normal levels or only slightly elevated, which of the following lab tests most accurately evaluate for euglycemic ketosis?
Answer Choices:
- Blood pH and arterial glucose.
- Beta-hydroxybutyrate and bicarbonate levels.
- Urine ketones and urine glucose.
- Anion gap and glucose level measured in mmol/L.
Getting to the Best Answer
If you are thinking about taking the certification exam, this practice test question will set you up for success. Test writers anticipate possible answers based on the details in the question. They will wave those “juicy answers” right under your nose. Your job is to weed through the particulars, pluck out the most important elements and choose the BEST answer.
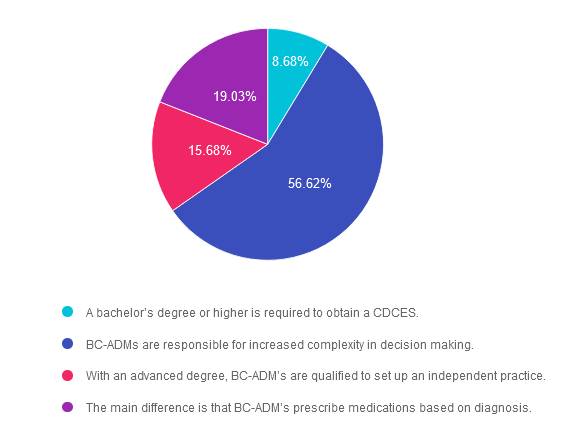
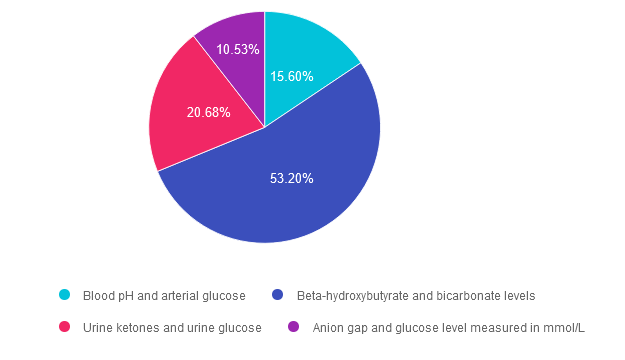
Answer 1 is incorrect. 15.60% chose this answer. “Blood pH and arterial glucose.” Since euglycemic ketosis is often associated with blood glucose levels less than 200 mg/dL, checking arterial glucose levels won’t provide additional clarity on diagnosis. However, checking pH levels is recommended, since a pH less than 7.3 is a clear clinical indication of ketosis.
Answer 2 is correct. 53.20% of you chose this answer. “Beta-hydroxybutyrate and bicarbonate levels.” YES, this is the best answer. Beta-hydroxybutyrate evaluation with a low cutoff equal to or greater than 3.0 mmol/L, whether by lab or point-of-care-testing, is one of the most accurate measurements to evaluate if a person is in ketosis. Bicarbonate level concentration < 18 mmol/L also helps to provide confirmation of ketosis. Ketoacidosis in diabetes is due to inadequate circulating insulin, so the body switches to burning fat for fuel (instead of glucose), which leads to a build up of ketones or ketosis.
Answer 3 is incorrect. About 20.68% of respondents chose this. “Urine ketones and urine glucose.” Urine ketone testing can be used if Beta-hydroxybutyrate evaluation is not available. A urine ketone strip value of 2+ or greater indicates ketosis. However, checking urine glucose levels won’t provide additional clarity on diagnosis, since euglycemic ketosis is often associated with blood glucose levels less than 200 mg/dL.
Finally, Answer 4 is incorrect. 10.53% chose this answer. “Anion gap and glucose level measured in mmol/L.” he anion gap has long been a clinical measure of acidosis; however it is not considered to be a key indicator in the new guidelines. Metabolic acidosis is now defined as a pH < 7.3 and a bicarbonate concentration < 18 mmol/L. The anion gap can still be used in settings where ketone testing is unavailable. In addition, checking urine glucose levels won’t provide additional clarity on diagnosis, since euglycemic ketosis is often associated with blood glucose levels less than 200 mg/dL.
We hope you appreciate this week’s rationale! Thank you so much for taking the time to answer our Question of the Week and participate in this fun learning activity!
Want to learn more about this question?
