Rationale of the Week | Can JR repeat Group Classes?

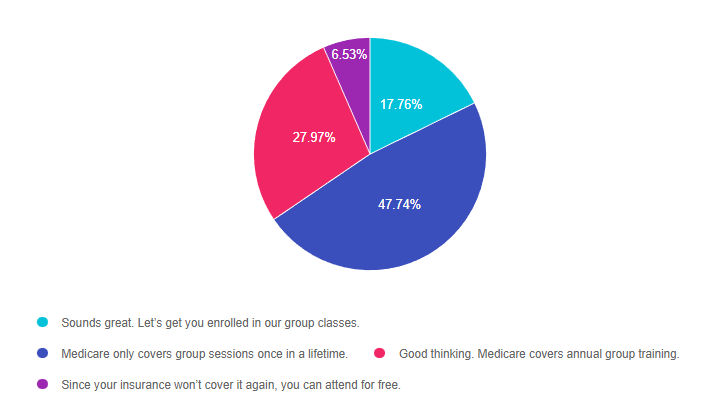
For last week’s practice question, we quizzed participants on reimbursement for group DSME classes through Medicare. 48% of respondents chose the best answer. We want to clarify and share this important information, so you can prepare for certification exams and pass it on to your colleagues.
Before we start though, if you don’t want any spoilers and haven’t tried the question yet, you can answer it below: Answer Question
Question:
JR is 73 years old and has Medicare Part A and B insurance. JR completed a Diabetes Self-Management Program at a local hospital when they were in their late 60s and tells you they want to repeat the group sessions since they have forgotten much of the information.
What is the most accurate response?
Answer Choices:
- Sounds great. Let’s get you enrolled in our group classes.
- Medicare only covers group sessions once in a lifetime.
- Good thinking. Medicare covers annual group training.
- Since your insurance won’t cover it again, you can attend for free.
Getting to the Best Answer
If you are thinking about taking the certification exam, this practice test question will set you up for success since there are questions on Medicare Reimbursement. Test writers anticipate possible answers based on the details in the question. They will wave those “juicy answers” right under your nose. Your job is to weed through the particulars, pluck out the most important elements and choose the BEST answer.
Answer 1 is incorrect. 17.76% chose this answer. “Sounds great. Let’s get you enrolled in our group classes.” A very welcoming answer, but unfortunately, it’s not accurate. According to Medicare Reimbursement Guidelines, Initial Diabetes Self Management Training (DSMT) is a “once-in-a-lifetime” Medicare benefit. Since JR completed a Diabetes Self-Management Program at a local hospital when they were in their late 60s, we assume that Medicare was billed for the service, since Medicare coverage starts at age 65. For this reason, it is important to verify that the beneficiary has not received any initial DSMT in the past prior to the delivery of the initial DSMT.
Answer 2 is correct. 47.74% of you chose this answer. “Medicare only covers group sessions once in a lifetime.” YES, this is the best answer. According to Medicare Reimbursement Guidelines, Initial Diabetes Self Management Training (DSMT) is a “once-in-a-lifetime” Medicare benefit. Since JR completed a Diabetes Self-Management Program at a local hospital when they were in their late 60s, we assume that Medicare was billed for the service, since Medicare coverage starts at age 65. For this reason, it is important to verify that the beneficiary has not received any initial DSMT in the past prior to the delivery of the initial DSMT.
However, if the beneficiary has received initial DSMT paid by another health insurance company, he/she is still eligible to receive the 10 hours of initial DSMT as a Medicare benefit.
Answer 3 is incorrect. About 27.97% of respondents chose this. “Good thinking. Medicare covers annual group training.” Another tempting answer, but not accurate. According to Medicare Reimbursement Guidelines, Initial Diabetes Self Management Training (DSMT) is a “once-in-a-lifetime” Medicare benefit. Since JR completed a Diabetes Self-Management Program at a local hospital when they were in their late 60s, we assume that Medicare was billed for the service, since Medicare coverage starts at age 65. For this reason, it is important to verify that the beneficiary has not received any initial DSMT in the past prior to the delivery of the initial DSMT.
Finally, Answer 4 is incorrect. 6.53% chose this answer. “Since your insurance won’t cover it again, you can attend for free.” This answer is kind hearted, but not correct. For Medicare, initial DSMT group classes can only be provided once in a lifetime and should be billed to Medicare and not offered for free. Programs can create a self-pay/uninsured policy where services are discounted (must be consistent in charges and discounts etc.).
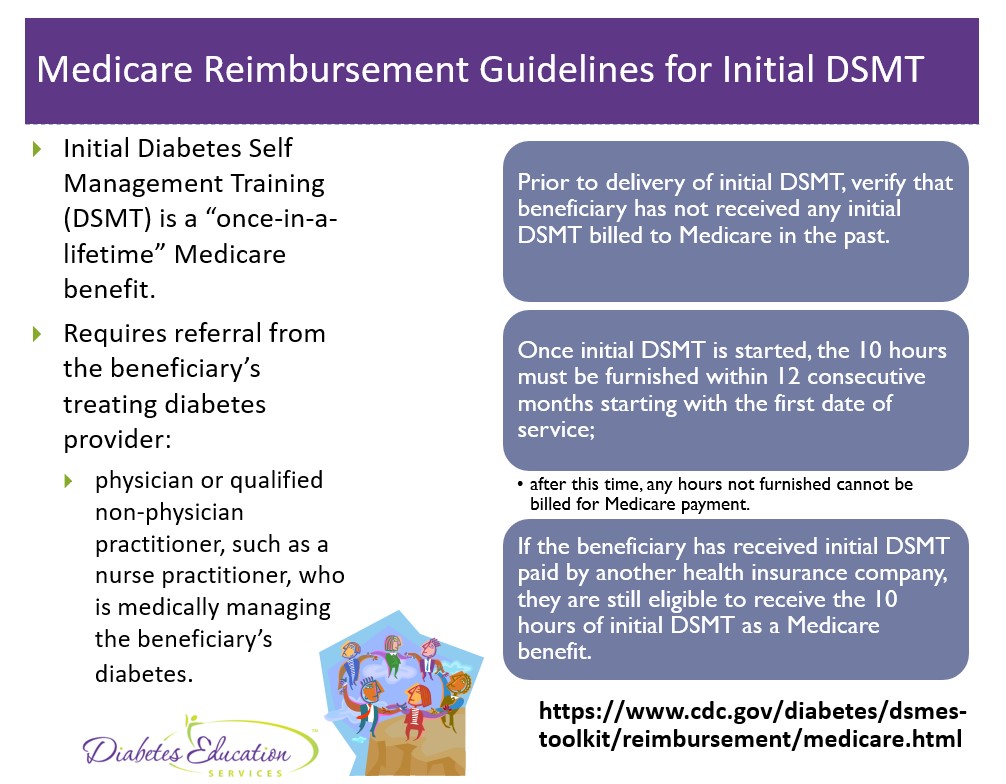
Here is a summary slide on Medicare Reimbursement Guidelines.
