Rationale of the Week | How Can TR Improve Time in Range?

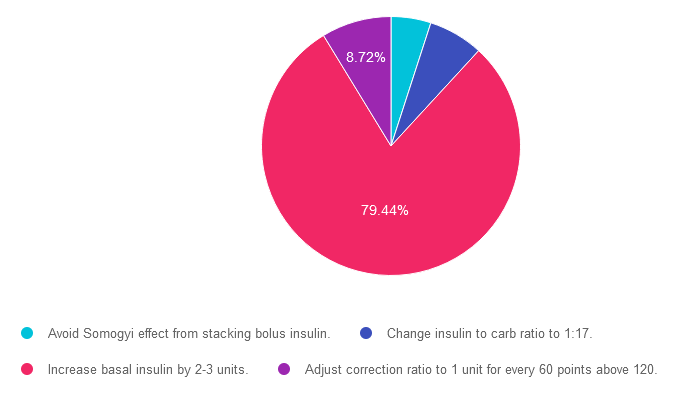
For last week’s practice question, we review how to help improve time in range. 79% of respondents chose the best answer which is awesome. We want to clarify and share this important information, so you can pass it on to people living with diabetes and your colleagues, plus prepare for exam success!
Before we start though, if you don’t want any spoilers and haven’t tried the question yet, you can answer it below: Answer Question
Question: TR is 25 and has new type 1 diabetes and is hoping to get on an insulin pump soon. TR weighs 70 kgs and takes 8 units basal insulin at bedtime, plus takes 1 unit bolus insulin for every 15 gms of carbohydrate and their correction for hyperglycemia is 1 unit for every 50 points above 120. When looking at TR’s ambulatory glucose profile, their time in range is 32% with 67% above range and about ~1% below range. Glucose levels tend to increase starting with dinner at 5pm and stay elevated throughout the night.
Based on this information, what change(s) could help improve time in range?
Answer Choices:
- Avoid Somogyi effect from stacking bolus insulin.
- Change insulin to carb ratio to 1:17.
- Increase basal insulin by 2-3 units.
- Adjust correction ratio to 1 unit for every 60 points above 120.
Getting to the Best Answer
If you are thinking about taking the certification exam, this practice test question will set you up for success. Test writers anticipate possible answers based on the details in the question. They will wave those “juicy answers” right under your nose. Your job is to weed through the particulars, pluck out the most important elements and choose the BEST answer.
Answer 1 is incorrect. 4.98% chose this answer. “Avoid Somogyi effect from stacking bolus insulin.” Somogyi is when blood sugars drop and the counter-regulatory system releases hormones that can dramatically increase blood sugar levels (sometimes referred to as rebound hyperglycemia). Since TR’s glucose levels tend to increase starting with dinner at 5pm and stay elevated throughout the night, they are not experiencing the hypoglycemia associated with the Somogyi effect.
Answer 2 is incorrect. 6.85% of you chose this answer. “Change insulin to carb ratio to 1:17.” Since TR’s glucose levels tend to increase starting with dinner at 5pm and stay elevated throughout the night, this is not due to post meal hyperglycemia. Overnight hyperglycemia is usually connected to inadequate basal insulin dosing.
Answer 3 is correct. About 79.44% of respondents chose this. “Increase basal insulin by 2-3 units.” YES, GREAT JOB! Since TR’s glucose levels tend to increase starting with dinner at 5pm and stay elevated throughout the night, this is an indication that TR has inadequate basal insulin dosing.
Finally, Answer 4 is incorrect. 8.72% chose this answer. “Adjust correction ratio to 1 unit for every 60 points above 120.” Since TR’s glucose levels tend to increase starting with dinner at 5pm and stay elevated throughout the night, this is not due to post meal hyperglycemia or inadequate bolus insulin correction coverage. Overnight hyperglycemia is usually connected to inadequate basal insulin dosing.
We hope you appreciate this week’s rationale! Thank you so much for taking the time to answer our Question of the Week and participate in this fun learning activity!
Want to learn more about this question?
NEW: Diabetes Technology Data Toolkit: Hands-on Data Interpretation Workshop with Dr. Diana Isaacs
Join Diana Isaacs live on August 30th, 2023, at 11:30 am PST
As diabetes technology is becoming commonplace in our practice, figuring out how to make sense of all the data can seem overwhelming. Dr. Isaacs has a special knack for breaking down the essential elements of the Ambulatory Glucose Profile (AGP) and other reports to provide participants with a clear road map for data interpretation. She includes tons of sample practice cases utilizing CGM, connected pens, and insulin pumps.
By attending this interactive workshop, participants will become more confident in interpreting the AGP and continuous glucose monitor (CGM) data and determining needed medication and lifestyle adjustments.
Topics include:
- Learn how to review the ambulatory glucose profile (AGP) report systematically and efficiently.
- Understand the key metrics of CGM Data and person-centered goals.
- Utilize CGM and connected data to make medication adjustments and lifestyle/behavior recommendations.
- Apply data interpretation principles to a wide variety of cases in people with type 1 and type 2 diabetes.
Instructor: Diana Isaacs, PharmD, BCPS, BCACP, CDCES, BC-ADM, FADCES, FCCPCES, was awarded ADCES Diabetes Care and Educational Specialist of the Year for her educational platform promoting the use of CGM for people with diabetes and other innovations. She is the Director of Education & Training in Diabetes Technology at the Cleveland Clinic. She has numerous diabetes publications and research projects focusing on medications, CGM, and diabetes technology. You won’t want to miss this hands-on workshop with an international expert in the field.
All hours earned count toward your CDCES Accreditation Information
Sign up for Diabetes Blog Bytes – we post one daily Blog Byte from Monday to Friday. And of course, Tuesday is our Question of the Week. It’s Informative and FREE! Sign up below!
The use of DES products does not guarantee the successful passage of the CDCES exam. CBDCE does not endorse any preparatory or review materials for the CDCES exam, except for those published by CBDCE.
Rationale of the Week | Hypoglycemia Before Meal; Best Approach?

