Rationale of the Week | Low blood sugars and Beer

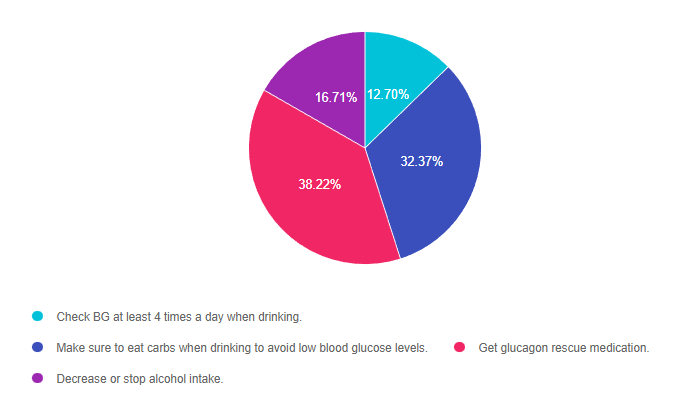
For last week’s practice question, we quizzed participants on low blood sugars and beer. 38% of respondents chose the best answer. We want to clarify and share this important information, so you can pass it on to people living with diabetes and your colleagues, plus prepare for exam success!
Before we start though, if you don’t want any spoilers and haven’t tried the question yet, you can answer it below: Answer Question
Question:
JL is 19 and has type 1 diabetes, drinks a “few beers” on the weekends with their college friends. JL uses an insulin pump, but mostly relies of fingerstick checks to monitor blood sugars. According to their log, JL experienced a few low blood glucose levels the past weekend of 62, 49, and 51.
Based on the ADA Standards, what is the most important recommendation for JL?
Answer Choices:
- Check BG at least 4 times a day when drinking.
- Make sure to eat carbs when drinking to avoid low blood glucose levels.
- Get glucagon rescue medication.
- Decrease or stop alcohol intake.
Getting to the Best Answer
Answer 1 is incorrect. 12.70% chose this answer, “Check BG at least 4 times a day when drinking.” This is a juicy answer. Although monitoring will help JL detect low blood sugars, it doesn’t necessarily translate into taking action to prevent or treat these frequent bouts of level 2 hypoglycemia.
Answer 2 is incorrect. 32.37% of you chose this answer, “Make sure to eat carbs when drinking to avoid low blood glucose levels.” This is another juicy answer and a solid recommendation. For people with type 1 who experience hypoglycemia when drinking alcohol, eating 15gms of carb along with each alcohol serving can help maintain glucose levels. However, this answer is not based on the ADA Standards of Care.
Answer 3 is correct. 38.22% of respondents chose this answer, “Get glucagon rescue medication.” This is the BEST answer. According to the ADA’s Standard 6 on Glycemic Targets, “6.12 Glucagon should be prescribed for all individuals at increased risk of level 2 or 3 hypoglycemia, so that it is available should it be needed”. JL is experiencing Level 2 hypoglycemia with glucose levels dropping to 49 and 51. (see image from Glucagon PocketCard to right for Hypo Levels). While prevention of hypoglycemia is the long term goal, in the short term we need to make sure JL has access to a glucagon rescue med and that their significant others are trained on how to administer this life saving glucose booster.
Finally, Answer 4 is incorrect. 16.71% chose this answer, “Decrease or stop alcohol intake.” While we might want to have a conversation about alcohol and safety, the ADA Standards allow for 1 alcohol serving a day for women and 2 alcohol servings a day for men. In this situation, we might want to discuss adjusting insulin dosing and carbohydrate intake to prevent future bouts of hypoglycemia. However, for safety sake, JL will need a glucagon rescue med prescribed in case of a severe low blood glucose.
Thank you so much for reading this “Rationale of the Week”. For more information on this topic, we encourage you to join our Online Courses and Virtual DiabetesEd Training Program.
Preparing for Diabetes Certification Exam?
It’s not too late to enroll in our Level 3 – Boot Camp 2023
Level 3 | DiabetesEd Specialist Boot Camp | 12+ CEs

Can’t join all the sessions live? No problem. Your registration guarantees you access to the recorded lectures for a full year.
This bundle is specifically designed for healthcare professionals who are studying for the Board Certified in Advanced Diabetes Management (BC-ADM) or the Certified Diabetes Care and Education Specialist (CDCES) certification exam.
Intended Audience: This library of critical information is designed for individuals or groups of diabetes specialists, including RNs, RDs, Pharmacists, Nurse Practitioners, Clinical Nurse Specialists, Physician Assistants, and other health care providers interested in staying up to date on current practices of care for people with diabetes and preparing for the BC-ADM or the CDCES certification Exam.
2023 Webinar Updates
- Recorded & Ready to Watch – Class 1 – Diabetes – Not Just Hyperglycemia 1.75 CEs
- Recorded & Ready to Watch – Class 2 – Standards of Care & Cardiovascular Goals 1.8 CEs
- Recorded & Ready to Watch – Class 3 – Meds for Type 2 – What you need to know 1.5
- February 16, 2023 – Class 4 – Insulin Therapy – From Basal/Bolus to Pattern Management 1.5 CEs
- February 21, 2023 – Class 5 – Insulin Intensive – Monitoring, Sick Days, Lower
- February 23, 2023 – Class 6 – Exercise and Medical Nutrition Therapy 1.5 CEs
- February 28, 2023 – Class 7 – Screening, Prevention, and Treatment of Microvascular Complications
- March 2, 2023 – Class 8 – Coping and Behavior Change 1.5 CEs
- March 9, 2023 – Class 9 – Test-Taking Coach Session (48 Questions) No CE
All hours earned count toward your CDCES Accreditation Information
Sign up for Diabetes Blog Bytes – we post one daily Blog Byte from Monday to Friday. And of course, Tuesday is our Question of the Week. It’s Informative and FREE! Sign up below!
The use of DES products does not guarantee the successful passage of the CDCES exam. CBDCE does not endorse any preparatory or review materials for the CDCES exam, except for those published by CBDCE.
Rationale of the Week | Safe for Surgery?

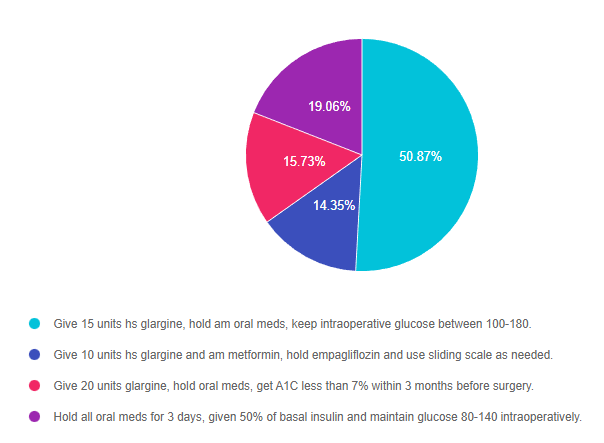
For last week’s practice question, we quizzed participants on the best action for a safe surgery. 51% of respondents chose the best answer. We want to clarify and share this important information, so you can pass it on to people living with diabetes and your colleagues, plus prepare for exam success!
