Rationale of the Week | JR is Skipping Provider Appointments

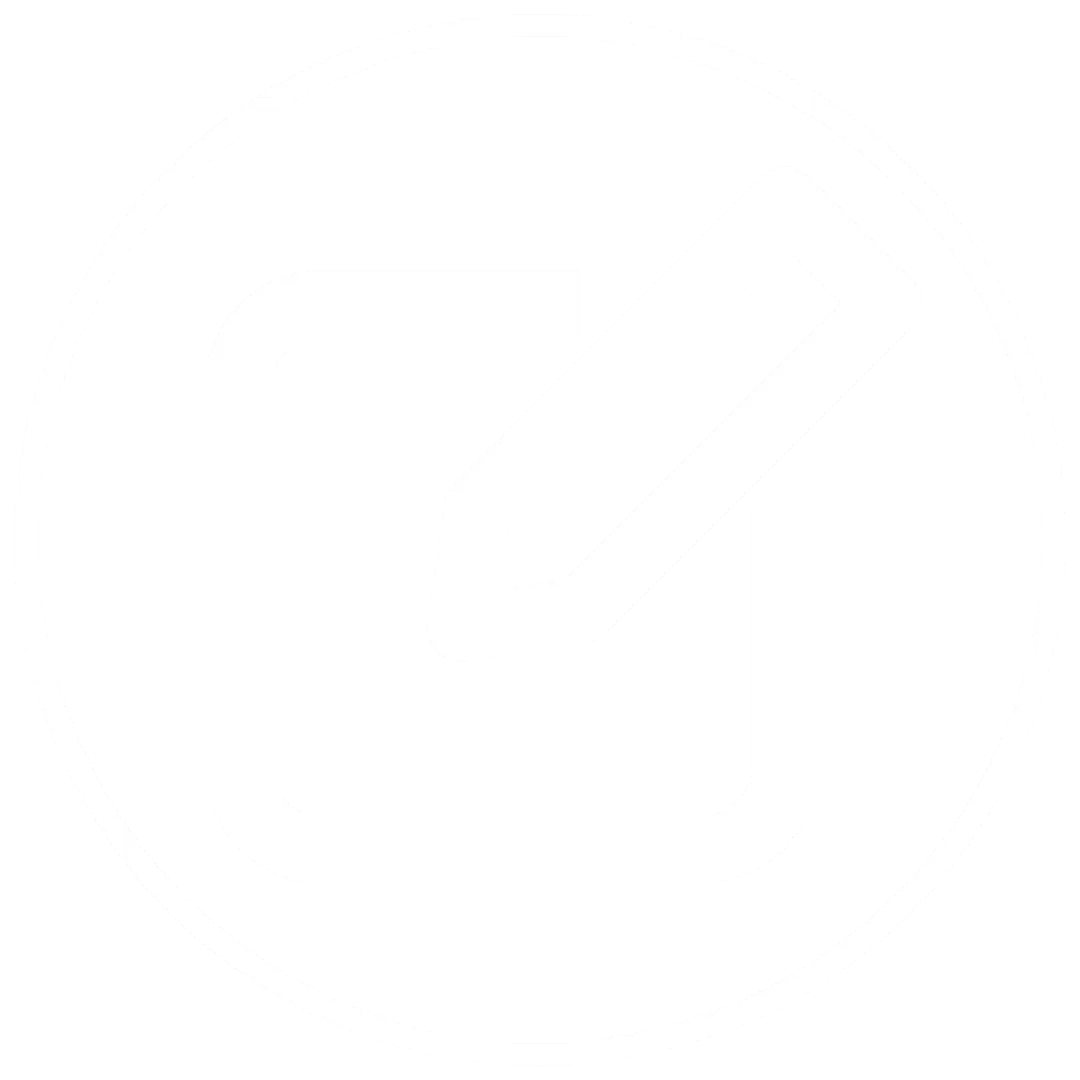
For last week’s practice question, we quizzed participants on diabetes distress. 78% of respondents chose the best answer. We want to clarify and share this important information, so you can pass it on to people living with diabetes and your colleagues, plus prepare for exam success!
Before we start though, if you don’t want any spoilers and haven’t tried the question yet, you can answer it below: Answer Question
Question: JR has type 1 diabetes and tells you, “My doctor just doesn’t seem to understand how to manage type 1 diabetes. Sometimes, I just skip my appointments because it feels like a waste of time.” JR’s most recent A1C was 8.7% and their time in ranges keeps decreasing with each visit.
Based on this, you realize that JR’s provider-related diabetes distress:
Answer Choices:
- has intensified to clinical depression.
- requires urgent referral to a mental health professional.
- could be responsive to self-management coaching.
- may be a sign of disordered eating.
Getting to the Best Answer
If you are thinking about taking the certification exam, this practice test question will set you up for success. Test writers anticipate possible answers based on the details in the question. They will wave those “juicy answers” right under your nose. Your job is to weed through the particulars, pluck out the most important elements, get rid of false answers, do any math very carefully and choose the BEST answer.
Answer 1 is incorrect. 9.58% chose this answer. “has intensified to clinical depression.” This is a tempting answer, but we don’t enough evidence to support that JR is struggling with depression. If we had JR complete the Diabetes Distress Scale, he would certainly score high on provider related distress based on this statement, “My doctor just doesn’t seem to understand how to manage type 1 diabetes. Sometimes, I just skip my appointments because it feels like a waste of time.” These comments certainly fit in the distress category. Through careful questioning and exploration, the diabetes educator could certainly help with problem solving.
Answer 2 is incorrect. 8.18% of you chose this answer. “requires urgent referral to a mental health professional.” Based on JR’s statement, “My doctor just doesn’t seem to understand how to manage type 1 diabetes. Sometimes, I just skip my appointments because it feels like a waste of time,” JR is certainly in distress. However, there is no language indicating that JR is in imminent danger of self-harm. Through careful questioning and exploration, the diabetes educator could certainly carefully assess JR’s mental health state and help with problem solving and referrals as needed.
Answer 3 is correct. About 77.84% of respondents chose this. “could be responsive to self-management coaching.” YES. This is the best answer. We could start by administering the Diabetes Distress Scale and then hone in on the high scoring areas. Then through careful questioning and exploration, the diabetes educator could certainly help with problem solving and identify if additional resources or referrals are needed.
Finally, Answer 4 is incorrect. 4.39% chose this answer. “may be a sign of disordered eating.” but we don’t enough evidence to support that JR is experiencing disordered eating. However, if we had JR complete the Diabetes Distress Scale, he would certainly score high on provider related distress based on this statement, “My doctor just doesn’t seem to understand how to manage type 1 diabetes. Sometimes, I just skip my appointments because it feels like a waste of time.”
We hope you appreciate this week’s rationale! Thank you so much for taking the time to answer our Question of the Week and participate in this fun learning activity!
Want to learn more about using the Diabetes Distress Scale and Coaching Strategies? Join our next
ReVive 5 Diabetes Training Program
Addressing diabetes distress can be tricky, even for seasoned healthcare professionals.
We invite you to attend this hands-on training program that provides the essential steps to address diabetes distress combined with an innovative approach to glucose management. Our experts offer realistic strategies to address diabetes distress that you can immediately apply to your practice setting. Plus, the ReVive 5 Program provides a breadth of tools and resources to create more meaningful connections with people with diabetes.
“ReVive 5” breathes new life into our relationship with diabetes, bringing a fresh perspective to both the person with diabetes and the provider.
Join A Team of Experts – Save $100
Team of Experts: ReVive 5 is taught by a team of 3 Interdisciplinary Experts:

- Lawrence Fisher, Ph.D., ABPP, Professor Emeritus, UCSF
- Susan Guzman, PhD
- Beverly Thomassian, RN, MPH, CDCES, BC-ADM
Accredited Training Program:
- 14.0 CEs – Includes the 7-hour Session ReVive 5 Training Program, Certificate, and 5 FREE bonus courses to supplement content.
- A comprehensive set of assessment tools, educational materials, log sheets, and resources.
Speakers Interviews – Learn more about the ReVive 5 Team
What is the Biggest Takeaway when Addressing Diabetes Distress? – Dr. Susan Guzman
Do you have to be a Mental Health Expert to Tackle Diabetes Distress? – Dr. Lawrence Fisher
Why I Transformed my Approach to Diabetes Self-Management Education- Coach Beverly
Don’t worry if you can’t make it live. Your registration guarantees access to the recorded version in the Online University.
All hours earned count toward your CDCES Accreditation Information
Sign up for Diabetes Blog Bytes – we post one daily Blog Byte from Monday to Friday. And of course, Tuesday is our Question of the Week. It’s Informative and FREE! Sign up below!
The use of DES products does not guarantee the successful passage of the CDCES exam. CBDCE does not endorse any preparatory or review materials for the CDCES exam, except for those published by CBDCE.
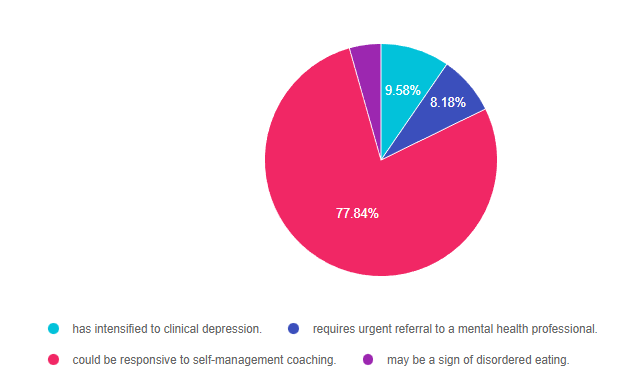
Rationale of the Week | Get your Calculator – How many Pens?