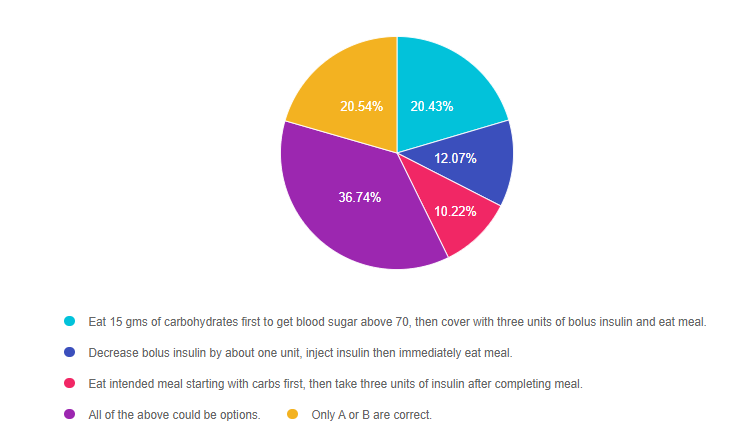
For last week’s practice question, we quizzed participants on Hypoglycemia before meals. 37% of respondents chose the best answer. We want to clarify and share this important information, so you can pass it on to people living with diabetes and your colleagues, plus prepare for exam success!
Before we start though, if you don’t want any spoilers and haven’t tried the question yet, you can answer it below: Answer Question
Question: JR has type 1 diabetes and is worried how to best adjust insulin to address hypoglycemia and prevent future episodes. They tell you that their blood sugar yesterday before lunch was 67 mg/dL and they were getting ready to eat 45 gms of carb and cover with 3 units of insulin.
JR asks, what is the best strategy in this situation? What action do you advise JR to take?
Answer Choices:
- Eat 15 gms of carbohydrates first to get blood sugar above 70, then cover with three units of bolus insulin and eat meal.
- Decrease bolus insulin by about one unit, inject insulin then immediately eat meal.
- Eat intended meal starting with carbs first, then take three units of insulin after completing meal.
- All of the above could be options.
- Only A or B are correct.
Getting to the Best Answer
If you are thinking about taking the certification exam, this practice test question will set you up for success. Test writers anticipate possible answers based on the details in the question. They will wave those “juicy answers” right under your nose. Your job is to weed through the particulars, pluck out the most important elements and choose the BEST answer.
Answer 1 is incorrect. 20.43% chose this answer. “Eat 15 gms of carbohydrates first to get blood sugar above 70, then cover with three units of bolus insulin and eat meal.” This standard intervention, often referred to as the “rule of 15”, is a safe approach that is certainly a correct option.
Answer 2 is incorrect. 12.07% of you chose this answer. “Decrease bolus insulin by about one unit, inject insulin then immediately eat meal.” This standard intervention is also a safe approach that is certainly a correct option.
Answer 3 is incorrect. About 10.22% of respondents chose this. “Eat intended meal starting with carbs first, then take three units of insulin after completing meal.” This creative intervention is certainly a viable option that JR could choose.
Answer 4 is correct. 36.74% chose this answer. “All of the above could be options.” YES, this is the BEST answer. People with type 1 diabetes can use a variety of approaches to address and treat hypoglycemia. As diabetes care and education coaches, we take a person-centered approach, leaning into the individual’s expertise. If an approach is safe and fits into JR’s lifestyle and comfort zone, we are going to support their decision. We also keep the door open to reviewing the impact of the approach and engaging in collaborative problem solving as needed.
Finally, Answer 5 is incorrect 20.54% of you chose this answer. “Only A or B are correct.” Not quite the best answer since people with type 1 diabetes can use a variety of approaches to address and treat hypoglycemia. As diabetes care and education coaches, we take a person-centered approach, leaning into the individual’s expertise. If an approach is safe and fits into JR’s lifestyle and comfort zone, we are going to support their decision. We also keep the door open to reviewing the impact of the approach and engaging in collaborative problem solving as needed. That is why the answer choice “C” could also be correct. JR might be most comfortable with taking the insulin after the meal to avoid another hypoglycemic event.
We hope you appreciate this week’s rationale! Thank you so much for taking the time to answer our Question of the Week and participate in this fun learning activity!
Want to learn more about this practice question?
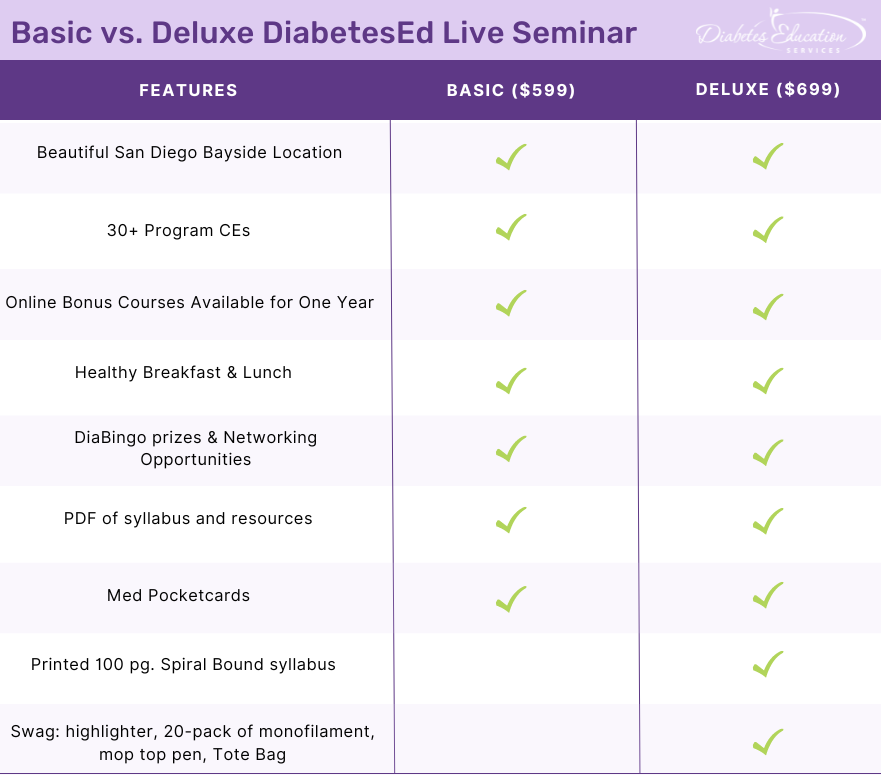
Join us LIVE in San Diego for our DiabetesEd Training Conference
October 11-13th, 2023