Before we start though, if you don’t want any spoilers and haven’t tried the question yet, you can answer it below: Answer Question
Question:
PZ is having elective surgery in the morning. Diabetes medications include 20 units glargine (Semglee) at hs, metformin BID and empagliflozin (Jardiance).
According to 2023 ADA Standards, what are the best actions for a safe surgery?
Answer Choices:
- Give 15 units hs glargine, hold am oral meds, keep intraoperative glucose between 100-180.
- Give 10 units hs glargine and am metformin, hold empagliflozin and use sliding scale as needed.
- Give 20 units glargine, hold oral meds, get A1C less than 7% within 3 months before surgery.
- Hold all oral meds for 3 days, given 50% of basal insulin and maintain glucose 80-140 intraoperatively.
Getting to the Best Answer
Answer 1 is correct. 50.87% chose this answer, “Give 15 units hs glargine, hold am oral meds, keep intraoperative glucose between 100-180.” YES, GREAT JOB! The ADA Standard 16 on Hospitalization has been updated with new perioperative glucose goals and preop medication adjustments. To prevent intraoperative hypoglycemia, the glucose goal was increased to 100-180. In addition, they recommend reducing basal insulin by 20-25% the night before surgery and holding all oral meds the morning of surgery. SGLT-2s are held for 3-4 days before surgery to decrease risk of DKA in the perioperative period. In this vignette, we reduced PZ’s basal insulin from 20 units to 15 units (25% decrease) and held all oral meds the morning of surgery. In addition, the 2023 Standards recommend achieving an A1C less than 8% before elective surgeries. Since about 20% of people undergoing surgery have diabetes, these guidelines are super helpful and important to improve post surgical outcomes.
Answer 2 is incorrect. 14.35% of you chose this answer, “Give 10 units hs glargine and am metformin, hold empagliflozin and use sliding scale as needed.” This is answer is close and partly correct, because it recommends holding the oral medications. However, the first part of the answer is incorrect since a basal insulin reduction of 50% is too aggressive. People release lots of counterregulatory hormones during surgery, so they still need at least 75% of their usual basal insulin dose to prevent intraoperative hyperglycemia. If the person uses NPH basal insulin, they would need to reduce the evening dose by 50%. Since about 20% of people undergoing surgery have diabetes, these guidelines are super helpful and important to improve post surgical outcomes.
Answer 3 is incorrect. 15.73% of respondents chose this answer, “Give 20 units glargine, hold oral meds, get A1C less than 7% within 3 months before surgery.” This is answer is close and partly correct, because it recommends holding the oral medications. However, the first part of the answer is incorrect since the basal insulin needs to be reduced by 20-25% to prevent intraoperative hypoglycemia. In addition, the 2023 Standards recommend achieving an A1C less than 8% (not 7%) before elective surgeries. Since about 20% of people undergoing surgery have diabetes, these guidelines are super helpful and important to improve post surgical outcomes.
Finally, Answer 4 is incorrect. 19.06% chose this answer, “Hold all oral meds for 3 days, given 50% of basal insulin and maintain glucose 80-140 intraoperatively.” This entire answer is incorrect for the following reasons. Oral meds are held the day of surgery, except for SGLT2i’s, which are held for 3-4 days pre-op. As far as basal insulin, the ADA guidelines recommend giving 75-80% of usual dose, except for NPH insulin, which is reduced by 50%. Lastly, the intraoperative glucose target is 100 -180. Since about 20% of people undergoing surgery have diabetes, these guidelines are super helpful and important to improve post surgical outcomes.
Thank you so much for reading this “Rationale of the Week”.
We invite you to join Coach Beverly on May 30, 2023 – Hospital and Hyperglycemia 1.5 CEs
Want to learn more about this question? Enroll in our
Level 2 | ADA Standards of Care CE Course | 2.0 CEs
2023 Update is Recorded & Ready to Watch!
This course, updated annually, is an essential review for anyone in the field of diabetes. Join Coach Beverly as she summarizes the 2023 updates to the American Diabetes Association’s Standards of Medical Care in Diabetes and provides critical teaching points and content for healthcare professionals involved in diabetes care and education.
Objectives:
- List significant changes and updates to the 2023 ADA Standards of Medical Care.
- State 3 updates on new blood pressure and lipid goals.
- Identify 5 key elements of the position statement.
- Discuss how to apply the Standards in the clinical setting and in preparation for exam success.
Intended Audience: This course is a knowledge-based activity designed for individuals or groups of diabetes professionals, including RNs, RDs, Pharmacists, Nurse Practitioners, Clinical Nurse Specialists, Physician Assistants, and other health care providers interested in staying up to date on current practices of care for people with prediabetes, diabetes, and other related conditions.
Don’t worry if you can’t make it live. Your registration guarantees access to the recorded version in the Online University.
All hours earned count toward your CDCES Accreditation Information
Preparing for Diabetes Certification Exam? Enroll in our Level 3 – Boot Camp 2023 Updates
Level 3 | DiabetesEd Specialist Boot Camp | 12+ CEs

Can’t join all the sessions live? No problem. Your registration guarantees you access to the recorded lectures for a full year.
This bundle is specifically designed for healthcare professionals who are studying for the Board Certified in Advanced Diabetes Management (BC-ADM) or the Certified Diabetes Care and Education Specialist (CDCES) certification exam.
Intended Audience: This library of critical information is designed for individuals or groups of diabetes specialists, including RNs, RDs, Pharmacists, Nurse Practitioners, Clinical Nurse Specialists, Physician Assistants, and other health care providers interested in staying up to date on current practices of care for people with diabetes and preparing for the BC-ADM or the CDCES certification Exam.
2023 Webinar Updates
- Recorded & Ready to Watch – Class 1 – Diabetes – Not Just Hyperglycemia 1.75 CEs
- February 9, 2023 – Class 2 – Standards of Care & Cardiovascular Goals 1.8 CEs
- February 14, 2023 – Class 3 – Meds for Type 2 – What you need to know 1.5
- February 16, 2023 – Class 4 – Insulin Therapy – From Basal/Bolus to Pattern Management 1.5 CEs
- February 21, 2023 – Class 5 – Insulin Intensive – Monitoring, Sick Days, Lower
- February 23, 2023 – Class 6 – Exercise and Medical Nutrition Therapy 1.5 CEs
- February 28, 2023 – Class 7 – Screening, Prevention, and Treatment of Microvascular Complications
- March 2, 2023 – Class 8 – Coping and Behavior Change 1.5 CEs
- March 9, 2023 – Class 9 – Test-Taking Coach Session (48 Questions) No CE
All hours earned count toward your CDCES Accreditation Information
Sign up for Diabetes Blog Bytes – we post one daily Blog Byte from Monday to Friday. And of course, Tuesday is our Question of the Week. It’s Informative and FREE! Sign up below!
The use of DES products does not guarantee the successful passage of the CDCES exam. CBDCE does not endorse any preparatory or review materials for the CDCES exam, except for those published by CBDCE.