We hope you appreciate this week’s rationale! Thank you so much for taking the time to answer our Question of the Week and participate in this fun learning activity! You can read through the Medicare Reimbursement Guidelines here or the ADCES Info Sheet on DSMT Reimbursement join our Setting Up a Successful Diabetes Program & Medicare Reimbursement Webinar for more information.
Want to learn more about this practice question?
Join us LIVE in San Diego for our DiabetesEd Training Conference
October 11-13th, 2023

Two Registration Options
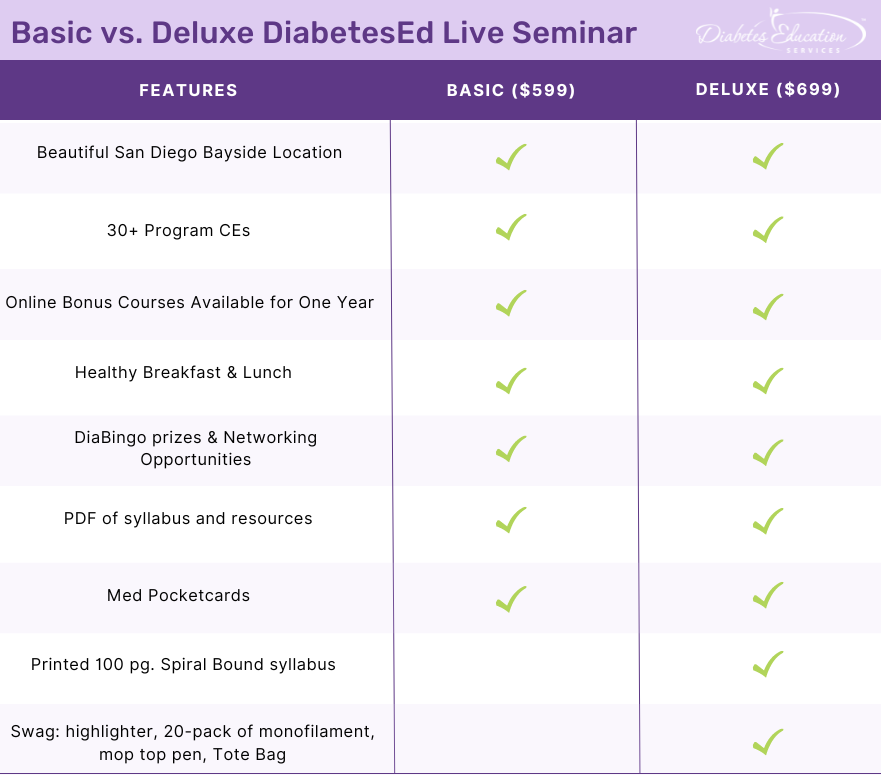
Join Coach Beverly and Team for two and a half days of knowledge-sharing, fun, networking, games with prizes, and “aha” moments in beautiful San Diego.
You don’t want to miss this one-of-a-kind learning opportunity. Get away from all those daily responsibilities and immerse yourself in a fun and intensive conference with plenty of networking opportunities.
Attendees will leave this conference with new tools and a more complete understanding of the latest advances in diabetes care, from medications to technology to Medical Nutrition Therapy!
Bring your colleagues and enjoy our friend discount.
Our team expertly translates the complex science of diabetes into understandable terms while keeping it real, practical, and fun.
Team of expert faculty includes:
- Diana Isaacs, PharmD, BCPS, BC-ADM, BCACP, CDCES – Educator of the Year, 2020
- Coach Beverly Thomassian, RN, MPH, CDCES, BC-ADM
- Ashley LaBrier, MS, RD, CDCES, Diabetes Program Coordinator
All hours earned count toward your CDCES Accreditation Information
Sign up for Diabetes Blog Bytes – we post one daily Blog Byte from Monday to Friday. And of course, Tuesday is our Question of the Week. It’s Informative and FREE! Sign up below!
The use of DES products does not guarantee the successful passage of the diabetes certification exams. CBDCE & ADCES does not endorse any preparatory or review materials for the certification exams, except for those published by CBDCE & ADCES.
Rationale of the Week | Carrying Insulin is too much Hassle!

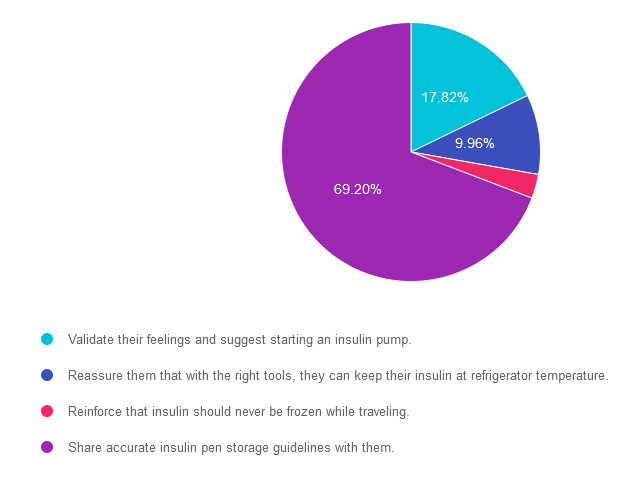
For last week’s practice question, we quizzed participants on carrying insulin. 69% of respondents chose the best answer. We want to clarify and share this important information, so you can pass it on to people living with diabetes and your colleagues, plus prepare for exam success!