Two Registration Options
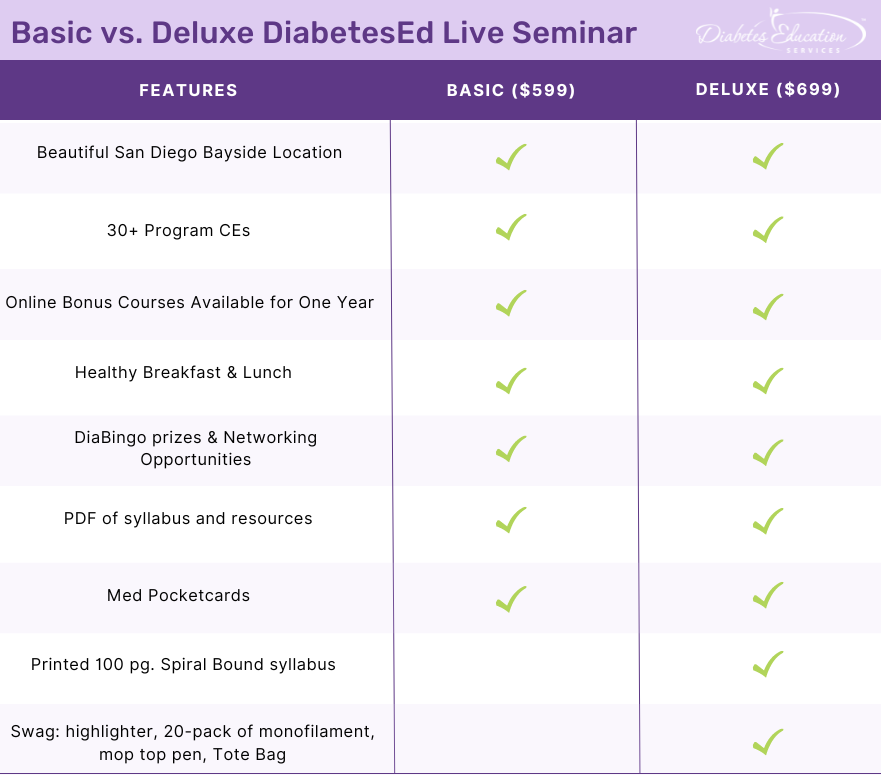
Join Coach Beverly and Team for two and a half days of knowledge-sharing, fun, networking, games with prizes, and “aha” moments in beautiful San Diego.
You don’t want to miss this one-of-a-kind learning opportunity. Get away from all those daily responsibilities and immerse yourself in a fun and intensive conference with plenty of networking opportunities.
Attendees will leave this conference with new tools and a more complete understanding of the latest advances in diabetes care, from medications to technology to Medical Nutrition Therapy!
Bring your colleagues and enjoy our friend discount.
Our team expertly translates the complex science of diabetes into understandable terms while keeping it real, practical, and fun.
Team of expert faculty includes:
- Diana Isaacs, PharmD, BCPS, BC-ADM, BCACP, CDCES – Educator of the Year, 2020
- Coach Beverly Thomassian, RN, MPH, CDCES, BC-ADM
- Ashley LaBrier, MS, RD, CDCES, Diabetes Program Coordinator
All hours earned count toward your CDCES Accreditation Information
Sign up for Diabetes Blog Bytes – we post one daily Blog Byte from Monday to Friday. And of course, Tuesday is our Question of the Week. It’s Informative and FREE! Sign up below!
The use of DES products does not guarantee the successful passage of the CDCES exam. CBDCE does not endorse any preparatory or review materials for the CDCES exam, except for those published by CBDCE.
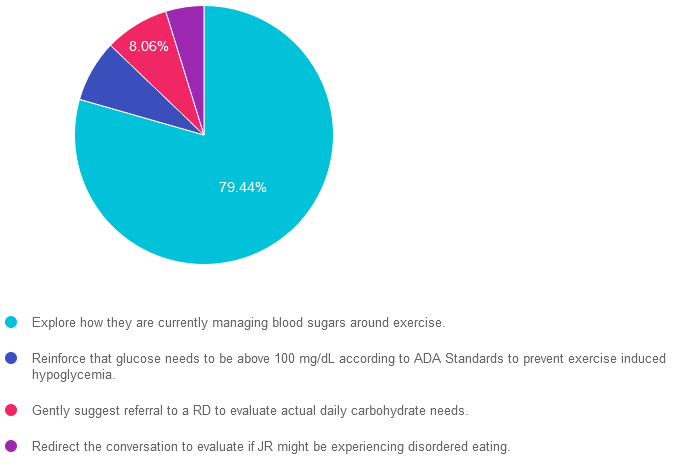
Rationale of the Week | Preventing Hypo During Exercise

For last week’s practice question, we quizzed participants on Hypoglycemia during exercise. 79% of respondents chose the best answer. We want to clarify and share this important information, so you can pass it on to people living with diabetes and your colleagues, plus prepare for exam success!
Before we start though, if you don’t want any spoilers and haven’t tried the question yet, you can answer it below: Answer Question
Question: JR has type 1 and tells you they limit their carbohydrate intake to 30 gms a day to prevent hyperglycemia. Their A1C is 6.7% and time in range is over 70%. They tell you their main goal is to figure out how to prevent hypoglycemia during exercise.
What would be the best response using a person-centered approach?
Answer Choices:
- Explore how they are currently managing blood sugars around exercise.
- Reinforce that glucose needs to be above 100 mg/dL according to ADA Standards to prevent exercise induced hypoglycemia.
- Gently suggest referral to a RD to evaluate actual daily carbohydrate needs.
- Redirect the conversation to evaluate if JR might be experiencing disordered eating.
Getting to the Best Answer
If you are thinking about taking the certification exam, this practice test question will set you up for success. Test writers anticipate possible answers based on the details in the question. They will wave those “juicy answers” right under your nose. Your job is to weed through the particulars, pluck out the most important elements and choose the BEST answer.
Answer 1 is correct]. 79.44% chose this answer. “Explore how they are currently managing blood sugars around exercise.” YES, GREAT JOB! Since this response is person centered and respectful of JR’s desire to learn how to prevent hypoglycemia, it is the best answer. Sometimes, we might be tempted to focus on a different goal than what the individual is requesting. However, by addressing their priorities FIRST, we build trust and create meaningful connections.
Answer 2 is incorrect. 7.73% of you chose this answer. “Reinforce that glucose needs to be above 100 mg/dL according to ADA Standards to prevent exercise induced hypoglycemia.” This answer doesn’t allow for exploration, personalization and customization. A glucose goal of “above 100” pre-exercise does not fit for everyone. People with type 1 diabetes often feel more comfortable with a blood sugar 180 mg/dL or greater before engaging in activity to prevent hypoglycemia from glucose expenditure during exercise.
Answer 3 is incorrect. About 8.06% of respondents chose this. “Gently suggest referral to a RD to evaluate actual daily carbohydrate needs.” Although, JR is limiting his intake to 30gms carb a day, they have stated that they want to work on preventing exercise related hypoglycemia. Sometimes, we might be tempted to focus on a different goal than what the individual is requesting. However, by addressing their priorities FIRST, we build trust and create meaningful connections.
Finally, Answer 4 is incorrect. 4.77% chose this answer. “Redirect the conversation to evaluate if JR might be experiencing disordered eating.” Although, JR is limiting his intake to 30gms carb a day, they have stated that they want to work on preventing exercise related hypoglycemia. Sometimes, we might be tempted to focus on a different goal than what the individual is requesting. However, by addressing their priorities FIRST, we build trust and create opportunities to explore other topics in the future.
We hope you appreciate this week’s rationale! Thank you so much for taking the time to answer our Question of the Week and participate in this fun learning activity!
Want to learn more about this question?
ReVive 5 Diabetes Training Program
“ReVive 5 Program is the best program I have ever attended – should be required for all diabetes educators! Thank you so much for translating this research into practical approaches!!” – Sarah F.
Save $100! Enroll now to watch the webinar on-demand

ReViVE 5 Diabetes Training Program:
Unlocking Hidden Barriers to Diabetes Management
Enroll Now and Save $100!
Recorded & Ready to Watch
Addressing diabetes distress can be tricky, even for seasoned healthcare professionals.
We invite you to attend this hands-on training program that provides the essential steps to address diabetes distress combined with an innovative approach to glucose management. Our experts offer realistic strategies to address diabetes distress that you can immediately apply to your practice setting. Plus, the ReVive 5 Program provides a breadth of tools and resources to create more meaningful connections with people with diabetes.
Team of Experts: ReVive 5 is taught by a team of 3 Interdisciplinary Experts:
- Lawrence Fisher, Ph.D., ABPP, Professor Emeritus, UCSF
- Susan Guzman, PhD
- Beverly Thomassian, RN, MPH, CDCES, BC-ADM
Accredited Training Program:
- 15.0 CEs – Includes the 7-hour ReVive 5 Training Program, Certificate, and 5 FREE bonus courses to supplement content.
- A comprehensive set of assessment tools, educational materials, log sheets, and resources.
“ReVive 5” breathes new life into our relationship with diabetes, bringing a fresh perspective to both the person with diabetes and the provider.
All hours earned count toward your CDCES Accreditation Information
Sign up for Diabetes Blog Bytes – we post one daily Blog Byte from Monday to Friday. And of course, Tuesday is our Question of the Week. It’s Informative and FREE! Sign up below!
The use of DES products does not guarantee the successful passage of the CDCES exam. CBDCE does not endorse any preparatory or review materials for the CDCES exam, except for those published by CBDCE.
Rationale of the Week | Post-Meal Hypoglycemia