Join our Annual Webinar
Airs live February 1, 2024 at 11:30 am PT
All hours earned count toward your CDCES Accreditation Information
Sign up for Diabetes Blog Bytes – we post one daily Blog Byte from Monday to Friday. And of course, Tuesday is our Question of the Week. It’s Informative and FREE! Sign up below!
The use of DES products does not guarantee the successful passage of the CDCES exam. CBDCE does not endorse any preparatory or review materials for the CDCES exam, except for those published by CBDCE.
Rationale of the Week | How much does Diabetes Cost the U.S?

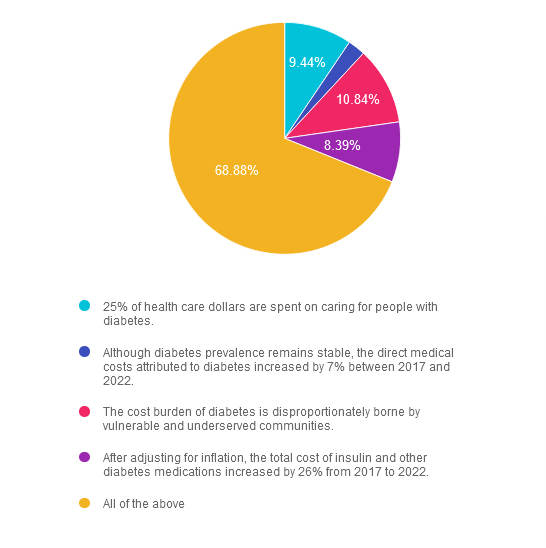
For last week’s practice question, we quizzed participants on how much does Diabetes Cost the U.S? 69% of respondents chose the best answer. We want to clarify and share this important information, so you can pass it on to people living with diabetes and your colleagues, plus prepare for exam success!
Before we start though, if you don’t want any spoilers and haven’t tried the question yet, you can answer it below: Answer Question
Question: According to the recently published ADA report on the 2022 Economic Costs of Diabetes in the U.S., which of the following statements is most accurate?
Answer Choices:
- 25% of health care dollars are spent on caring for people with diabetes.
- Although diabetes prevalence remains stable, the direct medical costs attributed to diabetes increased by 7% between 2017 and 2022.
- The cost burden of diabetes is disproportionately borne by vulnerable and underserved communities.
- After adjusting for inflation, the total cost of insulin and other diabetes medications increased by 26% from 2017 to 2022.
- All of the above
Getting to the Best Answer
If you are thinking about taking the certification exam, this practice test question will set you up for success. Test writers anticipate possible answers based on the details in the question. They will wave those “juicy answers” right under your nose. Your job is to weed through the particulars, pluck out the most important elements and choose the BEST answer.
Answer 1 is incorrect. 9.44% chose this answer. “25% of health care dollars are spent on caring for people with diabetes.” Yes, a quarter of all health care dollars are spent on diabetes, with the majority of money spent on hospitalizations due to cardiovascular complications and medications. Read more details in the Diabetes Care Article, “Economic Costs of Diabetes in the U.S. 2022.
Answer 2 is incorrect. 2.45% of you chose this answer. “Although diabetes prevalence remains stable, the direct medical costs attributed to diabetes increased by 7% between 2017 and 2022.” The cost of treating diabetes keeps increasing, putting additional financial strain on people living with diabetes. Read more details in the Diabetes Care Article, “Economic Costs of Diabetes in the U.S. 2022.
Answer 3 is incorrect. About 10.84% of respondents chose this. “The cost burden of diabetes is disproportionately borne by vulnerable and underserved communities.” People who earn the least amount of money and live in under-resourced areas, continue to have the highest rates of diabetes and other chronic health conditions. Read more details in the Diabetes Care Article, “Economic Costs of Diabetes in the U.S. 2022.
Answer 4 is incorrect. About 8.39% of respondents chose this. “After adjusting for inflation, the total cost of insulin and other diabetes medications increased by 26% from 2017 to 2022.” Yes, the cost of medications keeps increasing, which may prevent many people from accessing optimal diabetes treatment. Read more details in the Diabetes Care Article, “Economic Costs of Diabetes in the U.S. 2022
Finally, Answer 5 is correct. 68.88% chose this answer. “All of the above” YES, GREAT JOB. Most of you chose the BEST Answer. Thank you for participating in our Question of the Week. All data is based on the Diabetes Care Article, “Economic Costs of Diabetes in the U.S. 2022”, published in November 2023
We hope you appreciate this week’s rationale! Thank you so much for taking the time to answer our Question of the Week and participate in this fun learning activity!