Before we start though, if you don’t want any spoilers and haven’t tried the question yet, you can answer it below: Answer Question
Question: JL has new type 1 diabetes and their time in range is about 40%. They tell you that carrying insulin pens around on ice is such a hassle that they don’t give insulin before eating out.
What is the best response?
Answer Choices:
- Validate their feelings and suggest starting an insulin pump.
- Reassure them that with the right tools, they can keep their insulin at refrigerator temperature.
- Reinforce that insulin should never be frozen.
- Share accurate insulin pen storage guidelines with them.
Getting to the Best Answer
If you are thinking about taking the certification exam, this practice test question will set you up for success. Test writers anticipate possible answers based on the details in the question. They will wave those “juicy answers” right under your nose. Your job is to weed through the particulars, pluck out the most important elements and choose the BEST answer.
Answer 1 is incorrect. 17.82% chose this answer. “Validate their feelings and suggest starting an insulin pump.” Although this answer is tempting, it’s not the best answer. The first part of the answer that suggests validating their feelings is accurate. However, we would want to explore accurate insulin pen storage options before suggesting switching over to an insulin pump. Please see our insulin storage guidelines cheat sheet for more information.
Answer 2 is incorrect. 9.96% of you chose this answer. “Reassure them that with the right tools, they can keep their insulin at refrigerator temperature.” Once the person uses the insulin pen for the first time, it no longer needs to be refrigerated. Each type of insulin pen has storage guidelines for insulin kept at room temperature. Please see our insulin storage guidelines cheat sheet for more information.
Answer 3 is incorrect. About 3.01% of respondents chose this. “Reinforce that insulin should never be frozen.” It is true that insulin should never be frozen, but this is not the best answer. We also want to follow up with accurate and safe insulin pen storage information.
Finally, Answer 4 is correct. 69.20% chose this answer. “Share accurate insulin pen storage guidelines with them.” Yes, this is the best answer! Once insulin pens are used for the first time, they can be stored at room temperature. Of course, users have to avoid letting them overheat at temperatures of 86 degrees Fahrenheit or greater or getting too cold. Either situation can damage the insulin molecule. Please see our insulin storage cheat sheet for more information and feel free to share this info with colleagues and people with diabetes alike.
We hope you appreciate this week’s rationale! Thank you so much for taking the time to answer our Question of the Week and participate in this fun learning activity!
ReVive 5 Diabetes Training Program
“ReVive 5 Program is the best program I have ever attended – should be required for all diabetes educators! Thank you so much for translating this research into practical approaches!!” – Sarah F.
Save $100! Enroll now to watch the webinar on-demand

ReViVE 5 Diabetes Training Program:
Unlocking Hidden Barriers to Diabetes Management
Enroll Now and Save $100!
Recorded & Ready to Watch
Addressing diabetes distress can be challenging, even for seasoned healthcare professionals.
We invite you to attend this hands-on training program that provides the essential steps to address diabetes distress combined with an innovative approach to glucose management.
Team of Experts: ReVive 5 is taught by a team of 3 Interdisciplinary Experts:
Lawrence Fisher, Ph.D., ABPP, Professor Emeritus, UCSF
Susan Guzman, PhD
Beverly Thomassian, RN, MPH, CDCES, BC-ADM
Accredited Training Program:
- 15.0 CEs – Includes the 7-hour ReVive 5 Training Program, Certificate, and 5 FREE bonus courses to supplement content.
- A comprehensive set of assessment tools, educational materials, log sheets, and resources.
“ReVive 5” breathes new life into our relationship with diabetes, bringing a fresh perspective to both the person with diabetes and the provider.
All hours earned count toward your CDCES Accreditation Information
Sign up for Diabetes Blog Bytes – we post one daily Blog Byte from Monday to Friday. And of course, Tuesday is our Question of the Week. It’s Informative and FREE! Sign up below!
The use of DES products does not guarantee the successful passage of the CDCES exam. CBDCE does not endorse any preparatory or review materials for the CDCES exam, except for those published by CBDCE.
Rationale of the Week | Diabetes & Hospital Standards
The use of DES products does not guarantee the successful passage of the CDCES exam. CBDCE does not endorse any preparatory or review materials for the CDCES exam, except for those published by CBDCE.

For last week’s practice question, we quizzed participants on in-patient diabetes care. 42% of respondents chose the best answer. We want to clarify and share this important information, so you can pass it on to people living with diabetes and your colleagues, plus prepare for exam success!
Before we start though, if you don’t want any spoilers and haven’t tried the question yet, you can answer it below: Answer Question
Question: JR was admitted to the hospital with an infection and newly discovered diabetes. To get glucose to ADA target range for hospitalized individuals, JR was started on 12 units of basal insulin plus bolus insulin with meals. JR experienced a morning BG of 87 mg/dL, so the provider decreased the basal insulin to 9 units. JR’s morning blood sugar the next day was 157 mg/dL.
What is the best action?
Answer Choices:
- Increase basal insulin by 10- 20%.
- Intensify correction scale.
- Continue with same basal dose.
- Ask MS if they are snacking during the night before making adjustments.
Getting to the Best Answer
If you are thinking about taking the certification exam, this practice test question will set you up for success. Test writers anticipate possible answers based on the details in the question. They will wave those “juicy answers” right under your nose. Your job is to weed through the particulars, pluck out the most important elements and choose the BEST answer.