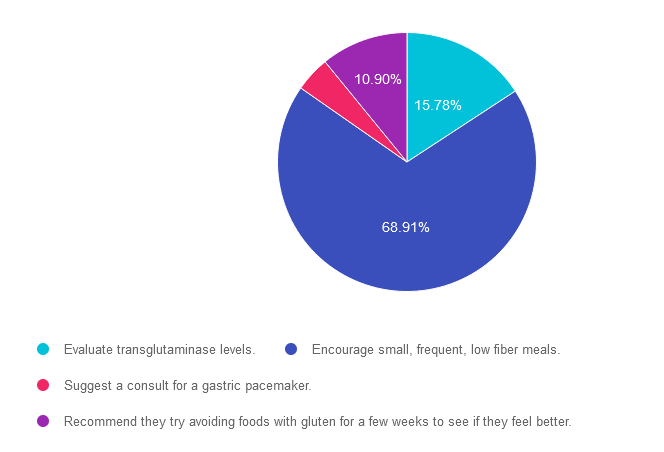
For last week’s practice question, we quizzed participants on post-meal hypoglycemia. 69% of respondents chose the best answer. We want to clarify and share this important information, so you can pass it on to people living with diabetes and your colleagues, plus prepare for exam success!
Before we start though, if you don’t want any spoilers and haven’t tried the question yet, you can answer it below: Answer Question
Question:
JR has lived with type 1 diabetes for over 30 years and has been complaining that they feel full and bloated after eating and experiencing more post-meal hypoglycemia.
Based on this information, what is the most appropriate recommendation for JR?
Answer Choices:
- Evaluate transglutaminase levels.
- Encourage small, frequent, low fiber meals.
- Suggest a consult for a gastric pacemaker.
- Recommend they try avoiding foods with gluten for a few weeks to see if they feel better.
Getting to the Best Answer
If you are thinking about taking the certification exam, this practice test question will set you up for success. Test writers anticipate possible answers based on the details in the question. They will wave those “juicy answers” right under your nose. Your job is to weed through the particulars, pluck out the most important elements and choose the BEST answer.
Answer 1 is incorrect. 15.78% chose this answer. “Evaluate transglutaminase levels.” Based on JR’s symptoms of “feeling full and bloated after eating and experiencing more post-meal hypoglycemia” we are not suspecting celiac disease since there is no mention of bloating after gluten rich foods. Plus, post meal hypoglycemia is more likely associated with the delayed gastric emptying associated with gastroparesis. Since transglutaminase is a test used to detect celiac disease, this is not the best answer.
Answer 2 is correct. 68.91% of you chose this answer. “Encourage small, frequent, low fiber meals.” YES. GREAT JOB! JR’s symptoms of “feeling full and bloated after eating and experiencing more post-meal hypoglycemia” are both classic symptoms of gastroparesis and delayed gastric emptying. This autonomic neuropathic condition is treated with glucose improvement and smaller, low fiber meals to support gastric movement. In addition, a referral to a GI specialist is certainly warranted.
Answer 3 is incorrect. About 4.41% of respondents chose this. “Suggest a consult for a gastric pacemaker.” JR’s symptoms of “feeling full and bloated after eating and experiencing more post-meal hypoglycemia” are both classic symptoms of gastroparesis and delayed gastric emptying. This autonomic neuropathic condition is treated with glucose improvement and smaller, low fiber meals to support gastric movement. However, before suggesting a consult for a gastric pacemaker, JR would first need a referral to a GI specialist to confirm diagnosis and evaluate best next steps.
Finally, Answer 4 is incorrect. 10.90% chose this answer. “Recommend they try avoiding foods with gluten for a few weeks to see if they feel better.” Based on JR’s symptoms of “feeling full and bloated after eating and experiencing more post-meal hypoglycemia” we are not suspecting celiac disease since there is no mention of bloating after gluten rich foods. Plus, post meal hypoglycemia is more likely associated with the delayed gastric emptying associated with gastroparesis.
We hope you appreciate this week’s rationale! Thank you so much for taking the time to answer our Question of the Week and participate in this fun learning activity!
Want to learn more about this practice question?
Join us LIVE in San Diego for our DiabetesEd Training Conference
October 11-13th, 2023

Two Registration Options
Join Coach Beverly and Team for two and a half days of knowledge-sharing, fun, networking, games with prizes, and “aha” moments in beautiful San Diego.
You don’t want to miss this one-of-a-kind learning opportunity. Get away from all those daily responsibilities and immerse yourself in a fun and intensive conference with plenty of networking opportunities.
Attendees will leave this conference with new tools and a more complete understanding of the latest advances in diabetes care, from medications to technology to Medical Nutrition Therapy!
Bring your colleagues and enjoy our friend discount.
Our team expertly translates the complex science of diabetes into understandable terms while keeping it real, practical, and fun.
Team of expert faculty includes:
- Diana Isaacs, PharmD, BCPS, BC-ADM, BCACP, CDCES – Educator of the Year, 2020
- Coach Beverly Thomassian, RN, MPH, CDCES, BC-ADM
- Ashley LaBrier, MS, RD, CDCES, Diabetes Program Coordinator
All hours earned count toward your CDCES Accreditation Information
Sign up for Diabetes Blog Bytes – we post one daily Blog Byte from Monday to Friday. And of course, Tuesday is our Question of the Week. It’s Informative and FREE! Sign up below!
The use of DES products does not guarantee the successful passage of the CDCES exam. CBDCE does not endorse any preparatory or review materials for the CDCES exam, except for those published by CBDCE.
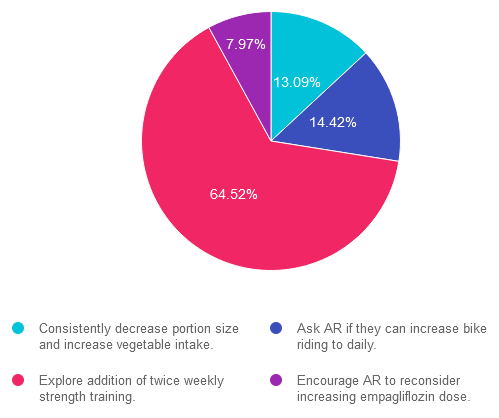
Rationale of the Week | Give me a Chance to Drop A1C