For last week’s practice question, we quizzed participants on counting every pen(ny.) 47% of respondents chose the best answer. We want to clarify and share this important information, so you can pass it on to people living with diabetes and your colleagues, plus prepare for exam success!
Before we start though, if you don’t want any spoilers and haven’t tried the question yet, you can answer it below: Answer Question
Question: KL takes 5-10 units of insulin glulisine (Apidra) based on an insulin scale before each of their 3 daily meals and 30 units of glargine (Basaglar) at bedtime.
Based on this information, how many u-100 glulisine (Apidra) insulin pens would KL use a month?
Answer Choices:
- 2 vials
- 4 pens
- 6 pens
- 3 pens
Getting to the Best Answer
If you are thinking about taking the certification exam, this practice test question will set you up for success. Test writers anticipate possible answers based on the details in the question. They will wave those “juicy answers” right under your nose. Your job is to weed through the particulars, pluck out the most important elements, get rid of false answers, do any math very carefully and choose the BEST answer.
Answer 1 is incorrect. 6.31% chose this answer. “2 vials.” One way to quickly eliminate a wrong answer is to see if the units in the question match the units in the answer. The question asks, “How many pens” would JR need a month and this answer is in “vials”. We can cross this one off as false. **See complete math explanation below.
Answer 2 is correct. 46.64% of you chose this answer. “4 pens.” YES.. Great job. You not only calculated JR’s insulin needs, but added in extra insulin for priming too! **See complete math explanation below.
Answer 3 is incorrect. About 16.24% of respondents chose this. “6 pens.” This was a juicy answer that lured respondents into adding together the glulisine and glargine dose. The answer only asks for how many glulisine pens would JR need a month. **See complete math explanation below.
Finally, Answer 4 is incorrect. 30.82% chose this answer. “3 pens.” This was the juiciest answer of all. However, it doesn’t take into account the 2 units of insulin used to prime the pen before each injection. Also, if they had 3 pens of 300 units each, what if they made a mistake or wasted a dose, or needed a little extra.. they might be short on insulin. We always want to allow for a little cushion, just in case. **See complete math explanation below.
**Complete explanation – Doing the math.
If JR takes 5-10 units of insulin glulisine (Apidra) 3 times a day, we have to assume they will be taking the highest dose each time, so they don’t run out of insulin. That means JR uses 30 units a day of glulisine. 30 units a day x 30 days in a month = 900 units. But wait, JR needs to prime the pen first with a 2 unit “air shot” before each injection to make sure insulin is flowing through the needle before each of their 3 injections. So this means that JR is using up to 12 units of insulin 3 times a day or 36 units x 30 days = 1,080 units of glulisine a month. The next thing we need to know is that each U-100 glulisine pen holds 300 units of insulin (see our Insulin Storage Cheat Sheet 2023). Now, we can do the math. JR uses 1,080 units of insulin a day. Since each pen holds 300 units, we take 1080 and divide by 300 for a total of 3.6. This means JR will need 4 pens of glulisine each month to manage their diabetes.
We hope you appreciate this week’s rationale! Thank you so much for taking the time to answer our Question of the Week and participate in this fun learning activity!
Want to learn more about this question? Join our NEW
ReVive 5 Diabetes Training Program
Whether you are a novice or an expert in providing diabetes care, we invite you to attend this exciting training program that provides the essential steps to address diabetes distress combined with an innovative approach to glucose management that will revolutionize your practice.
“ReVive 5” breathes new life into our relationship with diabetes, bringing a fresh perspective to both the person with diabetes and the provider.
Join A Team of Experts – Save $100
Team of Experts: ReVive 5 is taught by a team of 3 Interdisciplinary Experts:

- Lawrence Fisher, Ph.D., ABPP, Professor Emeritus, UCSF
- Susan Guzman, PhD
- Beverly Thomassian, RN, MPH, CDCES, BC-ADM
Accredited Training Program:
- 14.0 CEs – Includes the 7-hour Session ReVive 5 Training Program, Certificate, and 5 FREE bonus courses to supplement content.
- A comprehensive set of assessment tools, educational materials, log sheets, and resources.
Speakers Interviews – Learn more about the ReVive 5 Team
What is the Biggest Takeaway when Addressing Diabetes Distress? – Dr. Susan Guzman
Do you have to be a Mental Health Expert to Tackle Diabetes Distress? – Dr. Lawrence Fisher
Why I Transformed my Approach to Diabetes Self-Management Education- Coach Beverly
Don’t worry if you can’t make it live. Your registration guarantees access to the recorded version in the Online University.
All hours earned count toward your CDCES Accreditation Information
Sign up for Diabetes Blog Bytes – we post one daily Blog Byte from Monday to Friday. And of course, Tuesday is our Question of the Week. It’s Informative and FREE! Sign up below!
The use of DES products does not guarantee the successful passage of the CDCES exam. CBDCE does not endorse any preparatory or review materials for the CDCES exam, except for those published by CBDCE.
Rationale of the Week | Is JR at Risk for NASH?