All data is based on the Diabetes Care Article, “Economic Costs of Diabetes in the U.S. 2022”, published in November 2023
Join us for our upcoming Hyperglycemic Crises, DKA & HHS Standards webinar
Airs live on December 12th, 2023, at 11:30 am PT
Topics:
- Discuss the common causes of hyperglycemic crises.
- List the differences & similarities between DKA and HHS and treatment strategies.
- Describe the causes & treatment of hyperglycemic crises.
This course discusses common causes of hyperglycemia crises. Topics include hyperglycemia secondary to medications & insulin deprivation. The differences & similarities between Diabetes Ketoacidosis and hyperosmolar Hyperglycemic Syndrome are also covered. Treatment strategies for all situations are included.
Can’t make it live? No worries. We will send post the recorded version to the Online University within 24 hours of the broadcast
Instructor: Beverly Thomassian RN, MPH, CDCES, has been Board Certified in Advanced Diabetes Management for over 20 years. She is an Associate Clinical Professor at UCSF, a working educator, and a nationally recognized diabetes expert. She has a Master’s Degree in Public Health from UCLA, with a focus on behavioral health and education.
All hours earned count toward your CDCES Accreditation Information
Sign up for Diabetes Blog Bytes – we post one daily Blog Byte from Monday to Friday. And of course, Tuesday is our Question of the Week. It’s Informative and FREE! Sign up below!
The use of DES products does not guarantee the successful passage of the diabetes certification exams. CBDCE & ADCES does not endorse any preparatory or review materials for the certification exams, except for those published by CBDCE & ADCES.
Rationale of the Week | Why do we celebrate World Diabetes Day on Nov 14th?

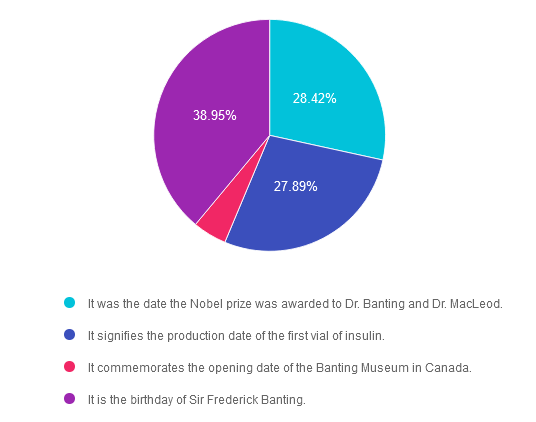
For last week’s practice question, we quizzed participants on why we celebrate World Diabetes Day on Nov 14th. 39% of respondents chose the best answer. We want to clarify and share this important information, so you can pass it on to people living with diabetes and your colleagues, plus prepare for exam success!
Before we start though, if you don’t want any spoilers and haven’t tried the question yet, you can answer it below: Answer Question
Question: In 1923, the Nobel prize in Physiology or Medicine was awarded to Frederick Grant Banting and John James Richard MacLeod “for the discovery of insulin”. 100 years later, we celebrate this life-saving discovery each year on November 14th, a day designated as World Diabetes Day.
Why do we celebrate World Diabetes Day on November 14th? Please choose the best answer.
Answer Choices:
- It was the date the Nobel Prize was awarded to Dr. Banting and Dr. MacLeod.
- It signifies the production date of the first vial of insulin.
- It commemorates the opening date of the Banting Museum in Canada.
- It is the birthday of Sir Frederick Banting.
Getting to the Best Answer
If you are thinking about taking the certification exam, this practice test question will set you up for success. Test writers anticipate possible answers based on the details in the question. They will wave those “juicy answers” right under your nose. Your job is to weed through the particulars, pluck out the most important elements, and choose the BEST answer.
Answer 1 is incorrect. 28.42% chose this answer. “It was the date the Nobel Prize was awarded to Dr. Banting and Dr. MacLeod.” This is not the reason, however it is interesting to note that the Nobel prize for the discovery of insulin was awarded on December 10, 1923 in Stockholm, Sweden.