For last week’s practice question, we quizzed participants on getting A1C to goal. 65% of respondents chose the best answer. We want to clarify and share this important information, so you can pass it on to people living with diabetes and your colleagues, plus prepare for exam success!
Before we start though, if you don’t want any spoilers and haven’t tried the question yet, you can answer it below: Answer Question
Question: AR’s has an A1C of 7.5% and is taking empagliflozin (Jardiance) 10mg daily, plus trying to eat healthy and ride their bike 4-5 days a week for 30 minutes. The provider suggests increasing the empagliflozin dose to 25mg to get the A1C below 7%. AR says that they don’t want to increase their medication dose and says they are dedicated to lowering their A1C through more activity.
Based on this scenario, what ADA recommended activity addition or change would help AR reach their A1C target?
Answer Choices:
- Consistently decrease portion size and increase vegetable intake.
- Ask AR if they can increase bike riding to daily.
- Explore addition of twice weekly strength training.
- Encourage AR to reconsider increasing empagliflozin dose.
Getting to the Best Answer
If you are thinking about taking the certification exam, this practice test question will set you up for success. Test writers anticipate possible answers based on the details in the question. They will wave those “juicy answers” right under your nose. Your job is to weed through the particulars, pluck out the most important elements and choose the BEST answer.
Answer 1 is incorrect. 13.09% chose this answer. “Consistently decrease portion size and increase vegetable intake.” This juicy answer is tempting, since it addresses portion size and includes more vegetable intake. However, it is not the best answer since it doesn’t match AR’s stated goal that “they are dedicated to lowering their A1C through more activity.”
Answer 2 is incorrect. 14.42% of you chose this answer. “Ask AR if they can increase bike riding to daily.” Based on the ADA Standards, individuals are encouraged to maintain 150 minutes of activity a week, plus strengthening activities twice weekly. Asking AR to increase bike to riding to daily, is not the best approach in this scenario to achieve A1C targets.
Answer 3 is correct. About 64.52% of respondents chose this. “Explore addition of twice weekly strength training.” YES, this is the best answer. Based on the ADA Standards, individuals are encouraged to maintain 150 minutes of activity a week, plus strengthening activities twice weekly. Studies show that increasing muscle mass significantly lowers glucose and A1C.
Finally, Answer 4 is incorrect. 7.97% chose this answer. “Encourage AR to reconsider increasing empagliflozin dose.” This juicy answer is tempting, since increasing the empagliflozin dose would most likely decrease AR’s blood sugar. However, it is not the best answer since it doesn’t match AR’s stated goal that “they are dedicated to lowering their A1C through more activity.”
We hope you appreciate this week’s rationale! Thank you so much for taking the time to answer our Question of the Week and participate in this fun learning activity!.
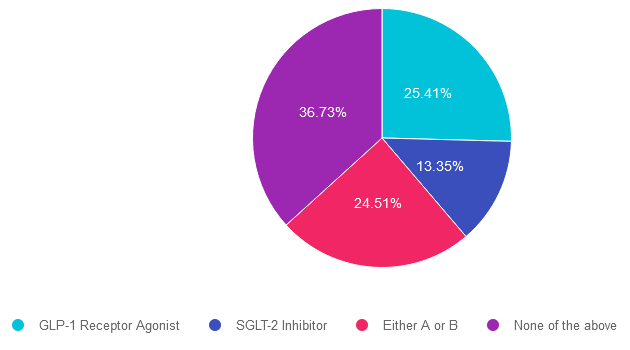
Rationale of the Week | Best Next Step for LR?

For last week’s practice question, over 1,900 participants submitted their answers for how LR could improve glucose while preparing for pregnancy. 37% of respondents chose the best answer. We want to clarify and share this important information, so you can pass it on to people living with diabetes and your colleagues, plus prepare for exam success!
Before we start though, if you don’t want any spoilers and haven’t tried the question yet, you can answer it below: Answer Question
Question: LR is 29 years old, has newly discovered diabetes and polycystic ovary syndrome (PCOS) and is trying to get pregnant. In addition to treating the diabetes and PCOS, LR would like to lose weight. LR was referred to the RD/RDN and encouraged to increase activity level. To treat PCOS and diabetes, LR was started on metformin ER 500mg BID. After a month of treatment, LR’s A1C was still above 8%.
According to ADA Standards, besides increasing the metformin dose, what additional therapy could be added to get LR’s glucose to goal?
Answer Choices:
- GLP-1 Receptor Agonist
- SGLT-2 Inhibitor
- Either A or B
- None of the above
Getting to the Best Answer
If you are thinking about taking the certification exam, this practice test question will set you up for success. Test writers anticipate possible answers based on the details in the question. They will wave those “juicy answers” right under your nose. Your job is to weed through the particulars, pluck out the most important elements and choose the BEST answer.
Answer 1 is incorrect. 25.41% chose this answer. “GLP-1 Receptor Agonist.” Given that LR has elevated blood glucose and wants to lose weight, starting a GLP-1 seems like a reasonable idea. However, GLP-1’s are not FDA approved for use during pregnancy. Since LR is trying to get pregnant, this class of medication would not be recommended.
Answer 2 is incorrect. 13.35% of you chose this answer. “SGLT-2 Inhibitor.” Given that LR has elevated blood glucose and wants to lose weight, starting a SGLT-2i seems like a reasonable idea. However, SGLT-2i’s are not FDA approved for use during pregnancy. Since LR is trying to get pregnant, this class of medication would not be recommended.
Answer 3 is incorrect. About 24.51% of respondents chose this. “Either A or B.” Given that LR has elevated blood glucose and wants to lose weight, starting either a SGLT-2i or a GLP-1 seems like a reasonable idea. However, SGLT-2i’s and GLP-1’s are not FDA approved for use during pregnancy. Since LR is trying to get pregnant, neither class of medication would not be recommended.
Finally, Answer 4 is correct. 36.73% chose this answer. “None of the above.” YES, This is the Best Answer. Metformin is the only non-insulin diabetes medication the ADA recommends for the first trimester of pregnancy. Many people with PCOS are treated with metformin to decrease insulin resistance and ovulation can resume, resulting in pregnancy. The ADA recommends stopping metformin after the first trimester and starting insulin if blood glucose levels remain above target.
We hope you appreciate this week’s rationale! Thank you so much for taking the time to answer our Question of the Week and participate in this fun learning activity!
Celebrating 25 Years Sale!!!
Save $100 on our Most Popular Online Programs! Sale ends July 31st!
Prepare for Certification and Earn CEs
ReVive 5 Diabetes Training Program
“ReVive 5 Program is the best program I have ever attended – should be required for all diabetes educators! Thank you so much for translating this research into practical approaches!!” – Sarah F.
Save $100! Enroll now to watch the webinar on-demand