Rationale of the Week | Diabetes and NASH, what is the link?

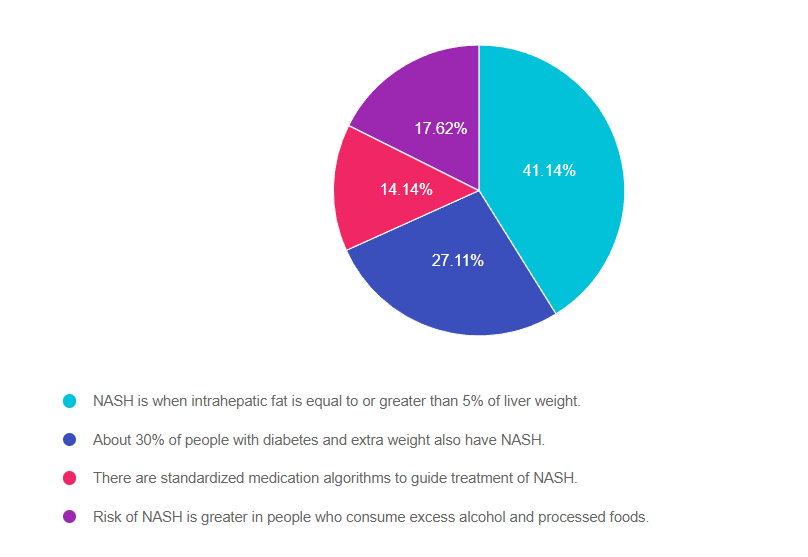
For last week’s practice question, we quizzed participants on Diabetes and NASH. 41% of respondents chose the best answer. We want to clarify and share this important information, so you can pass it on to people living with diabetes and your colleagues, plus prepare for exam success!
Before we start though, if you don’t want any spoilers and haven’t tried the question yet, you can answer it below: Answer Question
Question:
The provider referred RT, a 72-year-old with type 2 diabetes and non-alcoholic fatty steatohepatitis (NASH), for an appointment with the diabetes care and education specialist. RT is frightened because their brother died of liver cancer.
Which of the following is the most accurate statement regarding NASH and diabetes?
Answer Choices:
- NASH is when intrahepatic fat is equal to or greater than 5% of liver weight.
- About 30% of people with diabetes and extra weight also have NASH.
- There are standardized medication algorithms to guide the treatment of NASH.
- Risk of NASH is greater in people who consume excess alcohol and processed foods.
Getting to the Best Answer
Answer 1 is correct. 41.14% chose this answer, “NASH is when intrahepatic fat is equal to or greater than 5% of liver weight.” GREAT JOB! According to ADA Standard 4, “NASH is defined histologically as having more than 5% hepatic steatosis and associated with inflammation and hepatocyte injury (hepatocyte ballooning), with or without evidence of liver fibrosis”.
Answer 2 is incorrect. 27.11% of you chose this answer, “About 30% of people with diabetes and extra weight also have NASH.” This is a juicy answer, but it is an underestimate of the current problem. Recent studies in adults in the U.S. estimate that more than 70% of people with type 2 diabetes have non alcoholic fatty liver disease (NAFLD). The more serious, steatohepatitis, is estimated to affect more than 50% of people with type 2 diabetes with NAFLD and it appears to be a driver for the development of fibrosis.
Answer 3 is incorrect. 14.14% of respondents chose this answer, “There are standardized medication algorithms to guide the treatment of NASH.” According to ADA Standard 4, at present, there are no FDA-approved drugs for the treatment of NASH. Therefore, treatment for people with type 2 diabetes and NASH is centered on the dual purpose of treating hyperglycemia and weight loss. Pioglitazone and some glucagon-like peptide 1 receptor agonists (GLP-1 RAs) have been shown to be effective to treat steatohepatitis, may slow fibrosis progression, and decrease cardiovascular disease.
Finally, Answer 4 is incorrect. 17.62% chose this answer, “Risk of NASH is greater in people who consume excess alcohol and processed foods.” Nonalcoholic steatohepatitis [NASH] indicates liver inflammation in the absence of ongoing or recent consumption of significant amounts of alcohol (defined as ingestion of >21 standard drinks per week in men and >14 standard drinks per week in women over a 2-year period preceding evaluation) or the presence of other secondary causes of fatty liver disease. NASH is not a result of excess alcohol intake and is usually associated with genetics, body weight and insulin resistance.
Thank you so much for reading this “Rationale of the Week”.
We also invite you to join our Online Courses for more information (see info below)
Hope you can join our Diabetes Boot Camp in February and our other Level 2 Courses.
Preparing for Diabetes Certification Exam? Enroll in our Level 3 – Boot Camp 2023 Updates
Level 3 | DiabetesEd Specialist Boot Camp | 12+ CEs

Can’t join all the sessions live? No problem. Your registration guarantees you access to the recorded lectures for a full year.
This bundle is specifically designed for healthcare professionals who are studying for the Board Certified in Advanced Diabetes Management (BC-ADM) or the Certified Diabetes Care and Education Specialist (CDCES) certification exam.
Intended Audience: This library of critical information is designed for individuals or groups of diabetes specialists, including RNs, RDs, Pharmacists, Nurse Practitioners, Clinical Nurse Specialists, Physician Assistants, and other health care providers interested in staying up to date on current practices of care for people with diabetes and preparing for the BC-ADM or the CDCES certification Exam.
2023 Webinar Updates
- February 7, 2023 – Class 1 – Diabetes – Not Just Hyperglycemia 1.75 CEs
- February 9, 2023 – Class 2 – Standards of Care & Cardiovascular Goals 1.8 CEs
- February 14, 2023 – Class 3 – Meds for Type 2 – What you need to know 1.5
- February 16, 2023 – Class 4 – Insulin Therapy – From Basal/Bolus to Pattern Management 1.5 CEs
- February 21, 2023 – Class 5 – Insulin Intensive – Monitoring, Sick Days, Lower
- February 23, 2023 – Class 6 – Exercise and Medical Nutrition Therapy 1.5 CEs
- February 28, 2023 – Class 7 – Screening, Prevention, and Treatment of Microvascular Complications
- March 2, 2023 – Class 8 – Coping and Behavior Change 1.5 CEs
- March 9, 2023 – Class 9 – Test-Taking Coach Session (48 Questions) No CE
All hours earned count toward your CDCES Accreditation Information
Sign up for Diabetes Blog Bytes – we post one daily Blog Byte from Monday to Friday. And of course, Tuesday is our Question of the Week. It’s Informative and FREE! Sign up below!
The use of DES products does not guarantee the successful passage of the CDCES exam. CBDCE does not endorse any preparatory or review materials for the CDCES exam, except for those published by CBDCE.
Rationale of the Week | What is the Right LDL Target for RZ?

For last week’s practice question, we quizzed participants on what is the right LDL target. 37% of respondents chose the best answer. We want to clarify and share this important information, so you can pass it on to people living with diabetes and your colleagues, plus prepare for exam success!