Answer 2 is incorrect. 27.89% of you chose this answer. “It signifies the production date of the first vial of insulin.” Great guess. However, it wasn’t until 1923 that the first vials of insulin were commercially produced and distributed.
Answer 3 is incorrect. About 4.74% of respondents chose this. “It commemorates the opening date of the Banting Museum in Canada.” The Banting House is a former residence and current museum in London, Ontario, Canada, known as the “Birthplace of Insulin.” It is the house where Sir Frederick Banting woke up at two o’clock in the morning on October 31, 1920 with the idea that led to the discovery of insulin. Since 1984, the house has been a museum dedicated to Banting’s discovery and his life.
Finally, Answer 4 is correct. 38.95% chose this answer. “It is the birthday of Sir Frederick Banting.” YES, this is the best answer. Dr. Banting was born on November 14, 1891. That is why we celebrate World Diabetes Day on November 14th.
World Diabetes Day Celebrates Dr. Banting’s Birthday and the Discovery of Insulin!
We hope you appreciate this week’s rationale! Thank you so much for taking the time to answer our Question of the Week and participate in this fun learning activity!
National Diabetes Month
.png?h=459&iar=0&w=1459&hash=E665292742D2BABAECCFA59A56B88D3C)
November kicks off National Diabetes Month, a time to recognize that over 11% of Americans are living with diabetes and over 35% have prediabetes. Since diabetes results from a combination of genetics plus environment, there is a recognition that social determinants of health play a pivotal role in the development of diabetes and its complications. Through advocacy and education, we can inform individuals on best care for diabetes and support them in taking action to improve the health of their communities to prevent future diabetes. We have put together a list of FREE diabetes resources in English and Spanish to share with people living with prediabetes and diabetes. Thank you for your advocacy and belief that we can make a difference. Coach Beverly
All hours earned count toward your CDCES Accreditation Information
Sign up for Diabetes Blog Bytes – we post one daily Blog Byte from Monday to Friday. And of course, Tuesday is our Question of the Week. It’s Informative and FREE! Sign up below!
The use of DES products does not guarantee the successful passage of the CDCES exam. CBDCE does not endorse any preparatory or review materials for the CDCES exam, except for those published by CBDCE.
Rationale of the Week | Diabetes & Demography

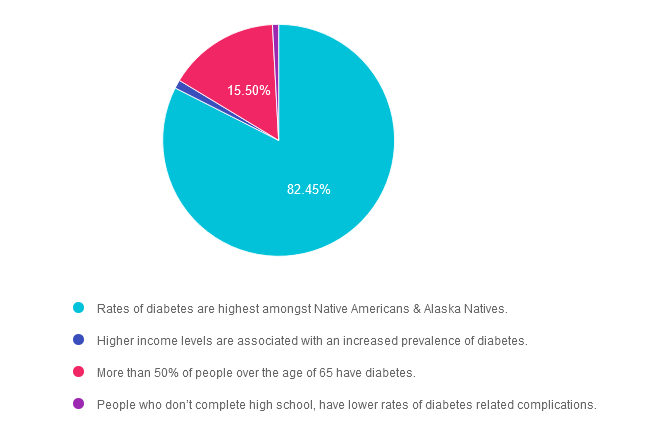
For last week’s practice question, we quizzed participants on diabetes & the impact it has on communities. 82% of respondents chose the best answer. We want to clarify and share this important information, so you can pass it on to people living with diabetes and your colleagues, plus prepare for exam success!
Before we start though, if you don’t want any spoilers and haven’t tried the question yet, you can answer it below: Answer Question
Question: November is National Diabetes Month. This month shines a spotlight on the 37 million people living with diabetes and the 96 million with prediabetes. Certain communities are hit harder with diabetes than others due to a combination of genetics and social determinants of health.
Which of the following statements are most accurate?
Answer Choices:
- Rates of diabetes are highest amongst Native Americans & Alaska Natives.
- Higher income levels are associated with an increased prevalence of diabetes.
- More than 50% of people over the age of 65 have diabetes.
- People who don’t complete high school, have lower rates of diabetes related complications.
Getting to the Best Answer
If you are thinking about taking the certification exam, this practice test question will set you up for success. Test writers anticipate possible answers based on the details in the question. They will wave those “juicy answers” right under your nose. Your job is to weed through the particulars, pluck out the most important elements and choose the BEST answer.