Addressing diabetes distress can be challenging, even for seasoned healthcare professionals.
We invite you to attend this hands-on training program that provides the essential steps to address diabetes distress combined with an innovative approach to glucose management.
Team of Experts: ReVive 5 is taught by a team of 3 Interdisciplinary Experts:
Lawrence Fisher, Ph.D., ABPP, Professor Emeritus, UCSF
Susan Guzman, PhD
Beverly Thomassian, RN, MPH, CDCES, BC-ADM
Accredited Training Program:
- 15.0 CEs – Includes the 7-hour ReVive 5 Training Program, Certificate, and 5 FREE bonus courses to supplement content.
- A comprehensive set of assessment tools, educational materials, log sheets, and resources.
“ReVive 5” breathes new life into our relationship with diabetes, bringing a fresh perspective to both the person with diabetes and the provider.
CDCES Basic Prep Bundle
30+ Online Courses | 50+ CEs
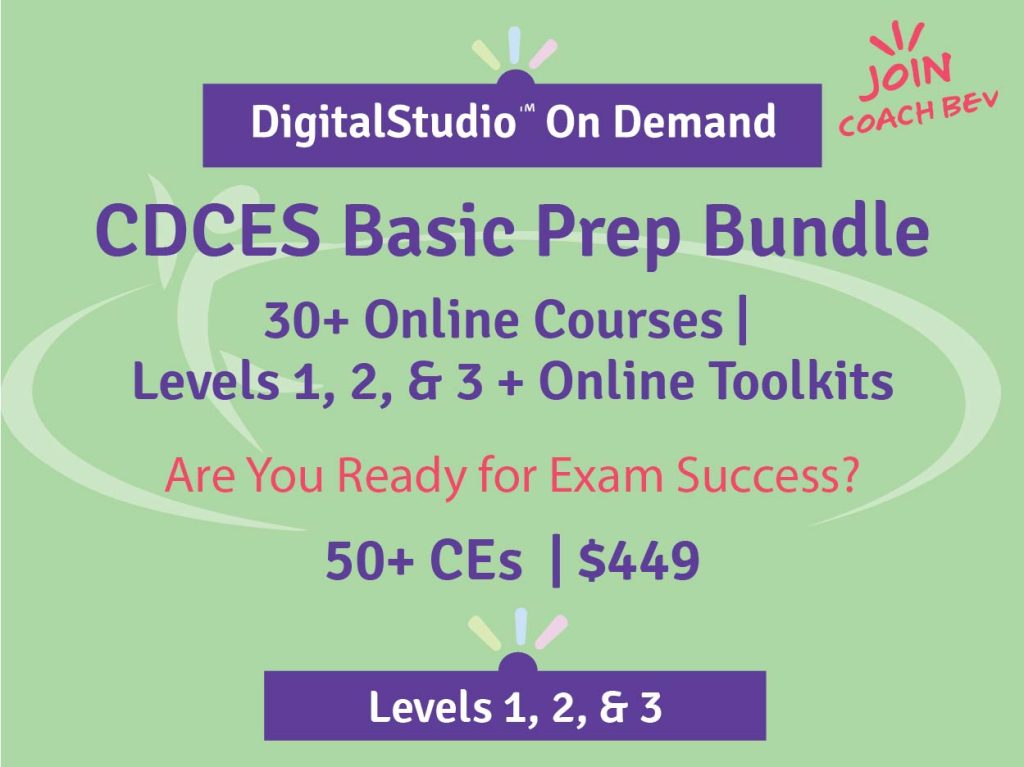
This bundle is specifically designed for healthcare professionals who are studying for the Certified Diabetes Care and Education Specialist (CDCES) exam.
The online bundle includes Level 1, Level 2, and Level 3 (Boot Camp), plus online Technology & Test-Taking Toolkits.
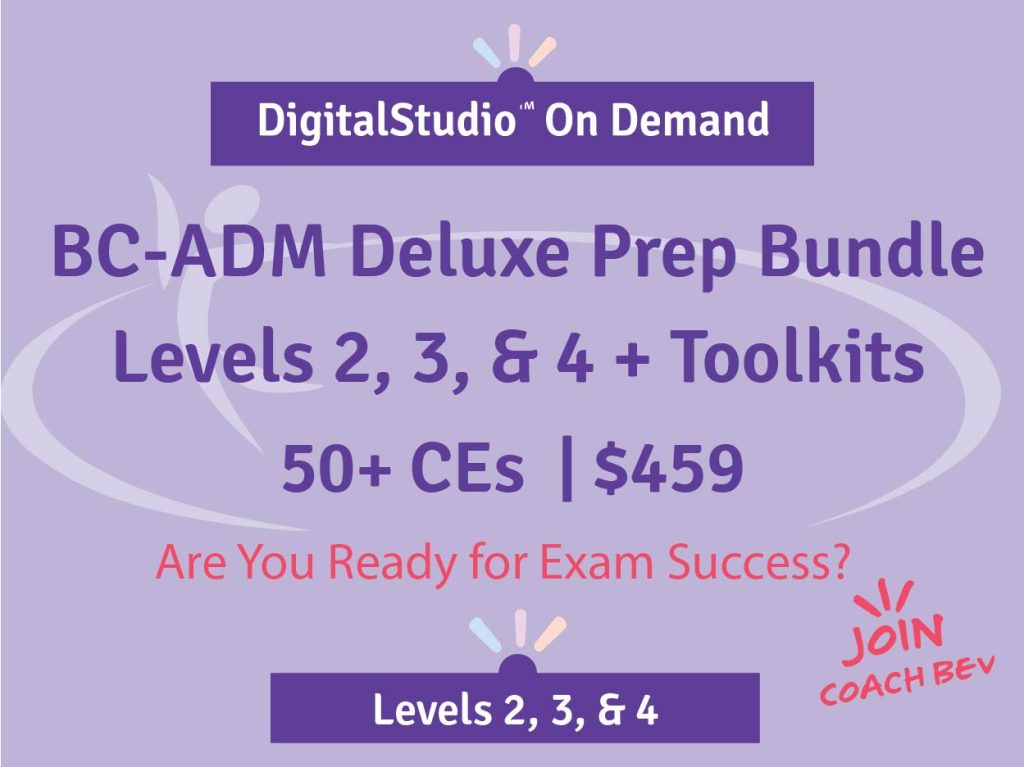
BC-ADM Deluxe Prep Bundle
35 online courses | 50+ CEs
This bundle is specifically designed for healthcare professionals who are studying for the Board Certified in Advanced Diabetes Management (BC-ADM) exam.
This bundle includes our Level 2, Level 3 (Boot Camp), and Level 4, plus online Technology & Test-Taking Toolkits.
NEW: Everything Bundle
40+ online courses | 85+ CEs
The first person who purchases our Everything Bundle wins our last copy of the Diabetes Review Guide 5th Ed.
The next edition of the Review Guide will be released in August. We will be preselling as soon as we get the thumbs up.

This exclusive Everything Bundle provides access to ALL of our Online University Courses and Training Programs. This bundle is perfect for those who need CEs to renew their license or diabetes certification or are looking for a comprehensive update on all topics of diabetes.
Subscribers enjoy over 40 courses taught by Coach Beverly and her team of experts on topics ranging from Diabetes Distress to MNT, Technology to Pattern Management with a focus on providing evidence-based, person-centered diabetes care.
The first person who purchases our Everything Bundle wins our last copy of the Diabetes Review Guide 5th Ed.
All hours earned count toward your CDCES Accreditation Information
ADCES Art & Science Desk Reference
5th Edition
The ADCES (formerly AADE) Art and Science of Diabetes Care and Education, 5th Edition is a specialist’s one-volume, go-to resource for the core knowledge and skills for providing person-centered care and education to persons with diabetes and related chronic conditions. This is a core resource for those who are studying for the Certified Diabetes Care and Education Specialist (CDCES) exam.
ADCES will be releasing an updated edition of the Art & Science Desk reference in August 2023
Sign up for Diabetes Blog Bytes – we post one daily Blog Byte from Monday to Friday. And of course, Tuesday is our Question of the Week. It’s Informative and FREE! Sign up below!
The use of DES products does not guarantee the successful passage of the CDCES exam. CBDCE does not endorse any preparatory or review materials for the CDCES exam, except for those published by CBDCE.
Rationale of the Week | What best describes Health Belief Model?