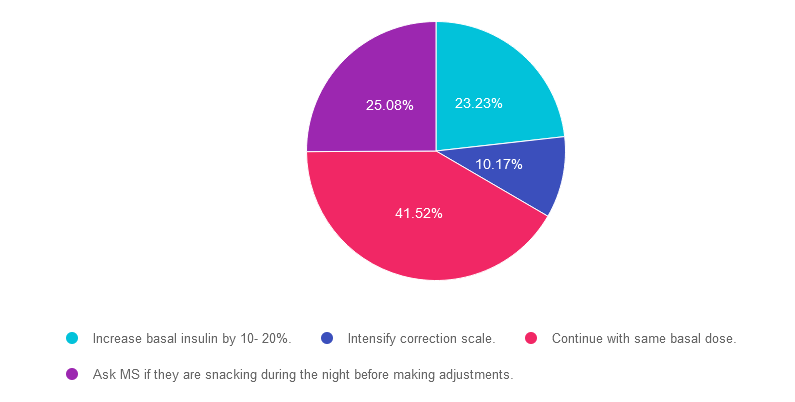
Answer 1 is incorrect. 23.23% chose this answer. “Increase basal insulin by 10- 20%.” This is a juicy answer because we typically consider the target glucose range 80-130 fasting and before meals. However, according to ADA Standards, the target glucose range during hospitalization is 140-180 mg/dL in general, and 100-180mg/dL in the non-critical care setting. Based on these inpatient goals, we wouldn’t need to increase basal insulin since JR’s morning glucose of 157 is right on target.
Answer 2 is incorrect. 10.17% of you chose this answer. “Intensify correction scale.” Another juicy answer because we typically consider the target glucose range 80-130 fasting and before meals. However, according to ADA Standards, the target glucose range during hospitalization is 140-180 mg/dL in general, and 100-180mg/dL in the non-critical care setting. Based on these inpatient goals, we wouldn’t need to intensify the correction scale since JR’s morning glucose of 157 is right on target. In addition, correction insulin doesn’t have much impact on fasting glucose. That’s the job of basal insulin.
Answer 3 is correct. About 41.52% of respondents chose this. “Continue with same basal dose.” YES, this is the BEST answer. According to ADA Standards, the target glucose range during hospitalization is 140-180 mg/dL in general, and 100-180mg/dL in the non-critical care setting. Based on these inpatient goals, we wouldn’t need to intensify the basal insulin since JR’s morning glucose of 157 is right on target.
Finally, Answer 4 is incorrect. 25.08% chose this answer. “Ask MS if they are snacking during the night before making adjustments.” Another juicy answer. It doesn’t really matter if MS was snacking, since according to ADA Standards, the target glucose range during hospitalization is 140-180 mg/dL in general, and 100-180mg/dL in the non-critical care setting. Based on these inpatient goals, regardless of whether or not they were snacking, JR’s morning glucose of 157 is right on target.
We hope you appreciate this week’s rationale! Thank you so much for taking the time to answer our Question of the Week and participate in this fun learning activity!
Want to learn more about this question? Enroll in our
Level 2 | Hospitals & Hyperglycemia
Research clearly demonstrates the importance of glucose control during hospitalization to improve outcomes not only in the inpatient setting but after discharge. This course reviews the evidence that supports inpatient glucose control & outlines practical strategies to achieve targets in the inpatient setting. We incorporate the latest American Diabetes Association’s (ADA) Standards of Medical Care in Diabetes & provide links to resources & inpatient management templates.
Objectives:
- Describe the impact of hyperglycemia in the hospital setting.
- Discuss the importance of inpatient glucose control.
- List three strategies to get glucose to goal in the hospital setting.
Intended Audience: A great course for healthcare professionals seeking strategies to manage and improve inpatient diabetes care.
The use of DES products does not guarantee the successful passage of the CDCES exam. CBDCE does not endorse any preparatory or review materials for the CDCES exam, except for those published by CBDCE.
Rationale of the Week | Pregnancy & Diabetes Medication

For last week’s practice question, we quizzed participants on gestational diabetes & medication. A whopping 70% of respondents chose the best answer – great job. We want to clarify and share this important information, so you can pass it on to people living with diabetes and your colleagues, plus prepare for exam success!
Before we start though, if you don’t want any spoilers and haven’t tried the question yet, you can answer it below: Answer Question
Question: AR has PCOS and type 2 diabetes and is in shock because they just discovered they are 6 weeks pregnant. AR takes metformin 1000mg BID plus empagliflozin (Jardiance) 25 mg and their most recent A1C is 8.6%.
Which of the following actions do you recommend?
Answer Choices:
- Stop empagliflozin
- Stop metformin, keep empagliflozin
- Stop metformin and empagliflozin, start insulin.
- Stop empagliflozin, start a GLP-1 inhibitor
Getting to the Best Answer
If you are thinking about taking the certification exam, this practice test question will set you up for success. Test writers anticipate possible answers based on the details in the question. They will wave those “juicy answers” right under your nose. Your job is to weed through the particulars, pluck out the most important elements and choose the BEST answer.
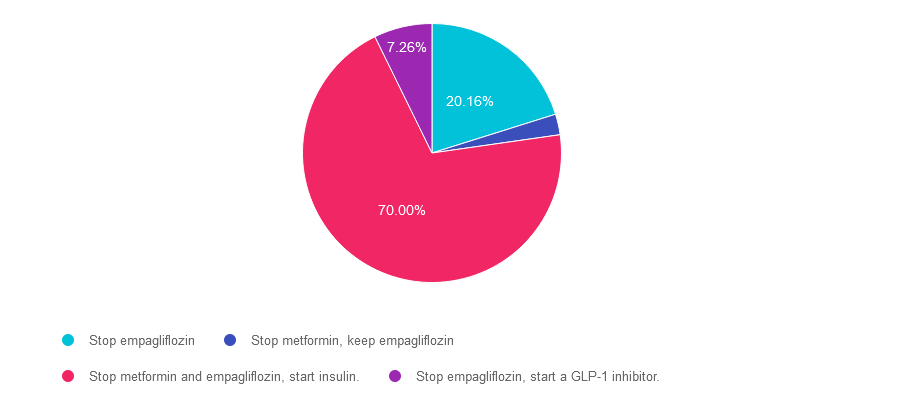
Answer 1 is incorrect. 20.16% chose this answer. “Stop empagliflozin.” It is true that empagliflozin and all SGLT-2’s are not indicated during pregnancy. However, there is a better answer given that her A1C of 8.6% is above the pregnancy target of less than 6.5%.