Answer 1 is correct. 82.45% chose this answer. “Rates of diabetes are highest amongst Native Americans & Alaska Natives.” YES, sadly, this is the best answer. For both men and women, prevalence of diagnosed diabetes was highest among American Indian and Alaska Native adults (13.6%), followed by non-Hispanic Black adults (12.1%), adults of Hispanic origin (11.7%), non-Hispanic Asian adults (9.1%) and non-Hispanic White adults (6.9%) (See CDC Appendix Table 3). As diabetes advocates, we can campaign for improved access to health care and address social determinants of health for communities at highest risk of prediabetes and diabetes.
Answer 2 is incorrect. 1.19% of you chose this answer. “Higher income levels are associated with an increased prevalence of diabetes.” People who have the lowest earnings and who don’t graduate high school have the highest rates of diabetes. Socioeconomic status and rates of diabetes are inversely related.
Answer 3 is incorrect. About 15.5% of respondents chose this. “More than 50% of people over the age of 65 have diabetes.” This is a tempting answer, but a little exaggerated. According to CDC Stats, 30% of people age 65 or live with diabetes.
Finally, Answer 4 is incorrect. 0.85% chose this answer. “People who don’t complete high school, have lower rates of diabetes related complications.” People who don’t graduate high school have the highest rates of diabetes and less resources to engage in preventive care.
We hope you appreciate this week’s rationale! Thank you so much for taking the time to answer our Question of the Week and participate in this fun learning activity!
National Diabetes Month
.png?h=459&iar=0&w=1459&hash=E665292742D2BABAECCFA59A56B88D3C)
November kicks off National Diabetes Month, a time to recognize that over 11% of Americans are living with diabetes and over 35% have prediabetes. Since diabetes results from a combination of genetics plus environment, there is a recognition that social determinants of health play a pivotal role in the development of diabetes and its complications. Through advocacy and education, we can inform individuals on best care for diabetes and support them in taking action to improve the health of their communities to prevent future diabetes. We have put together a list of FREE diabetes resources in English and Spanish to share with people living with prediabetes and diabetes. Thank you for your advocacy and belief that we can make a difference. Coach Beverly
All hours earned count toward your CDCES Accreditation Information
Sign up for Diabetes Blog Bytes – we post one daily Blog Byte from Monday to Friday. And of course, Tuesday is our Question of the Week. It’s Informative and FREE! Sign up below!
The use of DES products does not guarantee the successful passage of the CDCES exam. CBDCE does not endorse any preparatory or review materials for the CDCES exam, except for those published by CBDCE.
Rationale of the Week | What are the 5 confirmed Tongue Tastes?

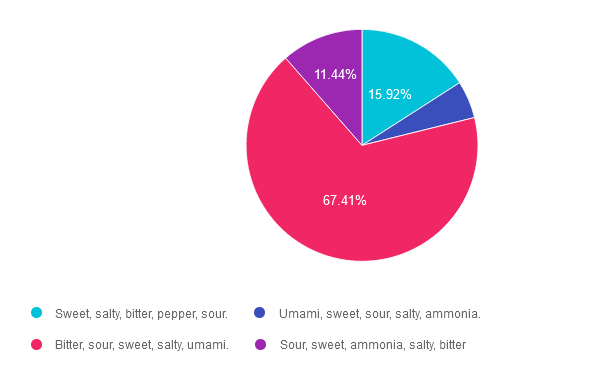
For last week’s practice question, we quizzed participants on the 5 different tongue tastes. 67% of respondents chose the best answer. We want to clarify and share this important information, so you can pass it on to people living with diabetes and your colleagues, plus prepare for exam success!
Before we start though, if you don’t want any spoilers and haven’t tried the question yet, you can answer it below: Answer Question
Question: JR thinks that their ability to taste food has diminished recently. They ask you, what are the five confirmed basic tastes of the tongue?
Which of the following lists describes the best answer?
Answer Choices:
- Sweet, salty, bitter, pepper, sour.
- Umami, sweet, sour, salty, ammonia.
- Bitter, sour, sweet, salty, umami.
- Sour, sweet, ammonia, salty, bitter
Getting to the Best Answer
If you are thinking about taking the certification exam, this practice test question will set you up for success. Test writers anticipate possible answers based on the details in the question. They will wave those “juicy answers” right under your nose. Your job is to weed through the particulars, pluck out the most important elements and choose the BEST answer.