For last week’s practice question, we quizzed participants on being at risk for NASH. 63% of respondents chose the best answer. We want to clarify and share this important information, so you can pass it on to people living with diabetes and your colleagues, plus prepare for exam success!
Before we start though, if you don’t want any spoilers and haven’t tried the question yet, you can answer it below: Answer Question
Question: JR is 46 years old with type 2 diabetes and a BMI of 33. In addition, JR has hypertension and hyperlipidemia, with elevated liver enzymes (ALT and AST).
According to the latest ADA Standards, which of the following would best help determine if JR is at risk for liver fibrosis and cirrhosis?
Answer Choices:
- UACR
- FIB-4
- GAD or ICA
- Weight in (kg) divided by the square of height in meters (m2)
Getting to the Best Answer
If you are thinking about taking the certification exam, this practice test question will set you up for success. Test writers anticipate possible answers based on the details in the question. They will wave those “juicy answers” right under your nose. Your job is to weed through the particulars, pluck out the most important elements and choose the BEST answer.
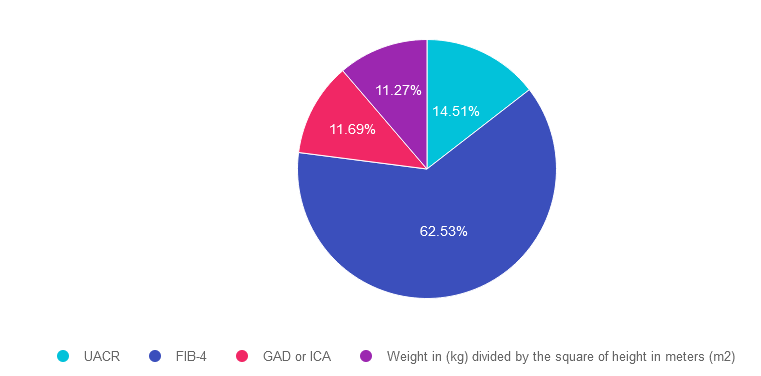
Answer 1 is incorrect. 14.51% chose this answer. “UACR.” This is a juicy answer, however the Urinary Albumin Creatinine Ratio (UACR) evaluates kidney function and doesn’t provide any hepatic insights. Instead we would recommend the Fibrosis-4 Index for Liver Fibrosis helps determine risk of hepatic cirrhosis and inflammation (see answer 2).
Answer 2 is correct. 62.53% of you chose this answer. “FIB-4.” GREAT JOB. The Fibrosis-4 Index for Liver Fibrosis helps determine risk of hepatic cirrhosis and inflammation. By entering the person’s age, AST, ALT and Platelet count using the FIB-4 calculator, a risk level is calculated (see slide below). The hope is that by screening for hepatic issues early, we can take action to protect the liver and improve outcomes.
Answer 3 is incorrect. About 11.69% of respondents chose this. “GAD or ICA.” Although this answer is familiar, it does not match the intent of the question. GAD and ICA are blood tests to determine if someone has autoimmune mediated type 1 diabetes. Instead we would recommend the Fibrosis-4 Index for Liver Fibrosis helps determine risk of hepatic cirrhosis and inflammation (see answer 2).
Finally, Answer 4 is incorrect. 11.27% chose this answer. “Weight in (kg) divided by the square of height in meters (m2).” This answer is also familiar since it is the formula to determine a person’s body mass index (BMI). Instead we would recommend the Fibrosis-4 Index for Liver Fibrosis helps determine risk of hepatic cirrhosis and inflammation (see answer 2).
We hope you appreciate this week’s rationale! Thank you so much for taking the time to answer our Question of the Week and participate in this fun learning activity! Learn more by attending our Virtual Conference plus save $100 through April 18, 2023.
Register now for our Virtual DiabetesEd Training Conference

Your team is invited to our Virtual DiabetesEd™ Training Conference! Set your team apart and prepare for diabetes certification!
Join this state-of-the-art conference taught by content experts, Diana Isaacs, PharmD, BCPS, BCACP, BC-ADM, CDCES, Beverly Thomassian RN, MPH, CDCES, BC-ADM, and Ashley LaBrier who are passionate about improving diabetes care.
Group discounts are available!*
All hours earned count toward your CDCES Accreditation Information
Sign up for Diabetes Blog Bytes – we post one daily Blog Byte from Monday to Friday. And of course, Tuesday is our Question of the Week. It’s Informative and FREE! Sign up below!
The use of DES products does not guarantee the successful passage of the CDCES exam. CBDCE does not endorse any preparatory or review materials for the CDCES exam, except for those published by CBDCE.
Rationale of the Week | Birthday Cake Dilemma

For last week’s practice question, we quizzed participants on having their cake and eating it too. A whopping 94% of respondents chose the best answer. We want to celebrate your success and give you all a shout out for a job well done.
Before we start though if you don’t want any spoilers and haven’t tried the question yet, you can answer it below: Answer Question
Question: AJ is a 9-year-old with type 1 diabetes, A1c of 7.2%, and uses an insulin pump and CGM. They ask you how to include a piece of birthday cake for an upcoming birthday celebration.
What is the best advice?
Answer Choices:
- Accept the cake but don’t actually eat it.
- Increase their daytime basal insulin to prevent hyperglycemia.
- Take additional bolus insulin to cover the extra carbs.
- Encourage AJ to have a piece of fruit instead.
Getting to the Best Answer
If you are thinking about taking the certification exam, this practice test question will set you up for success. Test writers anticipate possible answers based on the details in the question. They will wave those “juicy answers” right under your nose. Your job is to weed through the particulars, pluck out the most important elements and choose the BEST Person-Centered answer.
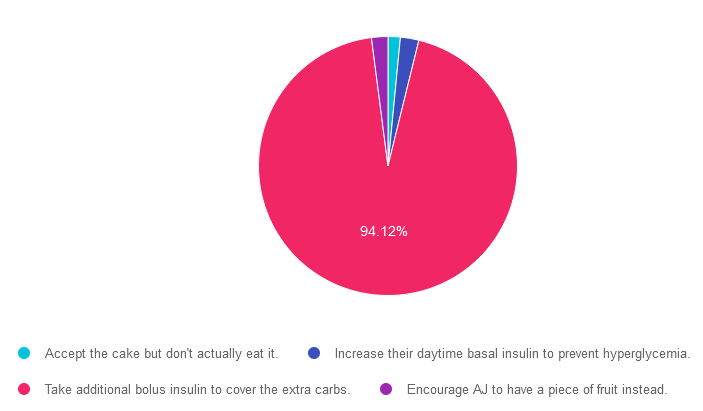
Answer 1 is incorrect. 1.53% chose this answer. “Accept the cake but don’t actually eat it.” Since this doesn’t honor AJ’s choice to accept and enjoy the cake, it is not the best answer. People with diabetes can absolutely enjoy special treats by adjusting their bolus insulin dose to account for the extra carbs to prevent post cake hyperglycemia.
Answer 2 is incorrect. 2.3% of you chose this answer. “Increase their daytime basal insulin to prevent hyperglycemia.” People with diabetes can absolutely enjoy special treats by adjusting their bolus insulin dose to account for the extra carbs to prevent post cake hyperglycemia.
Answer 3 is correct. About 94.12% of respondents chose this. “Take additional bolus insulin to cover the extra carbs.” YAY! This person centered approach is the BEST guilt free answer since it recognizes and respects AJ’s choice to enjoy a piece of birthday cake while still managing blood sugars with extra bolus insulin.
Finally, Answer 4 is incorrect. 2.05% chose this answer. “Encourage AJ to have a piece of fruit instead.” Since this doesn’t honor AJ’s choice to accept and enjoy the cake, it is not the best answer. People with diabetes can absolutely enjoy special treats by adjusting their bolus insulin dose to account for the extra carbs to prevent post cake hyperglycemia.
We hope you appreciate this week’s person-centered rationale! Thank you so much for taking the time to answer our Question of the Week and participate in this fun learning activity!
Want to learn more about Medical Nutrition Therapy?
You are invited to join our Virtual Conference with our Nutrition expert speaker, Ashley LaBrier, MS, RD, CDCES, who will be providing a half-day presentation on this important topic!