Answer 2 is incorrect. 2.58% of you chose this answer. “Stop metformin, keep empagliflozin.” Empagliflozin and all SGLT-2’s are contraindicated during pregnancy, so this answer is not the best choice.
Answer 3 is correct. About 70% of respondents chose this. “Stop metformin and empagliflozin, start insulin.” GREAT JOB. Given that her A1C of 8.6% is above the pregnancy target of less than 6.5%, insulin absolutely needs to be started to get glucose to goal. According to the ADA Standards, the provider may opt to continue the metformin treatment for PCOS for the first trimester But given the urgent need to get blood glucose to target, this individual will be most effectively managed with a combination of nutrition therapy and insulin.
Finally, Answer 4 is incorrect. 7.26% chose this answer. “Stop empagliflozin, start a GLP-1 inhibitor.” Yes, we need to stop empagliflozin since all SGLT-2’s are contraindicated during pregnancy. However, GLP-1 Inhibitors are also contraindicated during pregnancy, so this answer is incorrect.
We hope you appreciate this week’s rationale! Thank you so much for taking the time to answer our Question of the Week and participate in this fun learning activity!
Want to learn more about this question? Enroll in our
Level 2 | Pregnancy & Diabetes
Pregnancy with diabetes is confronted with a variety of issues that require special attention, education, & understanding. This course reviews those special needs while focusing on Gestational Diabetes & Pre-Existing Diabetes. Included are the most recent diagnostic criteria, management goals, & prevention of complications during pregnancy. This is a helpful review for Certification Exams & those who want more information on people who are pregnant & live with diabetes.
Objectives:
- List three issues that affect pregnancy with diabetes.
- Describe the unique attributes of pre-existing diabetes in pregnancy & gestational diabetes.
- State the diagnostic criteria & management goals for gestational diabetes.
- Potential short-term & long-term complications of fetal exposure to hypoglycemia.
- Prevention measures to keep mother & baby healthy.
Intended Audience: A great course for healthcare professionals seeking to enhance their knowledge of the issues surrounding pregnancy and diabetes and appropriate care to improve outcomes.
Level 2 | Hospitals & Hyperglycemia
Research clearly demonstrates the importance of glucose control during hospitalization to improve outcomes not only in the inpatient setting but after discharge. This course reviews the evidence that supports inpatient glucose control & outlines practical strategies to achieve targets in the inpatient setting. We incorporate the latest American Diabetes Association’s (ADA) Standards of Medical Care in Diabetes & provide links to resources & inpatient management templates.
Objectives:
- Describe the impact of hyperglycemia in the hospital setting.
- Discuss the importance of inpatient glucose control.
- List three strategies to get glucose to goal in the hospital setting.
Intended Audience: A great course for healthcare professionals seeking strategies to manage and improve inpatient diabetes care.
Rationale of the Week | AR is pregnant and Worried

For last week’s practice question, we quizzed participants on gestational diabetes & pregnancy complications. 68% of respondents chose the best answer. We want to clarify and share this important information, so you can pass it on to people living with diabetes and your colleagues, plus prepare for exam success!
Before we start though, if you don’t want any spoilers and haven’t tried the question yet, you can answer it below: Answer Question
Question: AR has PCOS type 2 diabetes and worried because they just discovered they are 6 weeks pregnant. AR takes metformin 1000mg BID plus empagliflozin (Jardiance) 25 mg and their most recent A1C is 8.6%.
Which of the following is a potential complication associated with hyperglycemia during the first 10 weeks of pregnancy?
Answer Choices:
- Intrauterine hypoglycemia
- Macrosomia and post-natal jaundice
- Neonatal respiratory distress
- Diabetic embryopathy
Getting to the Best Answer
If you are thinking about taking the certification exam, this practice test question will set you up for success. Test writers anticipate possible answers based on the details in the question. They will wave those “juicy answers” right under your nose. Your job is to weed through the particulars, pluck out the most important elements and choose the BEST answer.
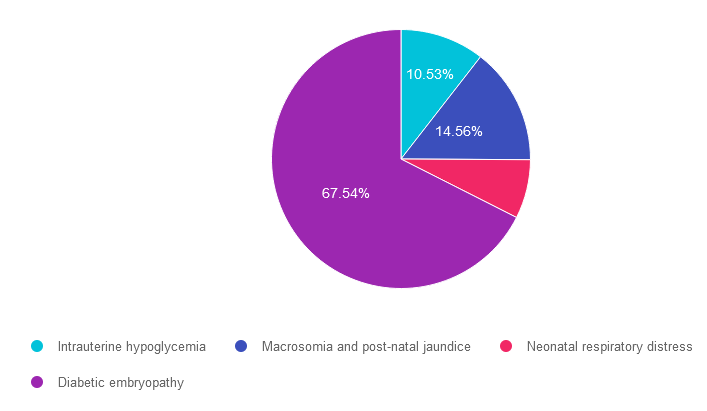
Answer 1 is incorrect. 10.53% chose this answer. “Intrauterine hypoglycemia.” Although this answer is tempting, it is not accurate. If the fetus experienced elevated blood sugars (from mom) during gestation, this stimulates increased fetal production of insulin. After delivery, baby’s who were exposed to intrauterine hyperglycemia are at higher risk of post-delivery hypoglycemia (not intrauterine hypoglycemia).
Answer 2 is incorrect. 14.56% of you chose this answer. “Macrosomia and post-natal jaundice.” Although this answer is tempting, it is not accurate. If the fetus experienced elevated blood sugars (from mom) during their first 10 weeks of gestation, this stimulates increased fetal production of insulin and can stimulate extra fat stores later in pregnancy leading to larger babies and higher risk for post delivery jaundice. However, the question is asking, what complications can elevated blood sugars cause during their first 10 weeks of pregnancy when the organs are developing?