Before we start though, if you don’t want any spoilers and haven’t tried the question yet, you can answer it below: Answer Question
Question:
RZ is 47 years old with type 2 diabetes and hypertension with a UACR of 199 mg/g. RZ takes metformin 1000 mg BID, plus lisinopril 20mg daily. RZ most recent LDL Cholesterol was 130 mg/dL. The provider writes an order for DASH meal planning education and initiation of atorvastatin 40mg.
Based on the most recent ADA Standards, what is the LDL Cholesterol target for RZ?
Answer Choices:
- LDL less than 100 mg/dL.
- Lower LDL by 30%.
- LDL target of 65 mg/dL or less.
- Determine LDL target based on ASCVD calculations.
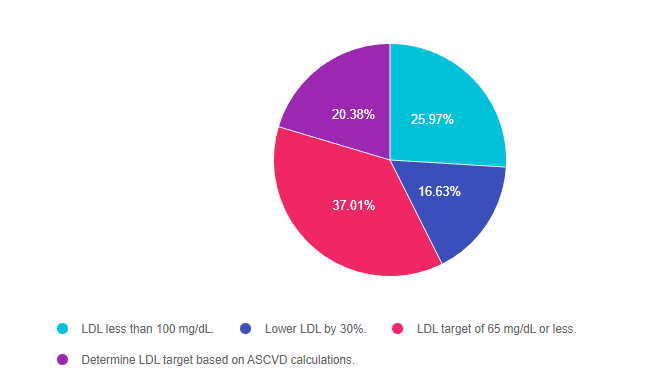
Getting to the Best Answer
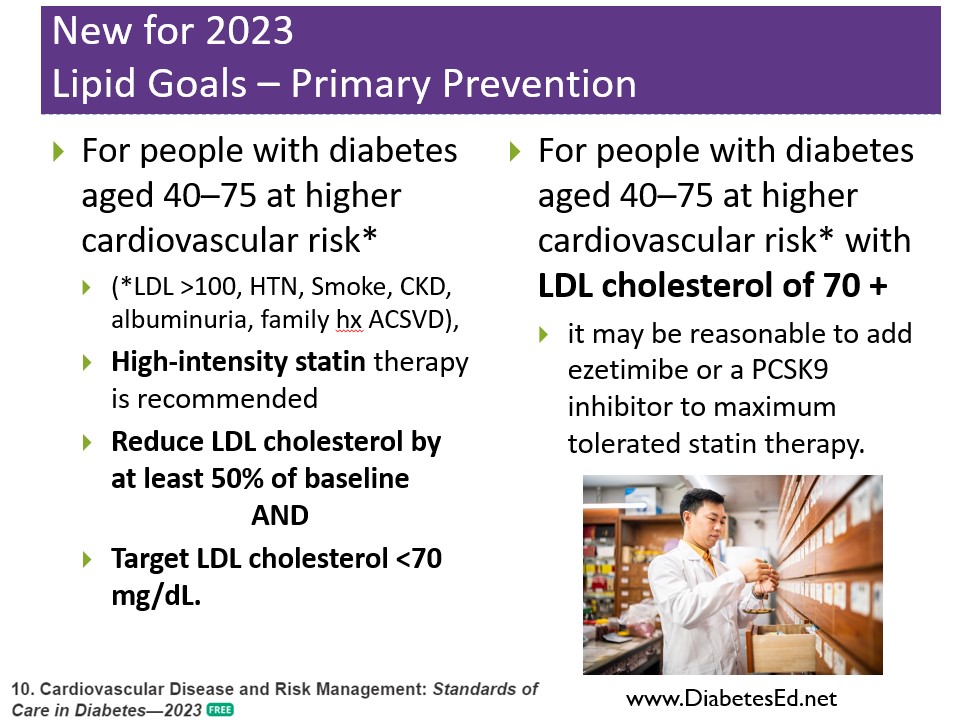
Answer 1 is incorrect. 25.97% chose this answer, “LDL less than 100 mg/dL.” This is a juicy answer since it is the OLD LDL goal from several years ago. But the new 2023 lipid guidelines have even more intense goals for high-risk individuals. Since RZ has diabetes, hypertension, and albuminuria (UACR >30mg/g), they have an elevated risk of ASCVD. Given their risk status, the 2023 guidelines recommend reducing LDL by at least 50% of baseline and target LDL cholesterol to less than 70 mg/dL (see slide below).
Answer 2 is incorrect. 16.63% of you chose this answer, “Lower LDL by 30%.” Another juicy answer. Given RZ’s risk status, the 2023 guidelines recommend reducing LDL by at least 50% of baseline and target LDL cholesterol to less than 70 mg/dL. (see slide below).
Answer 3 is correct. 37.01% of respondents chose this answer, “LDL target of 65 mg/dL or less.” GREAT JOB! Since RZ has diabetes, hypertension, and albuminuria (UACR >30mg/g), they have an elevated risk of ASCVD. Given their risk status, the 2023 guidelines recommend reducing LDL by at least 50% of baseline and target LDL cholesterol to less than 70 mg/dL. Since RZ’s current LDL is 130, the goal is to reduce the LDL by at least 50% (LDL of 65mg/dL) AND less than 70 mg/dL by using a high-intensity statin and lifestyle therapy, (see slide below).
Finally, Answer 4 is incorrect. 20.38% chose this answer, “Determine LDL target based on ASCVD calculations.” Although this information would be helpful, it wouldn’t change the lipid goals. Given their risk status, the 2023 guidelines recommend reducing LDL by at least 50% of baseline and target LDL cholesterol to less than 70 mg/dL, (see slide below).
Thank you so much for reading this “Rationale of the Week”.
We also invite you to join our Online Courses for more information (see info below)
Hope you can join our ADA Standards of Care Webinar Update in February and our other Level 2 Courses.
Want to learn more about this question? Join us for our
Level 2 | ADA Standards of Care CE Course | 2.0 CEs
Updates air live between Feb. 2, 2023, at 11:30 am PST
This course, updated annually, is an essential review for anyone in the field of diabetes. Join Coach Beverly as she summarizes the 2023 updates to the American Diabetes Association’s Standards of Medical Care in Diabetes and provides critical teaching points and content for healthcare professionals involved in diabetes care and education.
Objectives:
- List significant changes and updates to the 2023 ADA Standards of Medical Care.
- State 3 updates on new blood pressure and lipid goals.
- Identify 5 key elements of the position statement.
- Discuss how to apply the Standards in the clinical setting and in preparation for exam success.
Intended Audience: This course is a knowledge-based activity designed for individuals or groups of diabetes professionals, including RNs, RDs, Pharmacists, Nurse Practitioners, Clinical Nurse Specialists, Physician Assistants, and other health care providers interested in staying up to date on current practices of care for people with prediabetes, diabetes and other related conditions.
Don’t worry if you can’t make it live. Your registration guarantees access to the recorded version in the Online University.
All hours earned count toward your CDCES Accreditation Information
Preparing for Diabetes Certification Exam? Enroll in our Level 3 – Boot Camp 2023 Updates
Level 3 | DiabetesEd Specialist Boot Camp | 12+ CEs

Can’t join all the sessions live? No problem. Your registration guarantees you access to the recorded lectures for a full year.