For last week’s practice question, we quizzed participants on person-centered care. 55% of respondents chose the best answer. We want to clarify and share this important information, so you can pass it on to people living with diabetes and your colleagues, plus prepare for exam success!
Before we start though, if you don’t want any spoilers and haven’t tried the question yet, you can answer it below: Answer Question
Question: MR has an A1C of 9.6% and is deciding whether or not to start another diabetes medication to help lower their glucose. MR’s parent had diabetes and severe complications due to chronic hyperglycemia.
What would best describe the application of the Health Belief Model in this situation?
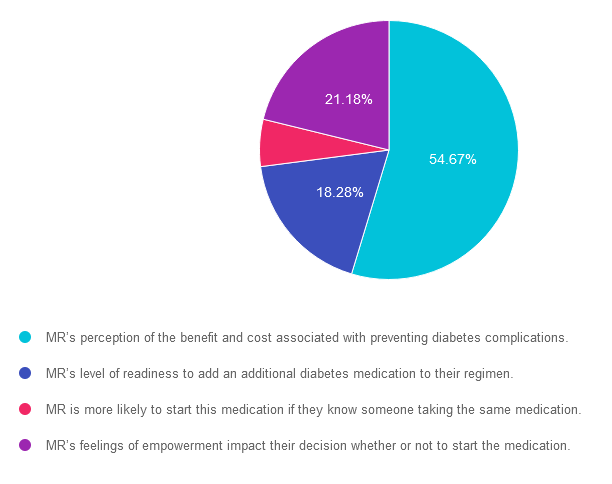
Answer Choices:
- MR’s perception of the benefit and cost associated with preventing diabetes complications.
- MR’s level of readiness to add an additional diabetes medication to their regimen.
- MR is more likely to start this medication if they know someone taking the same medication.
- MR’s feelings of empowerment impact their decision whether or not to start the medication.
Getting to the Best Answer
If you are thinking about taking the certification exam, this practice test question will set you up for success. Test writers anticipate possible answers based on the details in the question. They will wave those “juicy answers” right under your nose. Your job is to weed through the particulars, pluck out the most important elements and choose the BEST answer.
Answer 1 is correct. 54.67% chose this answer. “MR’s perception of the benefit and cost associated with preventing diabetes complications.” GREAT JOB. The Health Belief Model (HBM) focuses on individual beliefs and perceptions about health-related behavior change. It suggests that behavior change is influenced by an individual’s perception of the severity of a health problem, their susceptibility to it, the benefits of behavior change, and the barriers or cues to action. In other words it looks at the cost-benefit of a given situation.
Answer 2 is incorrect. 18.28% of you chose this answer. “MR’s level of readiness to add an additional diabetes medication to their regimen.” This answer actually refers the Stages of Change (transtheoretical) Model: This model proposes that individuals go through a series of stages when changing behavior: precontemplation, contemplation, preparation, action, and maintenance. It suggests that people move through these stages in a cyclical manner and that interventions should be tailored to each stage.
Answer 3 is incorrect. About 5.88% of respondents chose this. “MR is more likely to start this medication if they know someone taking the same medication.” This answer reflects the Social Cognitive Theory (SCT): This theory emphasizes the reciprocal interaction between personal factors (such as cognition and self-efficacy), environmental factors, and behavior. It suggests that behavior change is influenced by observing others (social modeling), self-regulation, and the belief that one can successfully perform the behavior (self-efficacy).
Finally, Answer 4 is incorrect. 21.18% chose this answer. “MR’s feelings of empowerment impact their decision whether or not to start the medication.” This answer refers to the empowerment model which is a theoretical framework that focuses on empowering individuals or communities to take control of their own lives and make informed decisions. It emphasizes the importance of promoting autonomy, self-efficacy, and participation in decision-making processes. The empowerment model is often applied in various fields, including social work, community development, healthcare, and education.
Behavior Change Theories Explained – LIVE FREE Webinar
August 23rd, @ 11:30 am PST

Learning behavior change theories and getting to the best answer for certification exams can be tricky. To say thanks for 25 years, Coach Beverly is going to host a FREE Webinar where she dissects common learning theories that are not only helpful for your clinical practice, but also for exam preparation.
Join her August 23rd at 11:30 am PT. For live webinars, Coach Beverly stays after class to answer any lingering questions you may have on the topic.
We hope you appreciate this week’s rationale! Thank you so much for taking the time to answer our Question of the Week and participate in this fun learning activity!
ReVive 5 Diabetes Training Program
“ReVive 5 Program is the best program I have ever attended – should be required for all diabetes educators! Thank you so much for translating this research into practical approaches!!” – Sarah F.
Save $100! Enroll now to watch the webinar on-demand

ReViVE 5 Diabetes Training Program:
Unlocking Hidden Barriers to Diabetes Management
Enroll Now and Save $100!
Recorded & Ready to Watch
Addressing diabetes distress can be tricky, even for seasoned healthcare professionals.
We invite you to attend this hands-on training program that provides the essential steps to address diabetes distress combined with an innovative approach to glucose management. Our experts offer realistic strategies to address diabetes distress that you can immediately apply to your practice setting. Plus, the ReVive 5 Program provides a breadth of tools and resources to create more meaningful connections with people with diabetes.
Team of Experts: ReVive 5 is taught by a team of 3 Interdisciplinary Experts:
- Lawrence Fisher, Ph.D., ABPP, Professor Emeritus, UCSF
- Susan Guzman, PhD
- Beverly Thomassian, RN, MPH, CDCES, BC-ADM
Accredited Training Program:
- 15.0 CEs – Includes the 7-hour ReVive 5 Training Program, Certificate, and 5 FREE bonus courses to supplement content.
- A comprehensive set of assessment tools, educational materials, log sheets, and resources.
“ReVive 5” breathes new life into our relationship with diabetes, bringing a fresh perspective to both the person with diabetes and the provider.
All hours earned count toward your CDCES Accreditation Information
Sign up for Diabetes Blog Bytes – we post one daily Blog Byte from Monday to Friday. And of course, Tuesday is our Question of the Week. It’s Informative and FREE! Sign up below!
The use of DES products does not guarantee the successful passage of the diabetes certification exams. CBDCE & ADCES does not endorse any preparatory or review materials for the certification exams, except for those published by CBDCE & ADCES.
Rationale of the Week | Accurate Meal Planning Approach?