Answer 3 is kind of incorrect. About 7.37% of respondents chose this. “Neonatal respiratory distress.” The question is asking, if the fetus experienced elevated blood sugars (from mom) during the first 10 weeks of gestation, what complications can elevated blood sugars cause during the first trimester pregnancy when the organs are developing? The lungs can be affected by first trimester hyperglycemia, causing the newborn to struggle with respiratory distress.
Finally, Answer 4 is correct. 67.54% chose this answer. “Diabetic embryopathy.” GREAT JOB. This is the best answer. If the fetus experienced elevated blood sugars (from mom) during the first 10 weeks of gestation, embryonic complications result from elevated blood sugars during the first trimester pregnancy when the organs are developing. These can include, congenital heart disease, renal anomalies and caudal regression.
We hope you appreciate this week’s rationale! Thank you so much for taking the time to answer our Question of the Week and participate in this fun learning activity!
Want to learn more about this question? Enroll in our
Level 2 | Pregnancy & Diabetes
Pregnancy with diabetes is confronted with a variety of issues that require special attention, education, & understanding. This course reviews those special needs while focusing on Gestational Diabetes & Pre-Existing Diabetes. Included are the most recent diagnostic criteria, management goals, & prevention of complications during pregnancy. This is a helpful review for Certification Exams & those who want more information on people who are pregnant & live with diabetes.
Objectives:
- List three issues that affect pregnancy with diabetes.
- Describe the unique attributes of pre-existing diabetes in pregnancy & gestational diabetes.
- State the diagnostic criteria & management goals for gestational diabetes.
- Potential short-term & long-term complications of fetal exposure to hypoglycemia.
- Prevention measures to keep mother & baby healthy.
Intended Audience: A great course for healthcare professionals seeking to enhance their knowledge of the issues surrounding pregnancy and diabetes and appropriate care to improve outcomes.
Level 2 | Hospitals & Hyperglycemia
Research clearly demonstrates the importance of glucose control during hospitalization to improve outcomes not only in the inpatient setting but after discharge. This course reviews the evidence that supports inpatient glucose control & outlines practical strategies to achieve targets in the inpatient setting. We incorporate the latest American Diabetes Association’s (ADA) Standards of Medical Care in Diabetes & provide links to resources & inpatient management templates.
Objectives:
- Describe the impact of hyperglycemia in the hospital setting.
- Discuss the importance of inpatient glucose control.
- List three strategies to get glucose to goal in the hospital setting.
Intended Audience: A great course for healthcare professionals seeking strategies to manage and improve inpatient diabetes care.
Oops – Rationale of the Week Error | Which Meds for a 14-year-old with Type 2?

We want to fix our mistake and clarify this important information. For last month’s practice question, a participant reached out to us and kindly shared that one of the medications listed was actually recently approved by the FDA for kids ages 10-17. We want to make this right, so you can pass on updated info to people living with diabetes and your colleagues, plus prepare for exam success! Look for 2 correct answers and explanations for this Rationale of the Week.
Question: KS is 14 years old and recently diagnosed with type 2 diabetes. Their A1C is 8.6%, LDL cholesterol is 137 mg/dL and their GFR is greater than 90.
Based on this clinical information and the ADA Standards for Pediatric Care, in addition to lifestyle and behavior changes, what medication(s) would be recommended?
Before we start though, if you don’t want any spoilers and haven’t tried the question yet, you can answer it below: Answer Question
Based on this clinical information and the ADA Standards for Pediatric Care, in addition to lifestyle and behavior changes, what medication(s) would be recommended?
Answer Choices:
- Dulaglutide (Trulicity) and Metformin
- Metformin and an ACE Inhibitor
- Exenatide XR (Bydureon) and a statin
- Empagliflozin (Jardiance) or Metformin
Getting to the Best Answer
If you are thinking about taking the certification exam, this practice test question will set you up for success. Test writers anticipate possible answers based on the details in the question. They will wave those “juicy answers” right under your nose. Your job is to weed through the particulars, pluck out the most important elements and choose the BEST answer.
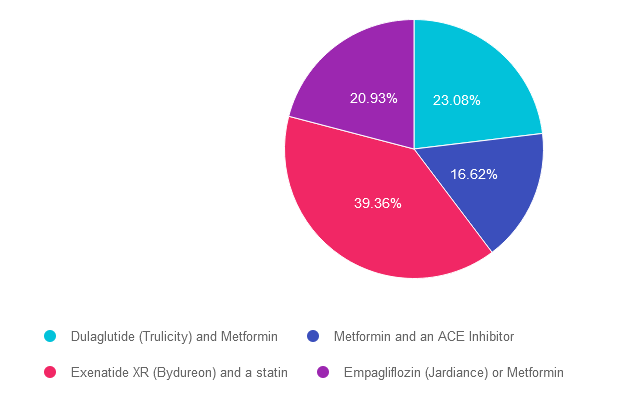
Answer 1 is CORRECT. 23.08% chose this answer. “Dulaglutide (Trulicity) and Metformin.” Both metformin and Dulaglutide (Trulicity) are FDA approved for children starting at age of ten. Dulaglutide was recently FDA approved for pediatrics up at doses up to 1.5 mg per week. We have updated our eMed PocketCards to include this GLP-1 RA as approved for kids ages 10-17.
Answer 2 is incorrect. 16.62% of you chose this answer. “Metformin and an ACE Inhibitor.” Although this answer if tempting, because metformin is FDA approved for children starting at age of ten, there is no mention of hypertension that would justify starting an ACE Inhibitor. See Med PocketCards. For this reason, this is not the best answer.
Answer 3 is CORRECT. About 39.36% of respondents chose this. “Exenatide XR (Bydureon) and a statin.” YES, this is the BEST answer. GREAT JOB. Two of the GLP-1 RA’s are approved for kids including exenatide XR and liraglutide. See Med PocketCards. In addition, statins are indicated for children age 10 or greater if they have diabetes and an LDL cholesterol of 130 mg/dL or greater.