Answer 1 is incorrect. 15.92% chose this answer. “Sweet, salty, bitter, pepper, sour.” This answer is really close, however there are no specific receptors on the tongue to detect the flavor pepper.
Answer 2 is incorrect. 5.22% of you chose this answer. “Umami, sweet, sour, salty, ammonia.” This answer is really close, however, ammonia is not a confirmed flavor and this list is missing the flavor, bitter.
Answer 3 is correct. About 67.41% of respondents chose this. “Bitter, sour, sweet, salty, umami.” YES, these are the 5 confirmed tastes and one more taste might be added to list, ammonium chloride. According to an article in Neuroscience News, “The tongue’s response to ammonium chloride, a component in some candies, may indicate a sixth basic taste. The study illuminated that OTOP1, a protein receptor that signals sour taste, also responds notably to ammonium chloride.”
Finally, Answer 4 is incorrect. 11.44% chose this answer. “Sour, sweet, ammonia, salty, bitter” This answer is really close, however, ammonia is not a confirmed flavor and this list is missing the flavor, umami.
We hope you appreciate this week’s rationale! Thank you so much for taking the time to answer our Question of the Week and participate in this fun learning activity!
Want to learn more about the GI System and Diabetes?
Exploring the GI System – From the Gut to the Butt | FREE Webinar
Now Recorded & Ready to Watch

Coach Bev invites you to join this 60 minute webinar that covers gastrointestinal health from top to bottom. Topics include; fatty liver disease diagnosis and treatment, intestinal complications associated with diabetes, keeping the microbiome healthy, and more. Join us to explore the magnificent wonders of diabetes and the gut.
Getting to the Gut Topics:
- From the Mouth to Intestines: Periodontal disease, Gastroparesis, Fatty liver disease, pancreas disorders
- Intestine as an Endocrine Organ & Bacterial Host
- NASH Treatment Options including lifestyle and pharmacotherapy
- State the relationship between gut health, microbiome and diabetes and inflammation
- Describe 3 strategies to get our microbiome back to better health.
Can’t make it live? No worries. We will send post the recorded version to the Online University within 24 hours of the broadcast
Instructor: Beverly Thomassian RN, MPH, CDCES, has been Board Certified in Advanced Diabetes Management for over 20 years. She is an Associate Clinical Professor at UCSF, a working educator, and a nationally recognized diabetes expert. She has a Master’s Degree in Public Health from UCLA, with a focus on behavioral health and education.
All hours earned count toward your CDCES Accreditation Information
Sign up for Diabetes Blog Bytes – we post one daily Blog Byte from Monday to Friday. And of course, Tuesday is our Question of the Week. It’s Informative and FREE! Sign up below!
The use of DES products does not guarantee the successful passage of the CDCES exam. CBDCE does not endorse any preparatory or review materials for the CDCES exam, except for those published by CBDCE.
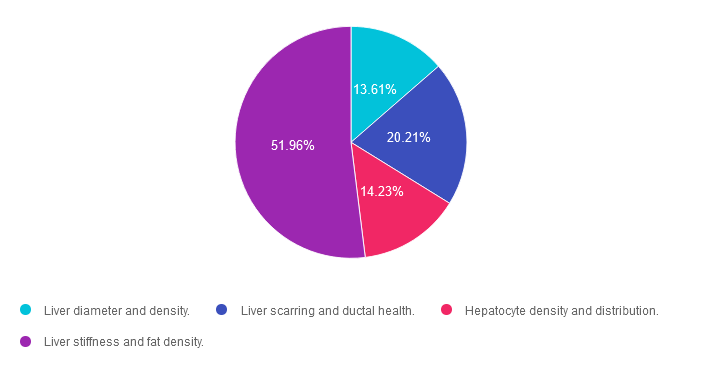
Rationale of the Week | What does a Liver Elastography Reveal?

For last week’s practice question, we quizzed participants on checking for fibrosis & liver elastography. 52% of respondents chose the best answer. We want to clarify and share this important information, so you can pass it on to people living with diabetes and your colleagues, plus prepare for exam success!
Before we start though, if you don’t want any spoilers and haven’t tried the question yet, you can answer it below: Answer Question
Question: The provider is sending JR for a Liver Elastography or FibroScan test since JR has elevated ALT and AST levels along with an elevated Fib-4 score.