Ashley LaBrier, MS, RD, CDES, is an innovator in the field of diabetes, nutrition, and technology. Ashley is a consultant and the Diabetes Education Program Coordinator at the Salinas Valley Medical Clinic’s Diabetes & Endocrine Center.
Ms. LaBrier is passionate about providing person-centered education to empower those who live with diabetes. Having been diagnosed with type 1 diabetes herself nearly 20 years ago, she combines her professional knowledge with personal experience and understanding.
Virtual DiabetesEd Training Conference

Whether you are new to diabetes or a seasoned expert, you’ll benefit from this virtual conference with the latest research plus critical content that you can immediately apply to your clinical practice.
If you are seeking a state-of-the-art review of current diabetes care, this course is for you. Our team has been fine-tuning this course for over fifteen years, and we know what you need. This program can also be a great addition to your CDCES or BC-ADM exam study plan.
Group discounts are available!*
Download Course Flyer | Download Schedule
All hours earned count toward your CDCES Accreditation Information
Sign up for Diabetes Blog Bytes – we post one daily Blog Byte from Monday to Friday. And of course, Tuesday is our Question of the Week. It’s Informative and FREE! Sign up below!
The use of DES products does not guarantee the successful passage of the CDCES exam. CBDCE does not endorse any preparatory or review materials for the CDCES exam, except for those published by CBDCE.
Rationale of the Week | Why the Post Meal Glucose Spike?

For last week’s practice question, we quizzed participants on post-meal glucose spikes. 51% of respondents chose the best answer. We want to clarify and share this important information, so you can pass it on to people living with diabetes and your colleagues, plus prepare for exam success!
Before we start though, if you don’t want any spoilers and haven’t tried the question yet, you can answer it below: Answer Question
Question: TR can’t figure out why her BG always spikes after breakfast.
How many grams of carb is in the following breakfast? 2 corn tortillas, 2 fried eggs with salsa, ½ cup hashbrowns and an 8 ounce glass of milk.
Answer Choices:
- 75 gms
- 57 gms
- 60 gms
- 4 servings
Getting to the Best Answer
If you are thinking about taking the certification exam, this practice test question will set you up for success. Test writers anticipate possible answers based on the details in the question. They will wave those “juicy answers” right under your nose. Your job is to weed through the particulars, pluck out the most important elements and choose the BEST answer.
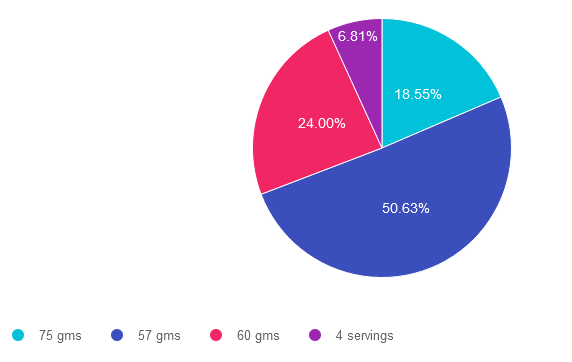
Answer 1 is incorrect. 18.55% chose this answer, “75 gms”. To answer this question accurately, it is important to be familiar with the common servings sizes of carbs and to know which foods don’t count as carbs. This answer is incorrect because it is an over estimate of carbs in this meal.
Answer 2 is correct. 50.63% of you chose this answer, “57 gms”. Yes, this is the BEST Answer. GREAT JOB. Here are the carbs broken down. 2 corn tortillas = 30gms carb, 2 fried eggs with salsa= 0 gms carb, ½ cup hashbrowns – 15 gms and an 8 ounce glass of milk =12gms. 30 + 15+ 12 = 57 gms of carbohydrate in this meal. An important fact to keep in mind for exam success; a cup of milk is 12 gms of carb, not 15gms.
Answer 3 is incorrect. About 24% of respondents chose this, “60 gms” This was the juicy answer. An important fact to keep in mind for exam success; a cup of milk is 12 gms of carb, not 15gms. Here are the carbs broken down. 2 corn tortillas = 30gms carb, 2 fried eggs with salsa= 0 gms carb, ½ cup hashbrowns – 15 gms and an 8 ounce glass of milk =12gms. 30 + 15+ 12 = 57 gms of carbohydrate in this meal.
Finally, Answer 4 is incorrect. 6.81% chose this answer, “4 servings” This answer is tempting, but the question asks “how many gms of carbohydrate” not, how many servings of carb. A great idea is to always eliminate answers that don’t match the unit of measure used in the question.
If you want more info on carb counting, you are invited to join our Virtual Conference in April. Save $100 through April 7, 2023 (see info below). We hope you appreciate this week’s rationale!
Want to learn more about Medical Nutrition Therapy?
You are invited to join our Virtual Conference with our Nutrition expert speaker, Ashley LaBrier, MS, RD, CDCES, who will be providing a half-day presentation on this important topic!