For last week’s practice question, we quizzed participants on ADA recommendations for meal planning with diabetes. 41% of respondents chose the best answer. We want to clarify and share this important information, so you can pass it on to people living with diabetes and your colleagues, plus prepare for exam success!
Before we start though, if you don’t want any spoilers and haven’t tried the question yet, you can answer it below: Answer Question
Question: Which of the following diabetes meal planning recommendations is accurate according to ADA Standards of Care?
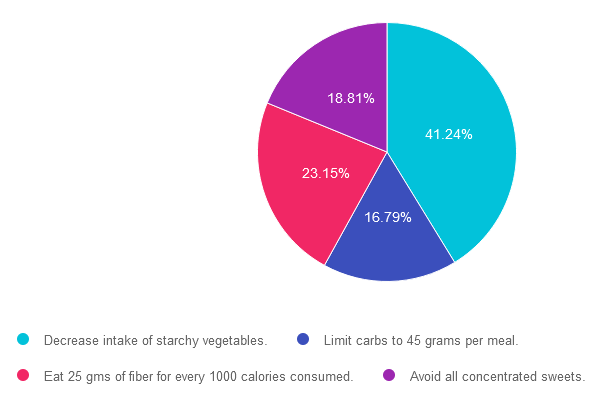
Answer Choices:
- Decrease intake of starchy vegetables.
- Limit carbs to 45 grams per meal.
- Eat 25 gms of fiber for every 1000 calories consumed.
- Avoid all concentrated sweets.
Getting to the Best Answer
If you are thinking about taking the certification exam, this practice test question will set you up for success. Test writers anticipate possible answers based on the details in the question. They will wave those “juicy answers” right under your nose. Your job is to weed through the particulars, pluck out the most important elements and choose the BEST answer.
Answer 1 is correct. 41.24% chose this answer. “Decrease intake of starchy vegetables.” YES, this is the BEST answer. According to ADA Standard 5, “Reducing overall carbohydrate intake for individuals with diabetes has demonstrated evidence for improving glycemia and may be applied in a variety of eating patterns that meet individual needs and preferences. Eating plans should emphasize nonstarchy vegetables, fruits, legumes, and whole grains, as well as dairy products, with minimal added sugars. However, “macronutrient distribution should be based on an individualized assessment of current eating patterns, preferences, and metabolic goals.”
Answer 2 is incorrect. 16.79% of you chose this answer. “Limit carbs to 45 grams per meal.” This is a juicy answer, but is an older approach that is no longer recommended. According to ADA Standard 5, “Evidence suggests that there is not an ideal percentage of calories from carbohydrate, protein, and fat for people with diabetes. However, macronutrient distribution should be based on an individualized assessment of current eating patterns, preferences, and metabolic goals.”
Answer 3 is incorrect. About 23.15% of respondents chose this. “Eat 25 gms of fiber for every 1000 calories consumed.” WOW, that would be a LOT of fiber. This is a great number to know for certification exams. According to ADA Standard 5, “People with diabetes and those at risk for diabetes are encouraged to consume a minimum of 14 g of fiber/1,000 kcal, with at least half of grain consumption being whole, intact grains, according to the Dietary Guidelines for Americans.”
Finally, Answer 4 is incorrect. 18.81% chose this answer. “Avoid all concentrated sweets.” Even if you are not sure what the best answer is at first, this answer has two red flags, the word “avoid” and the word “all”. Since the ADA recommends flexibility and tailoring to the individual, this would not be the best person-centered answer. According to ADA Standard 5, “Dietary guidance should emphasize the importance of a healthy dietary pattern as a whole rather than focusing on individual nutrients, foods, or food groups, given that individuals rarely eat foods in isolation.”
We hope you appreciate this week’s rationale! For more info on ADA Standard 5, click here. Thank you so much for taking the time to answer our Question of the Week and participate in this fun learning activity!
Want to learn more about this practice question?
Join us LIVE in San Diego for our DiabetesEd Training Conference
October 11-13th, 2023

Two Registration Options
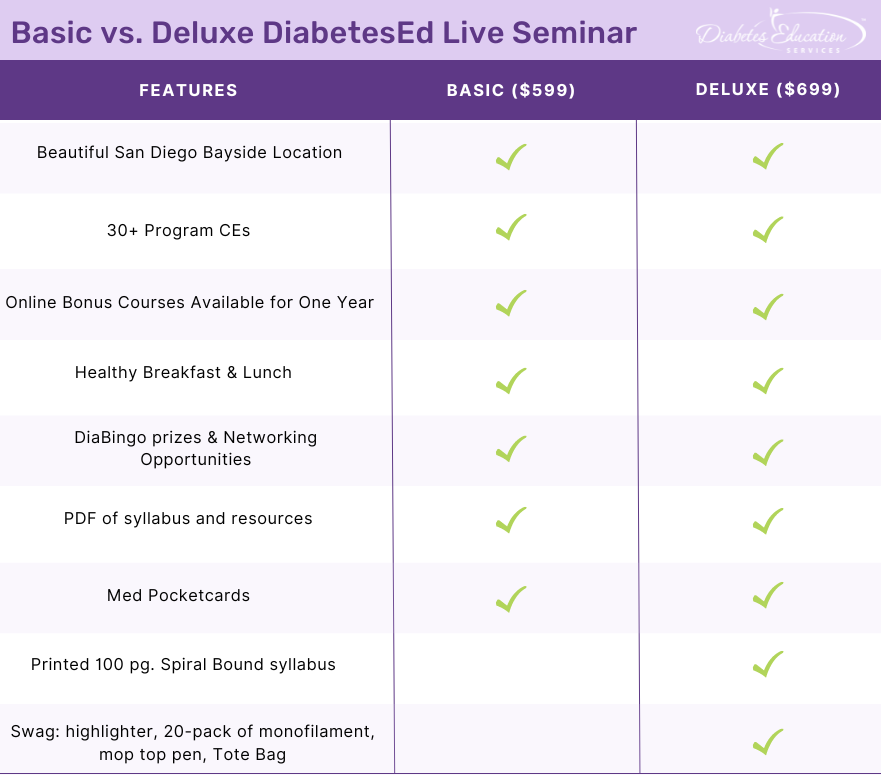
Join Coach Beverly and Team for two and a half days of knowledge-sharing, fun, networking, games with prizes, and “aha” moments in beautiful San Diego.
You don’t want to miss this one-of-a-kind learning opportunity. Get away from all those daily responsibilities and immerse yourself in a fun and intensive conference with plenty of networking opportunities.
Attendees will leave this conference with new tools and a more complete understanding of the latest advances in diabetes care, from medications to technology to Medical Nutrition Therapy!
Bring your colleagues and enjoy our friend discount.
Our team expertly translates the complex science of diabetes into understandable terms while keeping it real, practical, and fun.
Team of expert faculty includes:
- Diana Isaacs, PharmD, BCPS, BC-ADM, BCACP, CDCES – Educator of the Year, 2020
- Coach Beverly Thomassian, RN, MPH, CDCES, BC-ADM
- Ashley LaBrier, MS, RD, CDCES, Diabetes Program Coordinator
All hours earned count toward your CDCES Accreditation Information
Sign up for Diabetes Blog Bytes – we post one daily Blog Byte from Monday to Friday. And of course, Tuesday is our Question of the Week. It’s Informative and FREE! Sign up below!
The use of DES products does not guarantee the successful passage of the CDCES exam. CBDCE does not endorse any preparatory or review materials for the CDCES exam, except for those published by CBDCE.