Which of the following are measured during this liver ultrasound procedure?
Answer Choices:
- Liver diameter and density.
- Liver scarring and ductal health.
- Hepatocyte density and distribution.
- Liver stiffness and fat density.
Getting to the Best Answer
If you are thinking about taking the certification exam, this practice test question will set you up for success. Test writers anticipate possible answers based on the details in the question. They will wave those “juicy answers” right under your nose. Your job is to weed through the particulars, pluck out the most important elements and choose the BEST answer.
Answer 1 is incorrect. 13.61% chose this answer. “Liver diameter and density.” This answer is tempting, but unfortunately, it is not accurate. Liver Elastography or FibroScan test measures for liver stiffness and fat density, two very important findings to quantify liver health.
Answer 2 is incorrect. 20.21% of you chose this answer. “Liver scarring and ductal health.” This answer is also tempting, but not accurate. Liver Elastography or FibroScan test measures for liver stiffness and fat density, two very important findings to quantify liver health.
Answer 3 is incorrect. About 14.23% of respondents chose this. “Hepatocyte density and distribution.” Unfortunately, this tempting answer is not accurate. Liver Elastography or FibroScan test measures for liver stiffness and fat density, two very important findings to quantify liver health.
Finally, Answer 4 is correct. 51.96% chose this answer. “Liver stiffness and fat density.” YES, this is the BEST Answer. This 5-10 minute, non-invasive test, measures liver stiffness or degree of fibrosis (reported as the kPa score) and the amount of fat in the liver (reported as the CAP score). Join our FREE Webinar on Exploring the GI System – From the Gut to the Butt on November 16th to learn more!
We hope you appreciate this week’s rationale! Thank you so much for taking the time to answer our Question of the Week and participate in this fun learning activity!
Want to learn more about the GI System and Diabetes?
Exploring the GI System – From the Gut to the Butt | FREE Webinar
Now Recorded & Ready to Watch

Coach Bev invites you to join this 60 minute webinar that covers gastrointestinal health from top to bottom. Topics include; fatty liver disease diagnosis and treatment, intestinal complications associated with diabetes, keeping the microbiome healthy, and more. Join us to explore the magnificent wonders of diabetes and the gut.
Getting to the Gut Topics:
- From the Mouth to Intestines: Periodontal disease, Gastroparesis, Fatty liver disease, pancreas disorders
- Intestine as an Endocrine Organ & Bacterial Host
- NASH Treatment Options including lifestyle and pharmacotherapy
- State the relationship between gut health, microbiome and diabetes and inflammation
- Describe 3 strategies to get our microbiome back to better health.
Can’t make it live? No worries. We will send post the recorded version to the Online University within 24 hours of the broadcast
Instructor: Beverly Thomassian RN, MPH, CDCES, has been Board Certified in Advanced Diabetes Management for over 20 years. She is an Associate Clinical Professor at UCSF, a working educator, and a nationally recognized diabetes expert. She has a Master’s Degree in Public Health from UCLA, with a focus on behavioral health and education.
All hours earned count toward your CDCES Accreditation Information
Sign up for Diabetes Blog Bytes – we post one daily Blog Byte from Monday to Friday. And of course, Tuesday is our Question of the Week. It’s Informative and FREE! Sign up below!
The use of DES products does not guarantee the successful passage of the CDCES exam. CBDCE does not endorse any preparatory or review materials for the CDCES exam, except for those published by CBDCE.
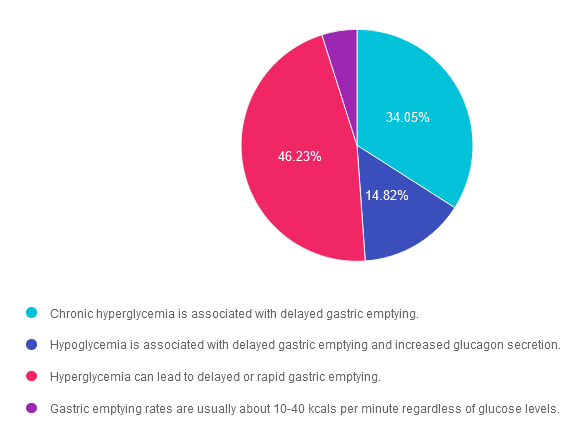
Rationale of the Week | Do glucose levels impact gastric emptying?