Ashley LaBrier, MS, RD, CDES, is an innovator in the field of diabetes, nutrition, and technology. Ashley is a consultant and the Diabetes Education Program Coordinator at the Salinas Valley Medical Clinic’s Diabetes & Endocrine Center.
Ms. LaBrier is passionate about providing person-centered education to empower those who live with diabetes. Having been diagnosed with type 1 diabetes herself nearly 20 years ago, she combines her professional knowledge with personal experience and understanding.
Virtual DiabetesEd Training Conference
Whether you are new to diabetes or a seasoned expert, you’ll benefit from this virtual conference with the latest research plus critical content that you can immediately apply to your clinical practice.
If you are seeking a state-of-the-art review of current diabetes care, this course is for you. Our team has been fine-tuning this course for over fifteen years, and we know what you need. This program can also be a great addition to your CDCES or BC-ADM exam study plan.
Group discounts are available!*
Download Course Flyer | Download Schedule
All hours earned count toward your CDCES Accreditation Information
Sign up for Diabetes Blog Bytes – we post one daily Blog Byte from Monday to Friday. And of course, Tuesday is our Question of the Week. It’s Informative and FREE! Sign up below!
The use of DES products does not guarantee the successful passage of the CDCES exam. CBDCE does not endorse any preparatory or review materials for the CDCES exam, except for those published by CBDCE.
Rationale of the Week | According to label, how many kcals total Fat?

For last week’s practice question, we quizzed participants on their nutrition label reading ability. About 59% of respondents chose the best answer, revealing how challenging nutrition labels can be to dissect and understand, even for super-smart health care professionals. We want to clarify and share this important information, so you can pass it on to people living with diabetes and your colleagues, plus prepare for exam success!
Before we start though, if you don’t want any spoilers and haven’t tried the question yet, you can answer it below: Answer Question
Question: You are teaching about counting fat.
If they ate 2 servings of this Macaroni and Cheese (see label), how many calories would come from total fat?
Answer Choices:

- 16 gms
- 144 kcals
- 460 kcals
- 20%
Getting to the Best Answer
If you are thinking about taking the certification exam, this practice test question will set you up for success. Test writers anticipate possible answers based on the details in the question or image (like this nutrition label). They will wave those “juicy answers” right under your nose. Your job is to weed through the particulars, pluck out the most important elements and choose the BEST answer.
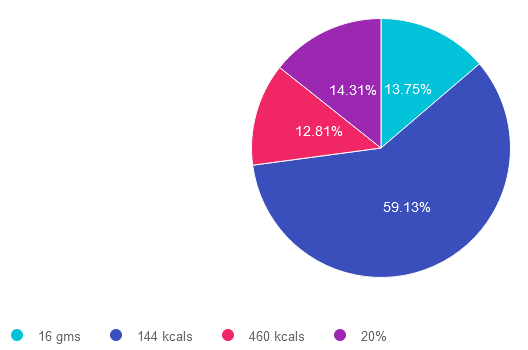
Answer 1 is incorrect. 13.75% chose this answer. “16 gms.” While it is true that there are 16 grams of fat in 2 servings of macaroni and cheese, this question doesn’t ask the test taker, “how many grams of fat”. The intent of the question is to determine how many kcals from total fat. Right away, we know this answer is wrong, because the unit is in gms not kcals.
Answer 2 is correct. 59.13% of you chose this answer. “144 kcals.” GREAT JOB. To get to this answer, you have to do a little math and know one important fact; there are 9 kcals in 1 gm of fat. On this label, one serving of macaroni and cheese has 8 gms, so 2 servings has 16 gms of total fat. 16 gms x 9 kcals = 144 kcals. In preparation for certification exams (and providing nutrition counseling), knowing how to read labels and being familiar with the kcals for protein, carbs and fats is very helpful.
Answer 3 is incorrect. About 12.81% of respondents chose this. “460 kcals.” This would be the correct answer if the question read, “how many total calories” is in 2 servings of this macaroni and cheese. However, the question is only asking for total fat calories in 2 servings. To get to best answer, you have to do a little math and know one important fact; there are 9 kcals in 1 gm of fat. On this label, one serving of macaroni and cheese has 8 gms, so 2 servings has 16 gms of total fat. 16 gms x 9 kcals = 144 kcals.
Finally, Answer 4 is incorrect. 14.31% chose this answer. “20%.” While it is true that there is 20% total fat in 2 servings of macaroni and cheese, this question doesn’t ask the test taker, “what percent of fat”. The intent of the question is to determine how many kcals from total fat. Right away, we know this answer is wrong, because the unit is in % not kcals.
We hope you appreciate this week’s rationale! Thank you so much for taking the time to answer our Question of the Week and participate in this fun learning activity!
Want to learn more about Medical Nutrition Therapy?
You are invited to join our Virtual Conference with our Nutrition expert speaker, Ashley LaBrier, MS, RD, CDCES, who will be providing a half-day presentation on this important topic!