This bundle is specifically designed for healthcare professionals who are studying for the Board Certified in Advanced Diabetes Management (BC-ADM) or the Certified Diabetes Care and Education Specialist (CDCES) certification exam.
Intended Audience: This library of critical information is designed for individuals or groups of diabetes specialists, including RNs, RDs, Pharmacists, Nurse Practitioners, Clinical Nurse Specialists, Physician Assistants, and other health care providers interested in staying up to date on current practices of care for people with diabetes and preparing for the BC-ADM or the CDCES certification Exam.
2023 Webinar Updates
- February 7, 2023 – Class 1 – Diabetes – Not Just Hyperglycemia 1.75 CEs
- February 9, 2023 – Class 2 – Standards of Care & Cardiovascular Goals 1.8 CEs
- February 14, 2023 – Class 3 – Meds for Type 2 – What you need to know 1.5
- February 16, 2023 – Class 4 – Insulin Therapy – From Basal/Bolus to Pattern Management 1.5 CEs
- February 21, 2023 – Class 5 – Insulin Intensive – Monitoring, Sick Days, Lower
- February 23, 2023 – Class 6 – Exercise and Medical Nutrition Therapy 1.5 CEs
- February 28, 2023 – Class 7 – Screening, Prevention, and Treatment of Microvascular Complications
- March 2, 2023 – Class 8 – Coping and Behavior Change 1.5 CEs
- March 9, 2023 – Class 9 – Test-Taking Coach Session (48 Questions) No CE
All hours earned count toward your CDCES Accreditation Information
Sign up for Diabetes Blog Bytes – we post one daily Blog Byte from Monday to Friday. And of course, Tuesday is our Question of the Week. It’s Informative and FREE! Sign up below!
The use of DES products does not guarantee the successful passage of the CDCES exam. CBDCE does not endorse any preparatory or review materials for the CDCES exam, except for those published by CBDCE.
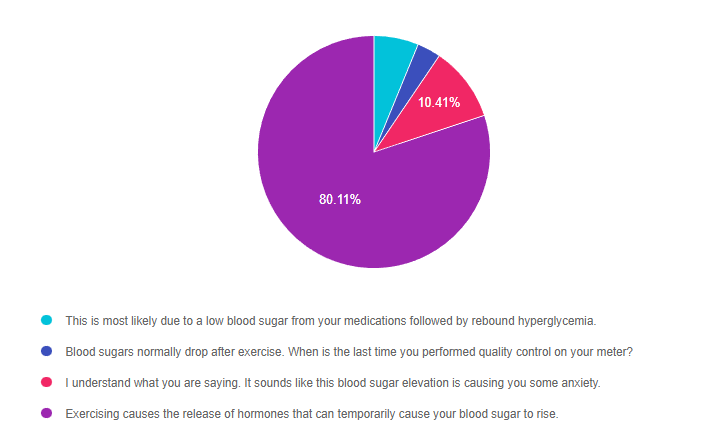
Rationale of the Week | Why is post-exercise glucose spiking?

For last week’s practice question, we quizzed participants on why glucose is spiking after exercise. 80% of respondents chose the best answer. We want to clarify and share this important information, so you can pass it on to people living with diabetes and your colleagues, plus prepare for exam success!
Before we start though, if you don’t want any spoilers and haven’t tried the question yet, you can answer it below: Answer Question
Question:
JR is 42 years old with type 2 diabetes and has worked up to brisk walking for 30 minutes on most days. JR has an A1C of 6.7% and takes an SGLT-2, metformin, and lovastatin along with trying to eat healthfully. JR decided to check blood sugars an hour after exercise and was surprised to see post-exercise blood glucose in the 180’s on two different days. JR asks you why their blood glucose actually rises after exercise.
What is the diabetes specialist’s best response?
Answer Choices:
- This is most likely due to a low blood sugar from your medications followed by rebound hyperglycemia.
- Blood sugars normally drop after exercise. When is the last time you performed quality control on your meter?
- I understand what you are saying. It sounds like this blood sugar elevation is causing you some anxiety.
- Exercising causes the release of hormones that can temporarily cause your blood sugar to rise.
Getting to the Best Answer
Answer 1 is incorrect. 6.19% chose this answer, “This is most likely due to a low blood sugar from your medications followed by rebound hyperglycemia.” This answer is tempting, but not accurate. Since JR’s only diabetes medication include metformin and a SGLT-2 inhibitor, they are not at risk for low blood sugar. Low blood sugar is only associated with sulfonylureas, meglitinides and insulin therapy.
Answer 2 is incorrect. 3.29% of you chose this answer, “Blood sugars normally drop after exercise. When is the last time you performed quality control on your meter?” In this situation, exercise can decrease hours after exercise, but usually increases immediately after exercise. Which means, JR doesn’t need to perform quality control on their glucose meter, since it is accurately reflecting blood sugar trends.
Answer 3 is incorrect. 10.41% of respondents chose this answer, “I understand what you are saying. It sounds like this blood sugar elevation is causing you some anxiety.” Although, this is a very compassionate response, it does not answer the question JR is asking, “why does my blood sugar go up after exercise?” For this reason, it is tempting, but not the best answer.
Finally, Answer 4 is correct. 80.11% chose this answer, “Exercising causes the release of hormones that can temporarily cause your blood sugar to rise.” YES, most of you chose the best answer. With exercise, counterregulatory or stress hormones are activated, which increases insulin resistance and causes blood glucose levels to temporarily rise to feed hungry muscles. This glucose rise is an expected temporary response and with time, blood sugars get back to baseline. GREAT JOB.
Thank you so much for reading this “Rationale of the Week”.
We also invite you to join our Online Courses for more information (see info below)
Hope you can join our ADA Standards of Care Webinar Update in February.
Want to learn more about this question? Enroll in our upcoming
Level 1 | Diabetes Fundamentals 2023 Updates | 9+ CEs
This bundle is specifically designed for healthcare professionals who want to learn more about diabetes fundamentals for their clinical practice or for those who are studying for the Certified Diabetes Care and Education Specialist (CDCES) exam.
Intended Audience: This library of critical information is designed for individuals or groups of diabetes specialists, including RNs, RDs, Pharmacists, Nurse Practitioners, Clinical Nurse Specialists, Physician Assistants, and other health care providers interested in staying up to date on current practices of care for people with diabetes and preparing for the CDCES Certification Exam.
2023 Webinar Updates
- Recorded & Ready to watch on-demand – Class 1 – Getting to the Nitty Gritty 1.5 CEs
- Recorded & Ready to watch on-demand – Class 2 – Nutrition and Exercise 1.5 CEs
- Recorded & Ready to watch on-demand – Class 3 – Meds Overview for Type 2 – 1.5 CEs
- January 19, 2023 – Class 4 – Insulin Therapy & Pattern Management 1.5 CEs
- January 24, 2023 – Class 5 – Goals of Care – 1.5 CEs
- January 26, 2023 – Class 6 – Hypoglycemia, Sick Days, Monitoring, Foot Care 1.5 CEs
All hours earned count toward your CDCES Accreditation Information
Want an overview of the new 2023 ADA Standards of Care in Diabetes?