Finally, Answer 4 is incorrect. 20.93% chose this answer. “Empagliflozin (Jardiance) or Metformin.” Although this answer if tempting, because metformin is FDA approved for children starting at age of ten, none of the SGLT-2’s are approved for pediatrics, including empagliflozin. See Med PocketCards. For this reason, this is not the best answer.
We hope you appreciate this week’s rationale! Thank you so much for taking the time to answer our Question of the Week and participate in this fun learning activity! For more information, see ADA Standard 14 on Children and Adolescents or join our webinar (see below).
Want to learn more about this question? Enroll in our
Level 2 | From Tots to Teens | Diabetes Standards | 1.5 CEs
This course includes updated goals & guidelines for children living with type 1 or type 2 diabetes. This course discusses the special issues diabetes educators need to be aware of when working with children with diabetes & their families. We discuss the clinical presentation of diabetes, goals of care, & normal growth & development through the early years through adolescence. Strategies to prevent acute & long-term complications are included with an emphasis on positive coping for families & children with diabetes.
Objectives:
- Discuss the goals of care for Type 1 and Type 2 Kids with Diabetes.
- State Strategies to prevent acute and chronic complications.
- Discuss the importance of positive psychosocial adjustment & resources.
Intended Audience: A great course for healthcare professionals seeking information about providing care for children with diabetes and their families.
Don’t worry if you can’t make it live. Your registration guarantees access to the recorded version in the Online University.
All hours earned count toward your CDCES Accreditation Information
Sign up for Diabetes Blog Bytes – we post one daily Blog Byte from Monday to Friday. And of course, Tuesday is our Question of the Week. It’s Informative and FREE! Sign up below!
The use of DES products does not guarantee the successful passage of the CDCES exam. CBDCE does not endorse any preparatory or review materials for the CDCES exam, except for those published by CBDCE.
Rationale of the Week | What’s Wrong with JR’s Foot?

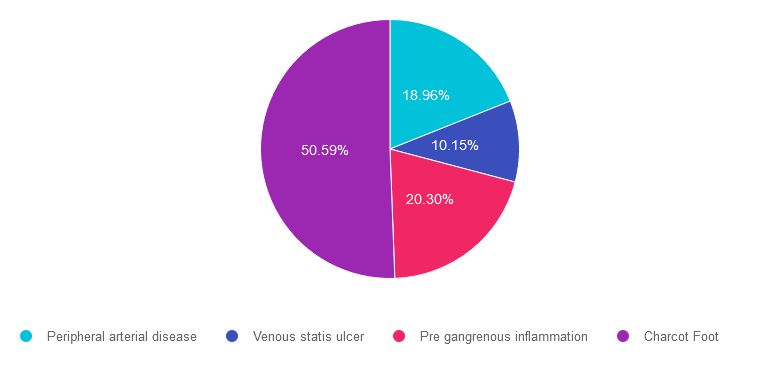
For last week’s practice question, we quizzed participants on what is wrong with JR’s foot. 51% of respondents chose the best answer. We want to clarify and share this important information, so you can pass it on to people living with diabetes and your colleagues, plus prepare for exam success!
Before we start though, if you don’t want any spoilers and haven’t tried the question yet, you can answer it below: Answer Question
Question: JR arrives at the clinic wearing a walking boot due to a recent foot injury. Tells you that they “banged their foot” on some farm equipment and since then it has been warm and swollen. It hurt at first, but the pain has diminished with time.
When JR takes off the boot, you see that the left foot needs attention.
Based on this photo, what diabetes-related foot condition do you suspect?

Answer Choices:
- Peripheral arterial disease
- Venous statis ulcer
- Pre gangrenous inflammation
- Charcot Foot
Getting to the Best Answer
If you are thinking about taking the certification exam, this practice test question will set you up for success. Test writers anticipate possible answers based on the details in the question. They will wave those “juicy answers” right under your nose. Your job is to weed through the particulars, pluck out the most important elements and choose the BEST answer.
Answer 1 is incorrect. 18.96% chose this answer. Peripheral arterial disease. People experiencing peripheral arterial disease usually present with thinner, pale, lower extremities. They complain of pain in their calves or buttocks when walking due to intermittent claudication. Pulses are difficult to palpate due to diminished circulation to lower extremities.
Answer 2 is incorrect. 10.15% of you chose this answer. Venous statis ulcer. This person may have lower extremity venous disease as evidenced by the marked edema and darkened skin. However, although the foot is red and swollen there is no ulcer present in this photo.
Answer 3 is incorrect. About 20.30% of respondents chose this. Pre gangrenous inflammation. This person is certainly experiencing inflammation and edema. However, we can’t determine if their lower extremity is moving toward gangrene just from this photo.
Finally, Answer 4 is correct. 50.59% chose this answer. Charcot Foot. YES, this is the BEST answer. GREAT JOB. This person arrived with a suddenly misshapen foot, coupled with edema and redness. The skin was intact and the individual denied pain. This presentation is the hallmark of Charcot foot, a condition that is a combination of neuropathy and diminished circulation coupled with elevated blood glucose levels. It requires immediate medical attention by a foot specialist. JR sought care from a Podiatrist and his foot was secured in a cast to protect the foot and prevent further damage.
We hope you appreciate this week’s rationale! Thank you so much for taking the time to answer our Question of the Week and participate in this fun learning activity!
Want to learn more about this question? Enroll in our
Level 2 | Lower Extremity Assessment | 1.5 CEs
People with diabetes are at increased risk of Lower Extremity Complications. This course reviews the steps involved in performing a detailed assessment of the lower extremities, including how to use a monofilament and tuning fork to detect neuropathy. We also discuss the significance of the Ankle Brachial Index and strategies to prevent lower extremity complications.
Objectives:
- Describe the risk factors for lower extremity complications.
- Discuss prevention strategies.
- Demonstrate steps involved in a lower extremity assessment.
Intended Audience: This is a great course for healthcare professionals who want to learn the steps involved in providing a thorough lower extremity assessment.