Ashley LaBrier, MS, RD, CDES, is an innovator in the field of diabetes, nutrition, and technology. Ashley is a consultant and the Diabetes Education Program Coordinator at the Salinas Valley Medical Clinic’s Diabetes & Endocrine Center.
Ms. LaBrier is passionate about providing person-centered education to empower those who live with diabetes. Having been diagnosed with type 1 diabetes herself nearly 20 years ago, she combines her professional knowledge with personal experience and understanding.
Virtual DiabetesEd Training Conference

Whether you are new to diabetes or a seasoned expert, you’ll benefit from this virtual conference with the latest research plus critical content that you can immediately apply to your clinical practice.
If you are seeking a state-of-the-art review of current diabetes care, this course is for you. Our team has been fine-tuning this course for over fifteen years, and we know what you need. This program can also be a great addition to your CDCES or BC-ADM exam study plan.
Group discounts are available!*
Download Course Flyer | Download Schedule
All hours earned count toward your CDCES Accreditation Information
Sign up for Diabetes Blog Bytes – we post one daily Blog Byte from Monday to Friday. And of course, Tuesday is our Question of the Week. It’s Informative and FREE! Sign up below!
The use of DES products does not guarantee the successful passage of the CDCES exam. CBDCE does not endorse any preparatory or review materials for the CDCES exam, except for those published by CBDCE.
Rationale of the Week | Is Fast Food the best solution for Food Insecurity?

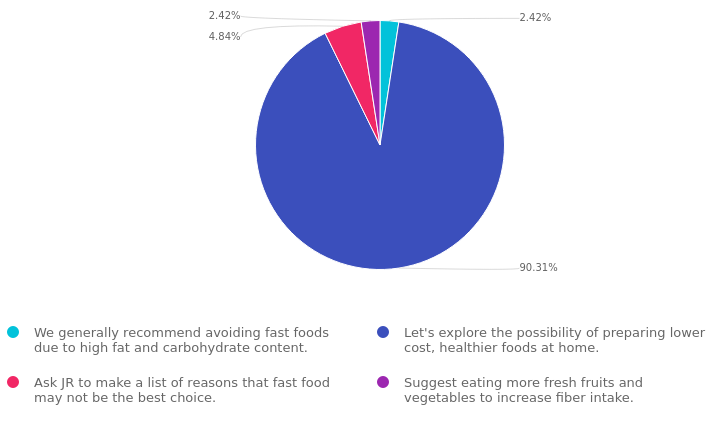
For last week’s practice question, we quizzed participants on if fast food is the best solution for food insecurity. 90% of respondents chose the best answer. We want to clarify and share this important information, so you can pass it on to people living with diabetes and your colleagues, plus prepare for exam success!
Before we start though, if you don’t want any spoilers and haven’t tried the question yet, you can answer it below: Answer Question
Question: Due to the increased cost of groceries, JR tells you all they can afford to eat are fast foods.
As a diabetes care and education specialist, what is the best response?
Answer Choices:
- We generally recommend avoiding fast foods due to high fat and carbohydrate content.
- Let’s explore the possibility of preparing lower-cost, healthier foods at home.
- Ask JR to make a list of reasons that fast food may not be the best choice.
- Suggest eating more fresh fruits and vegetables to increase fiber intake.
Getting to the Best Answer
If you are thinking about taking the certification exam, this practice test question will set you up for success. Test writers anticipate possible answers based on the details in the question. They will wave those “juicy answers” right under your nose. Your job is to weed through the particulars, pluck out the most important elements and choose the BEST answer.
Answer 1 is incorrect. 2.42% chose this answer. “We generally recommend avoiding fast foods due to high fat and carbohydrate content.” While it is true that many fast food options are often high in fat and carbohydrates, we want to honor people choices and situations. This response might be received as critical and could limit the opportunity to collaborate on healthier approaches.
Answer 2 is correct. 90.31% of you chose this answer. “Let’s explore the possibility of preparing lower-cost, healthier foods at home.” GREAT JOB, most chose this BEST answer for good reason. This person-centered approach invites JR to explore lower cost foods that they can prepare at home. It honors JR’s concern over their limited income and invites collaborative problem solving.
Answer 3 is incorrect. 4.48% of respondents chose this. “Ask JR to make a list of reasons that fast food may not be the best choice.” As with the first answer, this response might be received as critical and could limit the opportunity to collaborate on healthier approaches.
Finally, Answer 4 is incorrect. 2.42% chose this answer. “Suggest eating more fresh fruits and vegetables to increase fiber intake.” This answer doesn’t really address the intent of the question and might limit the opportunity to collaborate on problem solving.
We hope you appreciate this week’s rationale! Thank you so much for taking the time to answer our Question of the Week and participate in this fun learning activity!
Want to learn more about Medical Nutrition Therapy?
You are invited to join our Virtual Conference with our Nutrition expert speaker, Ashley LaBrier, MS, RD, CDCES, who will be providing a half-day presentation on this important topic!