Join us live on February 2, 2023, at 11:30 am PST for our
Level 2 | ADA Standards of Care 2023 Update | 2.0 CEs
This course, updated annually, is an essential review for anyone in the field of diabetes. Join Coach Beverly as she summarizes the 2023 updates to the American Diabetes Association’s Standards of Medical Care in Diabetes and provides critical teaching points and content for healthcare professionals involved in diabetes care and education.
All hours earned count toward your CDCES Accreditation Information
Sign up for Diabetes Blog Bytes – we post one daily Blog Byte from Monday to Friday. And of course, Tuesday is our Question of the Week. It’s Informative and FREE! Sign up below!
The use of DES products does not guarantee the successful passage of the CDCES exam. CBDCE does not endorse any preparatory or review materials for the CDCES exam, except for those published by CBDCE.
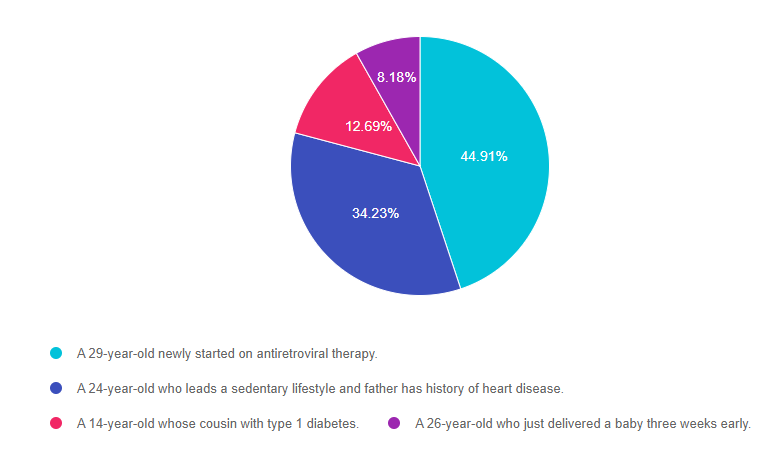
Rationale of the Week | Who has most diabetes risk based on 2023 Standards?

For last week’s practice question, we quizzed participants on who is most at risk of diabetes based on the new ADA Standards. 45% of respondents chose the best answer. We want to clarify and share this important information, so you can pass it on to people living with diabetes and your colleagues, plus prepare for exam success!
Before we start though, if you don’t want any spoilers and haven’t tried the question yet, you can answer it below: Answer Question
Question:
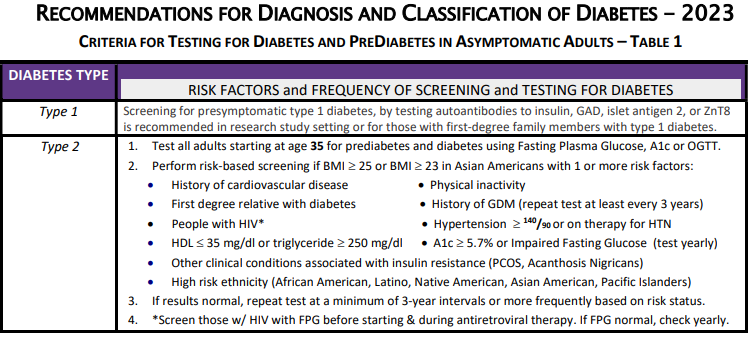
The clinic where JR works as a Diabetes Specialist wants to set up a screening program to identify people with undiagnosed prediabetes or diabetes based on risk status. According to the 2023 ADA Standards of Care, which of the following indicates that an individual is at increased risk of having prediabetes and diabetes and needs further testing?
Answer Choices:
- A 29-year-old newly started on antiretroviral therapy.
- A 24-year-old who leads a sedentary lifestyle and father has history of heart disease.
- A 14-year-old whose cousin with type 1 diabetes.
- A 26-year-old who just delivered a baby three weeks early.
Getting to the Best Answer
Answer 1 is correct. 44.91% chose the BEST answer, “A 29-year-old newly started on antiretroviral therapy.” GREAT JOB. A potential side effect of antiretroviral therapy, used to treat HIV, is the destruction of beta cells and resultant hyperglycemia. The ADA guidelines recommend screening blood sugars before starting antiretroviral therapy, during treatment and yearly. Of course, it is also important to alert the individual on antiretroviral therapy of the signs of hyperglycemia and ask them to report any signs right away. Please refer to our Diabetes Diagnosis and Screening Cheat Sheet for more information.
Answer 2 is incorrect. 34.23% of you chose this answer, “A 24-year-old who leads a sedentary lifestyle and father has history of heart disease.” Screening for prediabetes or diabetes starts at the age of 35 for everyone or for younger individuals with an elevated BMI and an additional risk factor. Since this person is under the age of 35 and we don’t know their weight, they wouldn’t meet the criteria for a high risk individual based on the information provided and the ADA Guidelines. Please refer to our Diabetes Diagnosis and Screening Cheat Sheet for more information.
Answer 3 is incorrect. 12.69% of respondents chose this answer, “A 14-year-old whose cousin with type 1 diabetes.” The ADA guidelines suggest screening individuals with a first-degree family members with type 1 diabetes. Since cousins aren’t considered first-degree relatives, this is not the best answer. However, JDRF has a Type 1 Screening Resource Page for those who are interested in being screened for type 1 diabetes. Please refer to our Diabetes Diagnosis and Screening Cheat Sheet for more information.
Finally, Answer 4 is incorrect. 8.18% chose this answer, “A 26-year-old who just delivered a baby three weeks early.” This answer is tempting, but does not match the ADA risk factors. A person who had gestational diabetes has a higher risk of future diabetes, but in this answer, there is no indication that the person had GDM or any blood sugar elevations. Delivering a baby early is not associated with increased diabetes risk. Please refer to our Diabetes Diagnosis and Screening Cheat Sheet for more information.
Thank you so much for reading this “Rationale of the Week”.
Please refer to our Diabetes Diagnosis and Screening Cheat Sheet for more information.
We also invite you to join our Online Courses for more information (see info below)
Hope you can join our ADA Standards of Care Webinar Update in February.
Want to learn more about this question? Enroll in our upcoming
Level 1 | Diabetes Fundamentals 2023 Updates | 9+ CEs
This bundle is specifically designed for healthcare professionals who want to learn more about diabetes fundamentals for their clinical practice or for those who are studying for the Certified Diabetes Care and Education Specialist (CDCES) exam.
Intended Audience: This library of critical information is designed for individuals or groups of diabetes specialists, including RNs, RDs, Pharmacists, Nurse Practitioners, Clinical Nurse Specialists, Physician Assistants, and other health care providers interested in staying up to date on current practices of care for people with diabetes and preparing for the CDCES Certification Exam.