For last week’s practice question, we quizzed participants on how glucose levels impact gastric emptying. 46% of respondents chose the best answer. We want to clarify and share this important information, so you can pass it on to people living with diabetes and your colleagues, plus prepare for exam success!
Before we start though, if you don’t want any spoilers and haven’t tried the question yet, you can answer it below: Answer Question
Question:
Glucose fluctuations can impact gastric emptying rates.
Which of the following is the MOST accurate statement that describes the impact of glucose levels on gastric emptying rates?
Answer Choices:
- Chronic hyperglycemia is associated with delayed gastric emptying.
- Hypoglycemia is associated with delayed gastric emptying and increased glucagon secretion.
- Hyperglycemia can lead to delayed or rapid gastric emptying.
- Gastric emptying rates are usually about 10-40 kcals per minute regardless of glucose levels.
Getting to the Best Answer
If you are thinking about taking the certification exam, this practice test question will set you up for success. Test writers anticipate possible answers based on the details in the question. They will wave those “juicy answers” right under your nose. Your job is to weed through the particulars, pluck out the most important elements and choose the BEST answer.
Answer 1 is incorrect. 34.05% chose this answer. “Chronic hyperglycemia is associated with delayed gastric emptying.” This tempting answer implies that chronic hyperglycemia only causes delayed gastric emptying. However, more recent data suggests that acute and chronic hyperglycemia can also cause faster gastric emptying, resulting in post meal hyperglycemia and increased hunger.
Answer 2 is incorrect. 14.82% of you chose this answer. “Hypoglycemia is associated with delayed gastric emptying and increased glucagon secretion.” This answer has elements of accuracy. If someone injects bolus insulin before eating a meal, and they have gastroparesis, this can result in post meal hypoglycemia due to a mismatch of insulin action and carbohydrate absorption. The second part of the answer is inaccurate, since increased glucagon secretion is associated with hyperglycemia.
Answer 3 is correct. About 46.23% of respondents chose this. “Hyperglycemia can lead to delayed or rapid gastric emptying.” YES, great job. Acute and chronic hyperglycemia can wreak havoc on stomach emptying, causing either delayed or expediated bolus propulsion to the duodenum.
Finally, Answer 4 is incorrect. 4.9% chose this answer. “Gastric emptying rates are usually about 10-40 kcals per minute regardless of glucose levels.” This answer sounds accurate, but gastric emptying rates are approximately 1-4 Kcals per minute.
We hope you appreciate this week’s rationale! Thank you so much for taking the time to answer our Question of the Week and participate in this fun learning activity!
A helpful research article recommended by Coach Beverly that expounds upon this topic:
Want to learn more about the GI System and Diabetes?
Exploring the GI System – From the Gut to the Butt | FREE Webinar
Now Recorded & Ready to Watch

Coach Bev invites you to join this 60 minute webinar that covers gastrointestinal health from top to bottom. Topics include; fatty liver disease diagnosis and treatment, intestinal complications associated with diabetes, keeping the microbiome healthy, and more. Join us to explore the magnificent wonders of diabetes and the gut.
Getting to the Gut Topics:
- From the Mouth to Intestines: Periodontal disease, Gastroparesis, Fatty liver disease, pancreas disorders
- Intestine as an Endocrine Organ & Bacterial Host
- NASH Treatment Options including lifestyle and pharmacotherapy
- State the relationship between gut health, microbiome and diabetes and inflammation
- Describe 3 strategies to get our microbiome back to better health.
Can’t make it live? No worries. We will send post the recorded version to the Online University within 24 hours of the broadcast
Instructor: Beverly Thomassian RN, MPH, CDCES, has been Board Certified in Advanced Diabetes Management for over 20 years. She is an Associate Clinical Professor at UCSF, a working educator, and a nationally recognized diabetes expert. She has a Master’s Degree in Public Health from UCLA, with a focus on behavioral health and education.
All hours earned count toward your CDCES Accreditation Information
Sign up for Diabetes Blog Bytes – we post one daily Blog Byte from Monday to Friday. And of course, Tuesday is our Question of the Week. It’s Informative and FREE! Sign up below!
The use of DES products does not guarantee the successful passage of the CDCES exam. CBDCE does not endorse any preparatory or review materials for the CDCES exam, except for those published by CBDCE.