Ashley LaBrier, MS, RD, CDES, is an innovator in the field of diabetes, nutrition, and technology. Ashley is a consultant and the Diabetes Education Program Coordinator at the Salinas Valley Medical Clinic’s Diabetes & Endocrine Center.
Ms. LaBrier is passionate about providing person-centered education to empower those who live with diabetes. Having been diagnosed with type 1 diabetes herself nearly 20 years ago, she combines her professional knowledge with personal experience and understanding.
Virtual DiabetesEd Training Conference

Whether you are new to diabetes or a seasoned expert, you’ll benefit from this virtual conference with the latest research plus critical content that you can immediately apply to your clinical practice.
If you are seeking a state-of-the-art review of current diabetes care, this course is for you. Our team has been fine-tuning this course for over fifteen years, and we know what you need. This program can also be a great addition to your CDCES or BC-ADM exam study plan.
Group discounts are available!*
Download Course Flyer | Download Schedule
All hours earned count toward your CDCES Accreditation Information
Sign up for Diabetes Blog Bytes – we post one daily Blog Byte from Monday to Friday. And of course, Tuesday is our Question of the Week. It’s Informative and FREE! Sign up below!
The use of DES products does not guarantee the successful passage of the CDCES exam. CBDCE does not endorse any preparatory or review materials for the CDCES exam, except for those published by CBDCE.
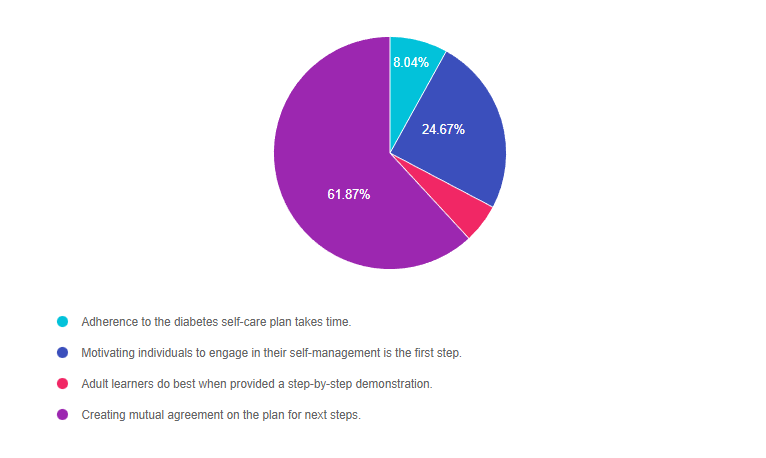
Rationale of the Week | What is Person-Centered Care?

For last week’s practice question, we quizzed participants on person-centered care. 62% of respondents chose the best answer. We want to clarify and share this important information, so you can pass it on to people living with diabetes and your colleagues, plus prepare for exam success!
Before we start though if you don’t want any spoilers and haven’t tried the question yet, you can answer it below: Answer Question
Question: TR is a healthcare professional who provides diabetes care and education support. They are interested in providing more person-centered care to the individuals they serve.
Which of the following statements verifies they are on the right track?
Answer Choices:
- Adherence to the diabetes self-care plan takes time.
- Motivating individuals to engage in their self-management is the first step.
- Adult learners do best when provided a step-by-step demonstration.
- Creating mutual agreement on the plan for next steps.
Getting to the Best Answer
If you are thinking about taking the certification exam, this practice test question will set you up for success. Test writers anticipate possible answers based on the details in the question. They will wave those “juicy answers” right under your nose. Your job is to weed through the particulars, pluck out the most important elements and choose the BEST answer.
Answer 1 is incorrect. 8.04% chose this answer. “Adherence to the diabetes self-care plan takes time.” Under the umbrella of a person-centered care approach, the terms “adherence” and “compliance” are outdated concepts that are no longer used. For example, if we say that TR is adherent, it means that they are following the provider’s instructions instead of being an active participant in care. This person-centered approach engages the individual in the decision-making process and self-care plan.
Answer 2 is incorrect. 24.67% of you chose this answer. “Motivating individuals to engage in their self-management is the first step.” This is a juicy answer that sounds really good. However, it is not a realistic expectation to believe we can motivate people to make changes in their self-management. We can provide coaching and support, but ultimately, the person with diabetes needs to find their own motivation to make slow and steady behavior change. For this reason, this approach is not considered a person-centered approach.
Answer 3 is incorrect. 5.42% of respondents chose this. “Adult learners do best when provided a step-by the-step demonstration.” This answer is partially correct. Adult learners do apply their previous knowledge to the task at hand. However, more importantly than just observing, adult learners need to participate in the learning activity and have “hand’s on” practice to solidify their knowledge.
Finally, Answer 4 is correct. 61.87% chose this answer. “Creating mutual agreement on the plan for next steps.” YES, this is the BEST PERSON-CENTERED ANSWER. This approach invites the person with diabetes to fully participate in determining their needs and goals while making plans for the future in collaboration with the provider.
We hope you appreciate this week’s rationale! Thank you so much for taking the time to answer our Question of the Week and participate in this fun learning activity!
Join us at our
Virtual DiabetesEd Training Conference

Your team is invited to our Virtual DiabetesEd™ Training Conference! Set your team apart and prepare for diabetes certification!
Join this state-of-the-art conference taught by content experts, Diana Isaacs, PharmD, BCPS, BCACP, BC-ADM, CDCES, Beverly Thomassian RN, MPH, CDCES, BC-ADM, and Ashley LaBrier who are passionate about improving diabetes care.
Group discounts are available!*
All hours earned count toward your CDCES Accreditation Information
Now introducing payment plans!
Many of you have requested to set up payment plans for your orders and we have found a great solution for this! During checkout, on the payment page, you can now select “Shop Pay” to pay in 3 installments instead of just one payment.
Sign up for Diabetes Blog Bytes – we post one daily Blog Byte from Monday to Friday. And of course, Tuesday is our Question of the Week. It’s Informative and FREE! Sign up below!
The use of DES products does not guarantee the successful passage of the CDCES exam. CBDCE does not endorse any preparator