2023 Webinar Updates
- January 10, 2023 – Class 1 – Getting to the Nitty Gritty 1.5 CEs
- January 12, 2023 – Class 2 – Nutrition and Exercise 1.5 CEs
- January 17, 2023 – Class 3 – Meds Overview for Type 2 – 1.5 CEs
- January 19, 2023 – Class 4 – Insulin Therapy & Pattern Management 1.5 CEs
- January 24, 2023 – Class 5 – Goals of Care – 1.5 CEs
- January 26, 2023 – Class 6 – Hypoglycemia, Sick Days, Monitoring, Foot Care 1.5 CEs
All hours earned count toward your CDCES Accreditation Information
Want an overview of the new 2023 ADA Standards of Care in Diabetes?
Join us live on February 2, 2023, at 11:30 am PST for our
Level 2 | ADA Standards of Care 2023 Update | 2.0 CEs
This course, updated annually, is an essential review for anyone in the field of diabetes. Join Coach Beverly as she summarizes the 2023 updates to the American Diabetes Association’s Standards of Medical Care in Diabetes and provides critical teaching points and content for healthcare professionals involved in diabetes care and education.
All hours earned count toward your CDCES Accreditation Information
Sign up for Diabetes Blog Bytes – we post one daily Blog Byte from Monday to Friday. And of course, Tuesday is our Question of the Week. It’s Informative and FREE! Sign up below!
The use of DES products does not guarantee the successful passage of the CDCES exam. CBDCE does not endorse any preparatory or review materials for the CDCES exam, except for those published by CBDCE.
Rationale of the Week | How long are these insulin pens good for?

For last week’s practice question, we quizzed participants on insulin storage guidelines. 55% of respondents chose the best answer. We want to clarify and share this important information, so you can pass it on to people living with diabetes and your colleagues, plus prepare for exam success!
Before we start though, if you don’t want any spoilers and haven’t tried the question yet, you can answer it below: Answer Question
Question:
JR has a bunch of insulin pens at home and is wondering if they are still good to use. Most of the unopened insulin pens are stored in the fridge, but JR has 2 degludec (Tresiba) pens that they left out of the refrigerator by accident. They ask you if they are still good. What is the most accurate response for the shelf life of degludec (Tresiba) pens stored at room temperature of up to 86 degrees Fahrenheit?
Answer Choices:
- In general, insulin pens expire after 10-14 days at room temperature.
- Insulin kept for more than 28 days at room temperature needs to be discarded.
- JR can put the degludec (Tresiba) back in the refrigerator and use it until the expiration date.
- Degludec (Tresiba) can be safely stored at room temperature for up to 56 days.
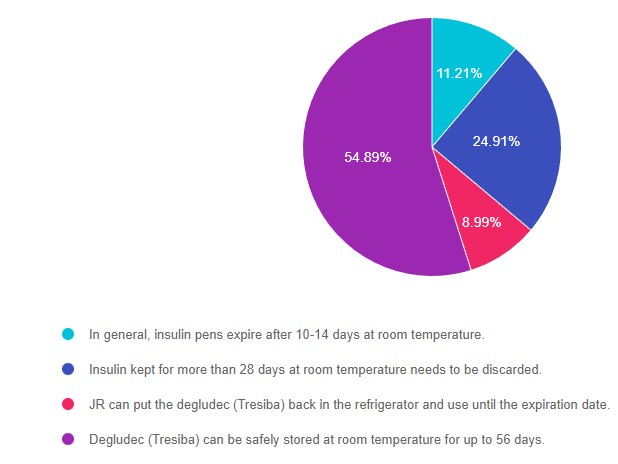
Getting to the Best Answer
- In general, insulin pens expire after 10-14 days at room temperature. (incorrect) 11% of respondents chose this juicy answer. However, degludec has one of the longest shelf lives at room temperature due to its pharmacokinetics. NPH and premixed insulin like 70/30 insulins have a shorter shelf life of 10-14 days. You can refer to our Insulin Storage Guidelines or package inserts for more information.
- Insulin kept for more than 28 days at room temperature needs to be discarded. (incorrect) About 25% of respondents chose this answer. Most bolus insulins have a shelf life of about 28 days whether they are stored in an insulin pen or vial. But many basal and concentrated insulins have a longer shelf life. NPH and premixed insulin like 70/30 insulins have a shorter shelf life of 10-14 days. Given the cost of insulin, this is important information to share with people living with diabetes, so they are aware of accurate insulin storage guidelines. You can refer to our Insulin Storage Guidelines or package inserts for more information.
- JR can put the degludec (Tresiba) back in the refrigerator and use it until the expiration date. (incorrect) 9% of respondents chose this answer, however, it is not an accurate answer. Once insulin is left out at room temperature, the clock starts ticking and with time, the potency of the insulin diminishes. For insulin degludec, the shelf life is 56 days outside of the refrigerator. If JR isn’t sure how long the insulin has been sitting out, they can look at the box Rx label or contact their pharmacy and find out what day the insulin was dispensed. You can refer to our Insulin Storage Guidelines or package inserts for more information.
- Degludec (Tresiba) can be safely stored at room temperature for up to 56 days. (correct). YES, this is the BEST answer and 55% of you chose this answer. Degludec along with Toujeo (Lantus U-300) can both be stored at room temperature for up to 56 days. You can refer to our Insulin Storage Guidelines or package inserts for more information.
Practical Clinical Pointers: Of course, these are general storage guidelines and if people using insulin notice blood sugars climbing despite adequate insulin dosing, it can be a sign the insulin has lost its potency. Sometimes, people on a budget might decide to keep using insulin past the expiration date. In either case, we can advise individuals to switch to a new insulin vial or pen right away if they notice blood sugars unexplainably trending up.
Thank you so much for reading this “Rationale of the Week”.
Please refer to our Insulin Storage Guidelines or package inserts for more information. We also invite you to join our Online Courses for more information (see info below)
Hope you can join our ADA Standards of Care Webinar Update in February.
See below for info.
Want to learn more about this question? Join us for our
Level 2 | ADA Standards of Care CE Course | 2.0 CEs
Update airs live Feb. 2, 2023, at 11:30 am PST
This course, updated annually, is an essential review for anyone in the field of diabetes. Join Coach Beverly as she summarizes the 2023 updates to the American Diabetes Association’s Standards of Medical Care in Diabetes and provides critical teaching points and content for healthcare professionals involved in diabetes care and education.
Objectives:
- List significant changes and updates to the 2023 ADA Standards of Medical Care.
- State 3 updates on new blood pressure and lipid goals.
- Identify 5 key elements of the position statement.
- Discuss how to apply the Standards in the clinical setting and in preparation for exam success.
Intended Audience: This course is a knowledge-based activity designed for individuals or groups of diabetes professionals, including RNs, RDs, Pharmacists, Nurse Practitioners, Clinical Nurse Specialists, Physician Assistants, and other health care providers interested in staying up to date on current practices of care for people with prediabetes, diabetes and other related conditions.
Don’t worry if you can’t make it live. Your registration guarantees access to the recorded version in the Online University.