Don’t worry if you can’t make it live. Your registration guarantees access to the recorded version in the Online University.
All hours earned count toward your CDCES Accreditation Information
Sign up for Diabetes Blog Bytes – we post one daily Blog Byte from Monday to Friday. And of course, Tuesday is our Question of the Week. It’s Informative and FREE! Sign up below!
The use of DES products does not guarantee the successful passage of the CDCES exam. CBDCE does not endorse any preparatory or review materials for the CDCES exam, except for those published by CBDCE.
Rationale of the Week | Do Statins Cause Dementia?

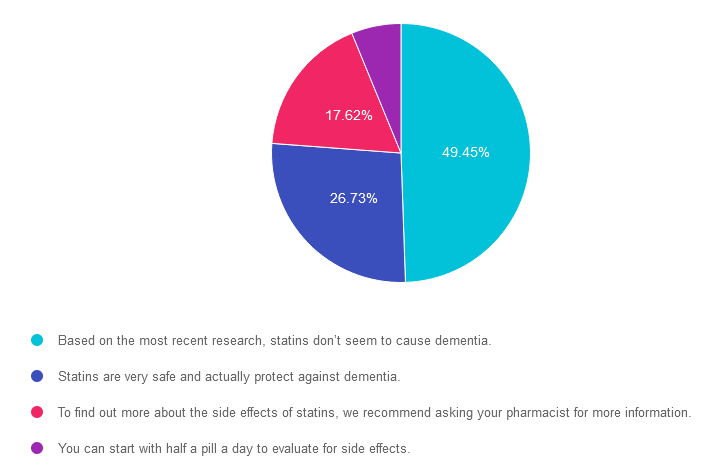
For last week’s practice question, we quizzed participants on statins & the risk of dementia. 49% of respondents chose the best answer. We want to clarify and share this important information, so you can pass it on to people living with diabetes and your colleagues, plus prepare for exam success!
Before we start though, if you don’t want any spoilers and haven’t tried the question yet, you can answer it below: Answer Question
Question: LR is 78 years old with a new diagnosis of diabetes. Their A1C is 7.9%, LDL cholesterol is 98 mg/dL, GFR is 58 mg/g and their BP is 124/78. The provider recommends a referral to the RD and DSME program and writes a prescription for metformin XR 500mg daily and lovastatin 20mg. LR is worried about taking a statin because they heard it can cause dementia.
Based on the ADA Standards, what is the best response?
Answer Choices:
- Based on the most recent research, statins don’t seem to cause dementia.
- Statins are very safe and actually protect against dementia.
- To find out more about the side effects of statins, we recommend asking your pharmacist for more information.
- You can start with half a pill a day to evaluate for side effects.
Getting to the Best Answer
If you are thinking about taking the certification exam, this practice test question will set you up for success. Test writers anticipate possible answers based on the details in the question. They will wave those “juicy answers” right under your nose. Your job is to weed through the particulars, pluck out the most important elements and choose the BEST answer.
Answer 1 is correct. 49.45% chose this answer. “Based on the most recent research, statins don’t seem to cause dementia.” YES, is the BEST answer. According to ADA 2023 SOC 10 a recent systematic review of the U.S. Food and Drug Administration’s (FDA’s) postmarketing surveillance databases, randomized controlled trials, and cohort, case-control, and cross-sectional studies evaluating cognition in patients receiving statins found that published data do not reveal an adverse effect of statins on cognition (138). Therefore, a concern that statins or other lipid-lowering agents might cause cognitive dysfunction or dementia is not currently supported by evidence and should not deter their use in individuals with diabetes at high risk for ASCVD (138).
Answer 2 is incorrect. 26.73% of you chose this answer. “Statins are very safe and actually protect against dementia.” Although the first part of this statement is correct, statins are safe, there is no evidence presented in the ADA Standards that statins protect against dementia.
Answer 3 is incorrect. About 17.62% of respondents chose this. “To find out more about the side effects of statins, we recommend asking your pharmacist for more information.” Although pharmacists are incredibly knowledgeable about medications, diabetes specialists can relate evidence based information to the people we serve, instead of making them take additional action to get the information they need to move forward. The good news is that there is no evidence that statins or other lipid-lowering agents might cause cognitive dysfunction or dementia and their use is recommended in individuals with diabetes at high risk for ASCVD.
Finally, Answer 4 is incorrect. 6.19% chose this answer. “You can start with half a pill a day to evaluate for side effects.” This approach is tempting, but it doesn’t address the fear of the statin causing dementia. The good news is that there is no evidence that statins or other lipid-lowering agents might cause cognitive dysfunction or dementia and their use is recommended in individuals with diabetes at high risk for ASCVD.
We hope you appreciate this week’s rationale! Thank you so much for taking the time to answer our Question of the Week and participate in this fun learning activity!
Want to learn more about this question? Enroll in our
Level 2 | Older Adults & Diabetes | 1.5 CEs
We are living longer & more people are getting diabetes. The American Diabetes Association has updated the Older Adults Standards, with special attention to considering the reduction of medication & insulin therapy intensity. The older population has unique issues & special needs that require consideration as we provide diabetes self-management education. This online course highlights key areas of assessment, intervention, and advocacy for older clients living with diabetes.
Objectives:
- Self-management considerations for older individuals.
- Strategies to prevent complications & maintain optimal quality of life.
- The role of the Diabetes Care & Education Specialist as an advocate.
Intended Audience: An important course for healthcare professionals seeking to gain an understanding of the special issues and goals for older adults.
Don’t worry if you can’t make it live. Your registration guarantees access to the recorded version in the Online University.
All hours earned count toward your CDCES Accreditation Information
Sign up for Diabetes Blog Bytes – we post one daily Blog Byte from Monday to Friday. And of course, Tuesday is our Question of the Week. It’s Informative and FREE! Sign up below!
The use of DES products does not guarantee the successful passage of the CDCES exam. CBDCE does not endorse any preparatory or review materials for the CDCES exam, except for those published by CBDCE.