All hours earned count toward your CDCES Accreditation Information
Studying for the CDCES Exam? Enroll in our
CDCES Deluxe Prep Bundle | 30+ Online Courses + Bonus Items | 47 CEs
This bundle includes our CDCES Online Prep Bundle (featured above) plus the ADCES Review Guide – 5th Edition-Revised. The online bundle includes Level 1, Level 2, and Level 3 (Boot Camp), plus two bonus courses. The ADCES Review Guide offers over 480+ practice questions and is a fantastic independent study tool and comprehensive resource for the Diabetes Care and Education Specialist Exam.
Included in this bundle
- Level 1 focuses on the fundamentals and introduces each topic area for the exam.
- Level 2 deep dives into the ADA Standards of Care,
- Level 3 AKA Boot Camp is a more accelerated level that focuses on test simulation for finding the best answer to get you to the finish line of your study path.
- Technology Toolkit which gives information on pumps, sensors, and calculations,
- Test Taking Toolkit includes over 220 practice questions for test simulation plus a webinar where Coach Beverly provides test-taking tips based on her experience taking the certification exam six times.
- ADCES Review Guide for the Diabetes Care and Education Specialist Exam – 5th Edition – Revised – The ADCES Review Guide is a fantastic independent study tool and comprehensive resource for the Diabetes Care and Education Specialist Exam. This book includes 480 + multiple-choice questions and strategies for preparing for and taking the exam with an answer key with rationales for all questions!
- Medication PocketCard – Our four-sided medication accordion Pocketcards were designed by Coach Beverly Thomassian to assist in clinical practice and exam preparation.
- Tote Bag
Sign up for Diabetes Blog Bytes – we post one daily Blog Byte from Monday to Friday. And of course, Tuesday is our Question of the Week. It’s Informative and FREE! Sign up below!
The use of DES products does not guarantee the successful passage of the CDCES exam. CBDCE does not endorse any preparatory or review materials for the CDCES exam, except for those published by CBDCE.
Rationale of the Week | For New ADA 2023 Standards, how is Hypertension defined?
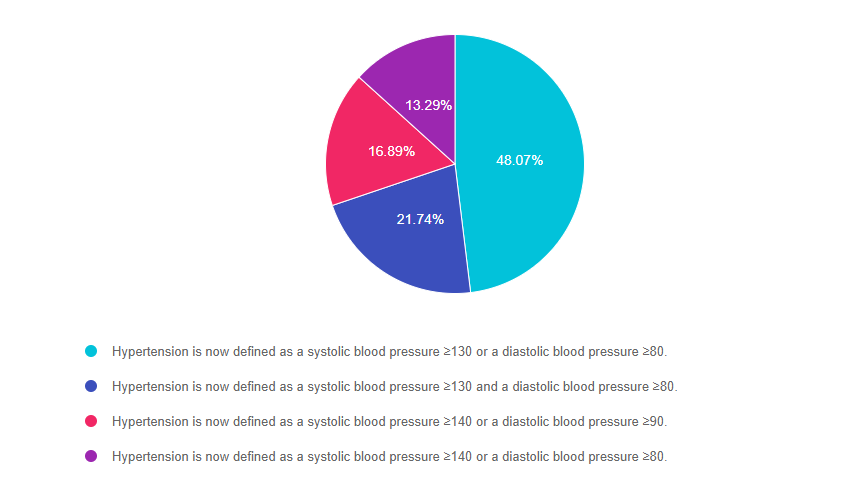
For last week’s practice question, we quizzed the new ADA 2023 standards on hypertension. 48% of respondents chose the best answer. We want to clarify and share this important information, so you can pass it on to people living with diabetes and your colleagues, plus prepare for exam success!
Before we start though, if you don’t want any spoilers and haven’t tried the question yet, you can answer it below: Answer Question
Question:
The new 2023 ADA Standards of Care are out, and they include several important clinical updates that are critical for our practice and certification exams.
What best represents the updated definition of hypertension in the 2023 Standards?
Answer Choices:
- Hypertension is now defined as a systolic blood pressure greater than or equal to 130 or a diastolic blood pressure greater than or equal to 80.
- Hypertension is now defined as a systolic blood pressure greater than or equal to 130 and a diastolic blood pressure greater than or equal to 80.
- Hypertension is now defined as a systolic blood pressure greater than or equal to 140 or a diastolic blood pressure greater than or equal to 90.
- Hypertension is now defined as a systolic blood pressure greater than or equal to 140 or a diastolic blood pressure greater than or equal to 80.
Getting to the Best Answer
Answer 1 is correct. 48.07% chose this BEST answer – GREAT JOB. According to Standard 10, Cardiovascular Disease and Risk Management, hypertension is now defined as a systolic blood pressure greater than or equal to 130 or a diastolic blood pressure greater than or equal to 80. This is in agreement with the definition of hypertension by the American College of Cardiology and American Heart Association. People with diabetes and hypertension qualify for antihypertensive drug therapy when the blood pressure is persistently elevated and is greater than or equal to 130/80. The on-treatment target blood pressure goal is less than 130/80, if it can be safely attained.
Answer 2 is incorrect. 21.74% of you chose this answer, “Hypertension is now defined as a systolic blood pressure greater than or equal to 130 and a diastolic blood pressure greater than or equal to 80.” This is so close to being the being the best answer, but it is not accurate. If either the diastolic or systolic pressure meet the cut-off, the person is considered to have a blood pressure reading that is above target.
Answer 3 is incorrect. 16.89% of respondents chose this answer, “Hypertension is now defined as a systolic blood pressure greater than or equal to 140 or a diastolic blood pressure greater than or equal to 90.” This was the definition of hypertension in the 2022 and older standards. The 2023 definition of hypertension is blood pressure equal to or greater than 130/80.
Finally, Answer 4 is incorrect. 13.29% chose this answer, “Hypertension is now defined as a systolic blood pressure greater than or equal to 140 or a diastolic blood pressure greater than or equal to 80.” This is a blending of hypertension definition from the 2022 and 2023 standards. The 2023 definition of hypertension is blood pressure equal to or greater than 130/80.
Thank you so much for reading this “Rationale of the Week”.
Want to learn more about this question? Join us for our
Level 2 | ADA Standards of Care CE Course
This course, updated annually, is an essential review for anyone in the field of diabetes. Join Coach Beverly as she summarizes the updates to the American Diabetes Association’s Standards of Medical Care in Diabetes and provides critical teaching points and content for healthcare professionals involved in diabetes care and education.
Objectives:
- List significant changes and updates to the ADA Standards of Medical Care.
- State 3 updates on new blood pressure and lipid goals.
- Identify 5 key elements of the position statement.
- Discuss how to apply the Standards in the clinical setting and in preparation for exam success.
Intended Audience: This course is a knowledge-based activity designed for individuals or groups of diabetes professionals, including RNs, RDs, Pharmacists, Nurse Practitioners, Clinical Nurse Specialists, Physician Assistants, and other health care providers interested in staying up to date on current practices of care for people with prediabetes, diabetes and other related conditions.
Don’t worry if you can’t make it live. Your registration guarantees access to the recorded version in the Online University.
All hours earned count toward your CDCES and BC-ADM Certification Accreditation Information








